No products in the cart.
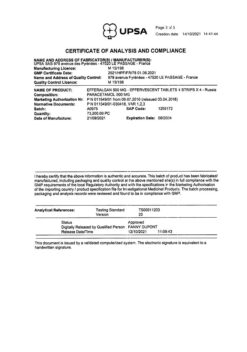
Paracetamol Reneval, tablets 500 mg 10 pcs
€1.48 €1.35
Description
Pharmacotherapeutic group: analgesic non-narcotic.
The ATX code: N02BE01
Pharmacological properties
Pharmacodynamics
Paracetamol has antipyretic and analgesic effects. A non-narcotic analgesic, it blocks cyclooxygenase (COX) I and II mainly in the central nervous system, affecting the centers of pain and thermoregulation. In inflamed tissues, cellular peroxidases neutralize the effect of paracetamol on COX, which explains the almost complete lack of anti-inflammatory effect. Since paracetamol has an extremely small effect on prostaglandin synthesis in periphytic tissues, it does not alter water-electrolyte metabolism and does not cause damage to the mucosa of the gastrointestinal tract. Thus, paracetamol is particularly suitable for patients with a history of gastrointestinal disease (such as patients with a history of gastrointestinal bleeding or elderly patients) or for patients taking concomitant medications when inhibition of peripheral prostaglandins may be undesirable.
Pharmacokinetics
Absorption
Absorption is high; the drug is rapidly and almost completely absorbed from the gastrointestinal tract. TCmax is reached in 0.5-2 hours; Cmax is 5-20 µg/ml. Binding with plasma proteins is 15%. It penetrates through the blood-brain barrier. Less than 1% of the dose of paracetamol taken by a nursing mother penetrates into breast milk. The therapeutically effective plasma concentration of paracetamol is achieved when administered at a dose of 10-15 mg/kg.
Metabolism
Metabolized in the liver (90-95%): 80% enters into conjugation reactions with glucuronic acid and sulfates to form inactive metabolites; 17% undergoes hydroxylation to form 8 active metabolites, which conjugate with glutathione to form already inactive metabolites. In case of glutathione deficiency these metabolites can block enzyme systems of hepatocytes and cause their necrosis. CYP2E1, CYP1A2 isoenzymes and, to a lesser extent, CYP3A4 isoenzyme are also involved in metabolism of the drug. Additional metabolic pathways are hydroxylation to 3-hydroxyparacetamol and methoxylation to 3-methoxyparacetamol, which are subsequently conjugated to glucuronides or sulfates. In adults, glucuronidation predominates; in newborns (including premature infants) and young children, sulfation predominates. Conjugated metabolites of paracetamol (glucuronides, sulfates and conjugates with glutathione) have low pharmacological (including toxic) activity.
Elimation
The elimination half-life (T1/2) is 1-4 hours. Excreted by the kidneys as metabolites, mainly conjugates, only 3% unchanged. In elderly patients, the clearance of paracetamol is decreased and the elimination half-life is increased.
Indications
Indications
An anesthetic for mild to moderate pain syndromes: arthralgia, myalgia, neuralgia, migraine, toothache and headache, algodismenorrhea, pain from injuries and burns.
An antipyretic for acute respiratory diseases and other infectious and inflammatory diseases accompanied by an increase in body temperature.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: non-narcotic analgesic.
ATX code: N02BE01
Pharmacological properties
Pharmacodynamics
Paracetamol has antipyretic and analgesic effects. A non-narcotic analgesic, it blocks cyclooxygenase (COX) I and II mainly in the central nervous system, affecting the centers of pain and thermoregulation. In inflamed tissues, cellular peroxidases neutralize the effect of paracetamol on COX, which explains the almost complete absence of anti-inflammatory effect. Since paracetamol has an extremely small effect on the synthesis of prostaglandins in peripheral tissues, it does not change water-electrolyte metabolism and does not cause damage to the mucous membrane of the gastrointestinal tract. Therefore, paracetamol is particularly suitable for patients with a history of gastrointestinal disease (such as patients with a history of gastrointestinal bleeding or elderly patients) or patients taking concomitant medications where inhibition of peripheral prostaglandins may be undesirable.
Pharmacokinetics
Absorption
Absorption is high, the drug is quickly and almost completely absorbed from the gastrointestinal tract. TCmax is achieved in 0.5-2 hours; Cmax – 5-20 mcg/ml. Communication with plasma proteins – 15%. Penetrates the blood-brain barrier. Less than 1% of the dose of paracetamol taken by a nursing mother passes into breast milk. The therapeutically effective concentration of paracetamol in plasma is achieved when administered at a dose of 10-15 mg/kg.
Metabolism
Metabolized in the liver (90-95%): 80% enters into conjugation reactions with glucuronic acid and sulfates to form inactive metabolites; 17% undergoes hydroxylation to form 8 active metabolites, which conjugate with glutathione to form inactive metabolites. With a lack of glutathione, these metabolites can block the enzyme systems of hepatocytes and cause their necrosis. The metabolism of the drug also involves isoenzymes CYP2E1, CYP1A2 and, to a lesser extent, the CYP3A4 isoenzyme. Additional metabolic pathways include hydroxylation to 3-hydroxyparacetamol and methoxylation to 3-methoxyparacetamol, which are subsequently conjugated to glucuronides or sulfates. In adults, glucuronidation predominates; in newborns (including premature babies) and small children, sulfation predominates. Conjugated metabolites of paracetamol (glucuronides, sulfates and conjugates with glutathione) have low pharmacological (including toxic) activity.
Removal
The half-life (T1/2) is 1-4 hours. Excreted by the kidneys in the form of metabolites, mainly conjugates, only 3% unchanged. In elderly patients, the clearance of paracetamol decreases and the half-life increases.
Special instructions
Special instructions
If no improvement is observed when taking paracetamol or the headache becomes constant, you should consult a doctor. If the febrile syndrome continues during the use of paracetamol for more than 3 days and pain syndrome for more than 5 days, a doctor’s consultation is required.
Patients with glutathione deficiency are susceptible to overdose and precautions must be taken. Glutathione deficiency due to eating disorders, cystic fibrosis, HIV infection, starvation, exhaustion makes it possible to develop severe liver damage with small overdoses of paracetamol (5 g or more). Cases of liver failure and abnormal liver function have been reported in patients with low glutathione levels, in particular in extremely malnourished patients suffering from anorexia, chronic alcoholism or in patients with a low body mass index. The risk of developing liver damage increases in patients with liver damage due to alcoholism.
Taking paracetamol affects laboratory test results in the quantitative determination of glucose and uric acid in plasma. During long-term treatment, monitoring of the peripheral blood picture and the functional state of the liver is necessary.
Paracetamol can cause serious skin reactions such as Stevens-Johnson syndrome, toxic epidermal necrolysis, acute generalized exanthematous pustulosis, which can be fatal. At the first appearance of a rash or other hypersensitivity reactions, use of the drug should be discontinued and you should immediately consult a doctor.
If acute viral hepatitis is detected in a patient, it is necessary to stop taking the drug. Do not take simultaneously with other drugs containing paracetamol.
To avoid toxic liver damage, paracetamol should not be combined with alcoholic beverages, or taken by persons prone to chronic alcohol consumption.
Impact on the ability to drive vehicles and machinery
There is no data on the effect of paracetamol on the ability to drive a car or use other machinery. However, given possible adverse reactions, it is recommended to exercise caution when taking paracetamol when driving vehicles or using other machinery.
Active ingredient
Active ingredient
Paracetamol
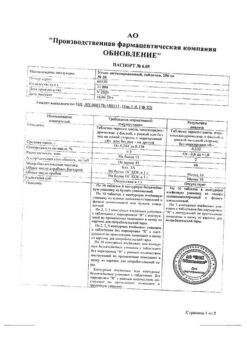
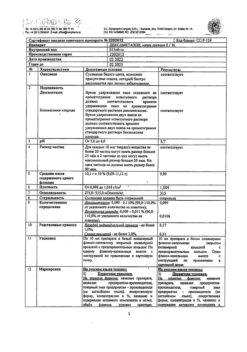
Composition
Composition
Active ingredient: Paracetamol – 500.0 mg
Excipients:
potato starch – 30.2 mg
povidone K 30 – 14.3 mg
magnesium stearate – 4.4 mg
stearic acid – 1.1 mg
Pregnancy
Pregnancy
Pregnancy
Animal and human studies have not shown any risk of use of the drug in pregnant women or harmful effects of the drug on the development of the embryo and fetus. Paracetamol can be used during pregnancy, but it is advisable to use the minimum effective dose and for the shortest possible course.
Breastfeeding period
Passes into breast milk in small quantities. Studies have not established the harmful effects of paracetamol on a child’s body during breastfeeding, however, it must be used with caution.
Contraindications
Contraindications
Hypersensitivity to paracetamol or any other ingredient of the drug;
severe liver or kidney dysfunction;
children under 6 years of age.
With caution
Renal and liver failure of mild to moderate severity, benign hyperbilirubinemia (including Gilbert’s syndrome), deficiency of the enzyme glucose-6-phosphate dehydrogenase, dehydration, hypovolemia, anorexia, bulimia and cachexia (insufficient supply of glutathione in the liver), viral hepatitis, alcoholic liver damage, alcoholism, pregnancy, breastfeeding, old age.
In these cases, you should consult your doctor before taking the drug.
Side Effects
Side Effects
To assess the frequency of adverse reactions (AR), the following criteria were used: “often” (≥ 1/100, < 1/10); “uncommon” (≥ 1/1000, < 1/100); “rare” (≥ 1/10000, < 1/1000); “very rare” (< 1/10000); “frequency unknown” (cannot be estimated from available data). HPs are grouped in accordance with the system-organ classes of the medical dictionary for regulatory activities MedDRA, as well as the recommendations of the World Health Organization.
At recommended doses, paracetamol is usually well tolerated. The following side effects were detected spontaneously during post-registration use.
Blood and lymphatic system disorders
often: postoperative bleeding;
very rarely: anemia, thrombocytopenia, leukopenia, neutropenia, agranulocytosis, hemolytic anemia;
frequency unknown: pancytopenia, sulfohemoglobinemia, methemoglobinemia.
Immune system disorders
rarely: allergic reactions (including skin rash, itching, urticaria, angioedema);
very rare: acute generalized exanthematous pustulosis, Stevens-Johnson syndrome, toxic epidermal necrolysis (Lyell’s syndrome), anaphylaxis.
Mental disorders
often: insomnia, anxiety.
Nervous system disorders
often: headache;
frequency unknown: dystonia, dizziness, psychomotor agitation, disorientation (when taking high doses).
Visual disorders
often: periorbital edema.
Heart disorders
often: tachycardia, chest pain.
Vascular disorders
often: peripheral edema, hypertension;
rarely: decreased blood pressure.
Respiratory, thoracic and mediastinal disorders
often: dyspnea, pathological breathing, pulmonary edema, hypoxia, pleural effusion, wheezing, shortness of breath, cough;
very rarely: bronchospasm (in patients with hypersensitivity to acetylsalicylic acid and other non-steroidal anti-inflammatory drugs).
Gastrointestinal disorders
often: diarrhea, constipation, dyspepsia, bloating;
rarely: abdominal pain, nausea, vomiting;
frequency unknown: dry mouth.
Disorders of the liver and biliary tract
rarely: increased activity of liver enzymes;
frequency unknown: liver failure, hepatitis, liver necrosis.
Skin and subcutaneous tissue disorders
frequency unknown: exanthema.
Musculoskeletal and connective tissue disorders
often: muscle spasms, trismus.
Renal and urinary tract disorders
often: oliguria;
frequency unknown: renal colic, nonspecific bacteriuria, interstitial nephritis, papillary necrosis.
General and administration site disorders
often: pyrexia, feeling tired;
rarely: general malaise/weakness.
Influence on the results of laboratory and instrumental studies
often: hypokalemia, hyperglycemia;
rarely: decrease or increase in prothrombin index;
frequency unknown: increase in creatinine (mostly secondary to hepatorenal syndrome).
If any of these side effects occur, stop taking paracetamol and consult your doctor immediately.
Interaction
Interaction
If you or your child are already taking other medications, you should consult your doctor before starting to take paracetamol.
Inducers of liver microsomal enzymes or potentially hepatotoxic substances (for example, alcohol, rifampicin, isoniazid, hypnotics and antiepileptic drugs, including phenobarbital, phenytoin and carbamazepine) increase the toxicity of paracetamol and can lead to liver damage even at non-toxic doses of paracetamol, so liver function should be monitored.
Phenytoin reduces the effectiveness of paracetamol, therefore, patients taking phenytoin should avoid frequent use of paracetamol, especially in high doses.
Reduces the effectiveness of uricosuric drugs.
Chloramphenicol
Paracetamol may increase the risk of increased chloramphenicol concentrations.
Zidovudine
Paracetamol may increase the risk of developing neutropenia, and therefore hematological parameters should be monitored. Simultaneous use is possible only after consulting a doctor.
Probenecid
Probenecid almost halves the clearance of paracetamol, which requires a reduction in the dose of paracetamol.
Indirect anticoagulants
Repeated use of paracetamol for more than 4 days increases the anticoagulant effect. The international normalized ratio (INR) should be monitored during and after the cessation of concomitant use of paracetamol (especially in high doses and/or for a long time) and coumarin derivatives. Irregular use of paracetamol does not have a significant effect. Propantheline and other drugs that slow down gastric emptying reduce the rate of absorption of paracetamol, which may delay or reduce the onset of the effect.
Metoclopramide and domperidone increase the rate of absorption of paracetamol and, accordingly, the onset of analgesic and antipyretic effects.
Long-term use of barbiturates reduces the effectiveness of paracetamol.
Ethanol contributes to the development of acute pancreatitis.
Long-term combined use of paracetamol and other NSAIDs increases the risk of developing “analgesic” nephropathy and renal papillary necrosis, and the onset of end-stage renal failure.
Simultaneous long-term administration of paracetamol in high doses and salicylates increases the risk of developing kidney or bladder cancer.
Diflunisal increases plasma concentrations by 50% – the risk of developing hepatotoxicity.
Myelotoxic drugs increase the manifestations of hematotoxicity of the drug.
Overdose
Overdose
Symptoms
The clinical picture of acute overdose develops within 24 hours after taking paracetamol. Gastrointestinal disorders appear (nausea, vomiting, loss of appetite, discomfort in the abdominal cavity and (or) abdominal pain), pallor of the skin. When simultaneous administration of 7.5 g or more to adults or more than 140 mg/kg to children, cytolysis of hepatocytes occurs with complete and irreversible liver necrosis, the development of liver failure, metabolic acidosis and encephalopathy, which can lead to coma and death. Ingestion of 5 g or more of paracetamol can lead to liver damage in the presence of risk factors (long-term treatment with carbamazepine, phenobarbital, phenytoin, primidone, rifampicin, St. John’s wort or other drugs that are inducers of microsomal liver enzymes; ethanol abuse, glutathione deficiency, digestive disorders, cystic fibrosis, HIV infection, starvation, cachexia). 12-48 hours after the administration of paracetamol, there is an increase in the activity of microsomal liver enzymes, lactate dehydrogenase, bilirubin concentration and a decrease in prothrombin content. Clinical symptoms of liver damage appear 2 days after an overdose of the drug and reach a maximum on days 4-6. In case of overdose, intoxication is possible, especially in elderly patients, children, patients with liver diseases (caused by chronic alcoholism), in patients with nutritional disorders, as well as in patients taking inducers of microsomal liver enzymes, and fulminant hepatitis, liver failure, cholestatic hepatitis, cytolytic hepatitis, sometimes with a fatal outcome, may develop. In severe cases of overdose, encephalopathy (impaired brain function), cerebral edema, bleeding, hypoglycemia, and even death may develop as a result of liver failure. It is possible to develop acute renal failure with acute tubular necrosis, the characteristic signs of which are pain in the lumbar region, hematuria (admixture of blood or red blood cells in the urine), proteinuria (increased protein in the urine), while severe liver damage may be absent. There have been cases of heart rhythm disturbances and pancreatitis.
Treatment
Immediate hospitalization. If you suspect an overdose, even in the absence of pronounced first symptoms, you must stop using paracetamol and immediately seek medical help. The level of paracetamol in the blood plasma should be determined, but not earlier than 4 hours after the overdose (earlier results are unreliable). Laboratory studies of the activity of microsomal liver enzymes should be performed at the beginning of treatment and then every 24 hours. The introduction of SH-group donors and precursors for the synthesis of glutathione-methionine and acetylcysteine is most effective in the first 8 hours.
Symptomatic treatment: within 1 hour after an overdose, it is recommended to lavage the stomach and take enterosorbents (activated carbon and others). In most cases, the activity of microsomal liver enzymes returns to normal within 1-2 weeks. In very severe cases, a liver transplant may be required. Administration of acetylcysteine within 24 hours of an overdose. The maximum protective effect is provided during the first 8 hours after an overdose; over time, the effectiveness of the antidote drops sharply. If necessary, acetylcysteine is administered intravenously. In the absence of vomiting, methionine can be used before the patient is admitted to the hospital. The need for additional therapeutic measures (further administration of methionine, intravenous administration of acetylcysteine) is determined depending on the concentration of paracetamol in the blood, as well as the time elapsed after its administration. Treatment of patients with severe liver dysfunction 24 hours after taking paracetamol should be carried out in conjunction with specialists from a poison control center or specialized liver disease department.
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after expiration date.
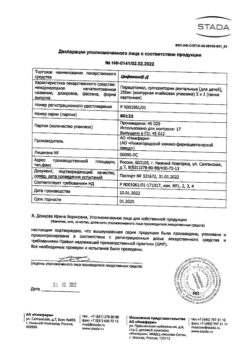
Manufacturer
Manufacturer
Update of PFC JSC, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C. Keep out of reach of children. |
| Manufacturer | Update PFC AO, Russia |
| Medication form | pills |
| Brand | Update PFC AO |
Other forms…
Related products
Buy Paracetamol Reneval, tablets 500 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.