No products in the cart.
Zalasta, tablets 10 mg 28 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Schizophrenia, Manic Depressive Psychosis, Anxiety
Adults
– Olanzapine is indicated for treatment of schizophrenia.
-Olanzapine is effective in maintenance and long-term therapy in patients with schizophrenia who have seen initial treatment effects.
– Olanzapine is indicated for treatment of a moderate to severe manic episode.
– Olanzapine is indicated for relapse prevention in patients with bipolar disorder in whom it has shown efficacy in treating a manic episode.
Indications
Indications
Adults
· Olanzapine is indicated for the treatment of schizophrenia.
· Olanzapine is effective in maintenance and long-term therapy in patients with schizophrenia who have responded to initial treatment.
· Olanzapine is indicated for the treatment of moderate to severe manic episodes.
· Olanzapine is indicated for the prevention of relapse in patients with bipolar disorder, in whom it has been shown to be effective in treating a manic episode.
Pharmacological effect
Pharmacological effect
antipsychotic (neuroleptic)
Special instructions
Special instructions
Contraindicated for persons under 18 years of age.
Elderly patients
A minimum starting dose (5 mg per day) is not usually prescribed, but its use should be considered in patients ≥65 years of age if the individual patient’s clinical condition warrants it.
Patients with renal and/or liver failure
Patients with renal and/or liver failure should begin treatment with a minimum dose (5 mg per day). For moderate liver failure (cirrhosis, Child-Pugh class A or B), the initial dose should be 5 mg, and if necessary, the dose should be increased with caution.
Improvement in the patient’s clinical condition with antipsychotic therapy can take from several days to several weeks; this period requires careful monitoring of the patient.
Risk of suicide
Patients with schizophrenia and bipolar disorder type 1 have a tendency to commit suicide; therefore, during pharmacotherapy, careful monitoring of patients with a high risk of suicide is required. In order to reduce the risk of overdose, a minimum amount of the drug should be prescribed, sufficient to ensure the proper therapeutic effect.
Psychosis and/or behavioral disorders due to dementia
Olanzapine is not recommended for use in patients with psychosis and/or behavioral disorders due to dementia due to increased mortality and risk of cerebrovascular complications. In placebo-controlled studies (6-12 weeks duration) in elderly patients (mean age 78 years) with psychosis and/or behavioral disturbance due to dementia, there was a two-fold increase in the incidence of death in patients receiving olanzapine compared with patients receiving placebo (3.5% versus 1.5%, respectively). The increased incidence of death was independent of the dose of olanzapine (mean daily dose 4.4 mg) and duration of treatment. Risk factors that may predispose to increased mortality in this patient population include age over 65 years, dysphagia, sedation, malnutrition and dehydration, pulmonary disease (eg, pneumonia with or without aspiration), or concomitant use of benzodiazepines. However, the incidence of death was higher in patients receiving olanzapine compared with those receiving placebo, regardless of these risk factors.
Results from the same clinical trials indicate cerebrovascular adverse events (CVAEs) (eg, stroke, transient ischemic attack), including deaths. There was a threefold increase in the incidence of CVN in patients receiving olanzapine compared with patients receiving placebo (1.3% versus 0.4%, respectively). All patients receiving olanzapine and placebo who experienced cerebrovascular events had risk factors. Risk factors for the development of CVN associated with olanzapine treatment include age over 75 years and vascular/mixed dementia. Olanzapine was not effective in these studies.
Parkinson’s disease
The use of olanzapine for the treatment of psychosis caused by the use of dopamine receptor agonists in Parkinson’s disease is not recommended. In clinical studies, worsening of parkinsonian symptoms and hallucinations was observed very often (and with a higher frequency than in the placebo group) (see section “Side effects”), the effectiveness of olanzapine for relieving psychotic symptoms was not greater than placebo. Inclusion criteria for these studies were: stable lowest effective dose of antiparkinsonian drugs (dopamine receptor agonist) and use of the same antiparkinsonian drugs and doses throughout the study. Olanzapine was started at 2.5 mg/day and increased at the discretion of the investigator to 15 mg/day.
Neuroleptic malignant syndrome (NMS)
NMS is a potentially lethal symptom complex caused by antipsychotic drugs. Rare cases of NMS have also been reported with the use of olanzapine. Clinical manifestations of NMS include hyperthermia, muscle rigidity, altered mental status, and autonomic disturbances (unstable pulse or blood pressure, tachycardia, increased sweating, and arrhythmias). Additional signs may include: increased serum CPK activity, myoglobinuria (rhabdomyolysis), and acute renal failure. If a patient develops signs and symptoms of NMS or has an unexplained high fever without additional manifestations of NMS, all antipsychotic medications, including olanzapine, should be discontinued.
Hyperglycemia and diabetes mellitus
Hyperglycemia and/or the development or decompensation of diabetes mellitus, sometimes accompanied by ketoacidosis or diabetic coma, have been reported infrequently, including several fatal cases (see section “Side effects”). In some cases, previous weight gain has been reported, which may be a predisposing factor. Close clinical monitoring is recommended in accordance with current antipsychotic treatment guidelines, such as measuring baseline blood glucose concentrations 12 weeks after initiation of olanzapine therapy and annually thereafter. Patients receiving any antipsychotic agents, including olanzapine, should be monitored for signs and symptoms of hyperglycemia (such as polydipsia, polyuria, polyphagia, and weakness). Patients with diabetes mellitus or risk factors for its development should regularly monitor blood glucose concentrations. Body weight should be checked regularly, for example before, 4, 8 and 12 weeks after starting olanzapine, and quarterly thereafter.
Lipid metabolic disorders
In placebo-controlled studies, undesirable changes in the lipid profile were observed in patients receiving olanzapine (see section “Side effects”). Lipid metabolic disorders should be corrected, especially in patients with dyslipidemia and patients with risk factors for developing lipid metabolic disorders. Patients receiving any antipsychotic drugs, including olanzapine, should have their lipid profile monitored regularly in accordance with current antipsychotic treatment guidelines (eg, before starting treatment, after 12 weeks of starting therapy, and every 5 years thereafter).
Anticholinergic activity
Although olanzapine exhibited anticholinergic activity in vitro, olanzapine therapy was rarely associated with anticholinergic side effects in clinical studies. However, clinical experience with olanzapine in patients with concomitant diseases is limited, so caution is recommended when prescribing the drug to patients with prostatic hypertrophy, paralytic ileus and similar conditions.
Liver dysfunction
Taking olanzapine was often, especially in the early stages of therapy, accompanied by a transient, asymptomatic increase in the activity of “liver” aminotransferases (AST and ALT) in the blood plasma. Caution and follow-up should be exercised in patients with increased plasma ALT and/or AST levels, symptoms of liver failure, conditions that cause decreased liver function reserve, or patients using potentially hepatotoxic drugs. In patients with hepatitis (including hepatocellular, cholestatic and mixed liver disease), treatment with olanzapine should be discontinued.
Neutropenia
Olanzapine should be used with caution in patients with low white blood cell and/or neutrophil counts regardless of cause, a history of drug suppression/bone marrow toxicity, bone marrow suppression due to concomitant disease, radiation or chemotherapy, and in patients with hypereosinophilic conditions or myeloproliferative disease. Neutropenia has often been reported with concomitant use of olanzapine and valproic acid (see section “Side effects”).
Discontinuation of therapy
Increased sweating, insomnia, tremor, anxiety, nausea, and vomiting were reported rarely (≥ 0.01% and < 0.1%) during abrupt discontinuation of olanzapine.
QT interval
In clinical trials, clinically significant prolongation of the QT interval (QT interval with Friederici correction [QTcF] ≥ 500 ms from baseline QTcF < 500 ms) was observed infrequently (0.1-1%) in patients receiving olanzapine, with no significant difference from placebo in the incidence of adverse cardiac events. However, like other antipsychotics, caution should be exercised when prescribing olanzapine concomitantly with drugs that can prolong the QTc interval, especially in elderly patients, patients with congenital prolongation of the QT interval, chronic heart failure, myocardial hypertrophy, hypokalemia or hypomagnesemia.
Thromboembolism
Venous thromboembolism (VTE) has been reported infrequently (≥ 0.1% and < 1%) during olanzapine therapy. A cause-and-effect relationship between the use of olanzapine and VTE has not been established. However, given that patients with schizophrenia often have acquired risk factors for the development of venous thromboembolism, it is necessary to identify all possible risk factors for VTE (for example, immobilization of patients) and take the necessary preventive measures.
General activity of the central nervous system (CNS)
Given the major effects of olanzapine on the central nervous system, caution should be exercised when using olanzapine concomitantly with other centrally acting drugs and ethanol. Because olanzapine exhibits dopamine receptor antagonism in vitro, it may block the effects of direct and indirect dopamine receptor agonists.
Convulsions
Olanzapine should be used with caution in patients with a history of seizures or exposure to factors that lower the seizure threshold. Convulsions have been reported infrequently during treatment with olanzapine. In most cases, a history of seizures or risk factors for seizures were reported.
Tardive dyskinesia
In comparative studies lasting a year or less, treatment with olanzapine was statistically significantly less likely to be accompanied by the development of iatrogenic dyskinesia. However, the risk of developing tardive dyskinesia increases with long-term olanzapine therapy. Therefore, if signs or symptoms of tardive dyskinesia occur in a patient using olanzapine, dose reduction or discontinuation of olanzapine should be considered. After stopping therapy, these symptoms may temporarily worsen or even recur.
Postural hypotension
In clinical studies of olanzapine, postural hypotension was reported infrequently in elderly patients. As with other antipsychotics, periodic monitoring of blood pressure is recommended in patients over 65 years of age.
Sudden death from cardiovascular failure
According to post-registration experience with olanzapine, cases of sudden death from cardiovascular failure have been reported. In a retrospective observational cohort study, the risk of sudden sudden cardiovascular death in patients receiving olanzapine was approximately twice as high as in patients not receiving antipsychotics. The risk of olanzapine use in the study was comparable to that of the atypical antipsychotics included in the pooled analysis.
Use of olanzapine in children
Olanzapine is not recommended for use in children and adolescents. In studies in adolescents 13-17 years of age, various adverse reactions were reported, including weight gain, lipid metabolism disorders, and hyperprolactinemia.
Special information on excipients
The drug Zalasta® contains lactose and is therefore contraindicated in patients with lactase deficiency, lactose intolerance, and glucose-galactose malabsorption syndrome.
Studies of the effect on the ability to drive vehicles and other machinery have not been conducted. Because olanzapine may cause drowsiness and dizziness, patients should be warned about the dangers when operating machinery, including vehicles.
Active ingredient
Active ingredient
Olanzapine
Composition
Composition
for 1 tablet 2.5 mg/5 mg/7.5 mg/10 mg/15 mg/20 mg:
Active ingredient:
Olanzapine 2.50 mg/5.00 mg/7.50 mg/10.00 mg/15.00 mg/20.00 mg
Excipients: cellactose1 [alpha-lactose monohydrate, cellulose], pregelatinized starch, corn starch, colloidal silicon dioxide, magnesium stearate
Cellactose1 is a spray-dried compound consisting of alpha-lactose monohydrate and cellulose powder, dry matter.
Pregnancy
Pregnancy
Pregnancy
Adequate and strictly controlled studies have not been conducted in pregnant women. Patients should be warned to notify their prescribers if they become pregnant or plan to become pregnant while being treated with olanzapine. However, due to limited experience in humans, olanzapine should be used during pregnancy if the potential benefit to the mother outweighs the possible risk to the fetus.
Infants whose mothers took olanzapine during the third trimester of pregnancy are at risk of developing adverse reactions, including extrapyramidal symptoms and/or withdrawal symptoms, which may vary in severity and duration after delivery. Agitation, hypertonicity, hypotonicity, tremor, somnolence, respiratory distress and malnutrition have been reported. In this regard, newborns should be closely monitored.
Breastfeeding period
A study in healthy lactating women found that olanzapine passes into breast milk. The mean dose received by the child (mg/kg) at steady state was 1.8% of the maternal olanzapine dose (mg/kg). Patients using olanzapine are advised not to breastfeed.
Fertility
There is no information on the effect on fertility.
Contraindications
Contraindications
· Hypersensitivity to any of the components of the drug.
· Patients at risk of developing angle-closure glaucoma.
· Children under 18 years of age.
· Lactase deficiency, lactose intolerance, glucose-galactose malabsorption syndrome.
Interaction
Interaction
Drug interaction studies were conducted exclusively in adult patients.
Potential interactions affecting the pharmacokinetics of olanzapine
Because olanzapine is metabolized by CYP1A2, substances that can selectively induce or inhibit this isoenzyme may alter the pharmacokinetics of olanzapine.
Induction of the CYP1A2 isoenzyme
Smoking and carbamazepine can induce the metabolism of olanzapine, which can lead to a decrease in the serum concentration of the latter. There was a mild to moderate increase in the clearance of olanzapine. Clinical results are limited; clinical observation is recommended, with dose increases if necessary (see section “Dosage and Administration”).
Inhibition of the CYP1A2 isoenzyme
Fluvoxamine, a specific inhibitor of the CYP1A2 isoenzyme, has been shown to significantly inhibit the metabolism of olanzapine. The average increase in olanzapine plasma Cmax after fluvoxamine administration is 54% in non-smoking women and 77% in smoking men. The mean increases in area under the concentration-time curve (AUC) were 52% and 108%, respectively. Patients using fluvoxamine or other CYP1A2 inhibitors, such as ciprofloxacin, should be prescribed a lower dose of olanzapine. Patients receiving therapy with a CYP1A2 inhibitor should consider reducing the dose of olanzapine.
Reduced bioavailability
Activated charcoal reduces the bioavailability of oral olanzapine by 50-60%, so it should be used 2 hours before or after taking olanzapine.
Fluoxetine (inhibitor of the CYP2D6 isoenzyme), single doses of antacids (aluminium- and magnesium-containing) and cimetidine do not have a significant effect on the pharmacokinetics of olanzapine.
The ability of olanzapine to influence the pharmacokinetics of other drugs
Olanzapine may block the effects of direct and indirect dopamine receptor agonists.
Olanzapine does not inhibit the main isoenzymes of the cytochrome P450 system in vitro (for example, 1A2, 2D6, 2C9, 2C19, 3A4). The results of in vivo studies confirm the absence of inhibition of the metabolism of the following drugs: tricyclic antidepressants (metabolized mainly with the participation of the CYP2D6 isoenzyme), warfarin (CYP2C19), theophylline (CYP1A2) and diazepam (CYP3A4 and CYP2C19).
Olanzapine does not interact with lithium and biperiden.
Indicators of plasma concentrations of valproic acid showed that the simultaneous use of olanzapine does not require dose adjustment of valproic acid.
General activity of the central nervous system (CNS)
Caution should be exercised in patients who drink alcohol or take drugs that depress the central nervous system.
Concomitant use of olanzapine with antiparkinsonian drugs in patients with Parkinson’s disease and dementia is not recommended (see section “Special Instructions”).
QTc interval
Caution should be exercised when using olanzapine simultaneously with drugs that prolong the QTc interval (see section “Special Instructions”).
Overdose
Overdose
Symptoms: Very common symptoms (≥ 10%) in olanzapine overdose are tachycardia, agitation/aggression, dysarthria, various extrapyramidal symptoms and decreased consciousness of varying severity (from sedation to coma).
Other clinically significant effects of olanzapine overdose included delirium, seizures, neuroleptic malignant syndrome (NMS), respiratory depression, aspiration, hypertension or hypotension, arrhythmias (<2% of overdose cases), and cardiac and respiratory arrest. The minimum dose for an acute overdose with a fatal outcome was 450 mg, the maximum dose for an overdose with a favorable outcome (survival) was 2 g of olanzapine.
Treatment: There is no specific antidote for olanzapine. Inducing vomiting is not recommended. Standard procedures for overdose are indicated, for example, gastric lavage, taking activated charcoal. Taking activated charcoal while taking oral olanzapine has shown a decrease in the bioavailability of olanzapine by up to 50-60%.
Symptomatic treatment is indicated in accordance with the clinical condition and monitoring of vital body functions, including correction of arterial hypotension, circulatory disorders and maintenance of respiratory function. Epinephrine, dopamine and other adrenergic agonists that are β-adrenergic receptor agonists should not be used, since stimulation of these receptors may exacerbate arterial hypotension. In order to identify possible arrhythmias, cardiovascular activity should be monitored. Careful medical observation should be continued until the patient recovers completely.
Clinical pharmacology
Clinical pharmacology
Pharmacodynamics
Olanzapine is an antipsychotic, antimanic and mood-stabilizing agent with a wide pharmacological spectrum of influence on a number of receptor systems. Preclinical studies have established affinity (Ki < 100 nmol/l) for various receptors: 5-HT2A/2C-, 5-HT3-, 5-HT6-serotonin, D1-, D2-, D3-, D4-, D5-dopamine, M1-5-muscarinic cholinergic receptors, α1-adrenergic and H1-histamine receptors. In animal studies evaluating the behavioral effects of olanzapine, olanzapine exhibited antagonism at serotonin, dopamine and m-cholinergic receptors, consistent with its receptor binding profile.
Under in vitro and in vivo conditions, olanzapine has a more pronounced affinity and activity for 5-HT2-serotonin receptors than for D2-dopamine receptors. According to electrophysiological studies, olanzapine selectively reduces the activity of mesolimbic (A10) dopaminergic neurons, and at the same time has a slight effect on striatal nerve pathways (A9) involved in the regulation of motor (motor) functions. Olanzapine reduces the conditioned defense response (in a test for antipsychotic activity) at doses below those that cause catalepsy (an effect indicative of motor [motor] adverse reactions). Unlike some other antipsychotics, olanzapine increases response in the “anxiolytic” test.
In a study in healthy volunteers with a single dose (10 mg) followed by positron emission tomography, olanzapine was more likely to bind to 5-HT2A-serotonin receptors than to D2-dopamine receptors. In addition, a study using single photon emission computed tomography in patients with schizophrenia found that patients who responded to olanzapine had lower connectivity with striatal D2 receptors compared with patients who responded to other antipsychotics and risperidone, while being comparable to patients who responded to clozapine.
Clinical effects
In two of two placebo-controlled clinical trials and two of three comparative clinical trials involving more than 2,900 patients with schizophrenia who had both positive and negative symptoms, olanzapine resulted in statistically significant reductions in the severity of both types of disorders.
In an international, double-blind, comparative study of 1,481 patients with schizophrenia, schizoaffective and related disorders, and associated depressive symptoms (mean Montgomery-Åsberg Depression Scale score 16.6), a prospective secondary analysis of changes in mood scores at the end of the study compared with baseline values showed a statistically significant (p=0.001) improvement in patients’ condition during treatment. olanzapine (-6.0) compared to haloperidol (-3.1).
The use of olanzapine for 3 weeks in patients with a manic or mixed episode of bipolar disorder was more effective in reducing the severity of manic symptoms compared with placebo and a complex of sodium valproate and valproic acid in a 1:1 ratio. Olanzapine also showed comparable efficacy to haloperidol in the proportion of patients achieving symptomatic remission of mania and depression at 6 and 12 weeks of use. The use of olanzapine at a dose of 10 mg as part of combination therapy in combination with lithium or valproic acid for at least 2 weeks led to a greater reduction in the severity of mania than monotherapy with lithium or valproic acid after 6 weeks of use of the latter.
In a 12-month relapse prevention clinical trial in patients with a manic episode who achieved remission on olanzapine and were subsequently randomized to olanzapine or placebo, olanzapine was statistically significantly superior to placebo in achieving the primary endpoint of relapse of bipolar disorder. Olanzapine has also been shown to be superior to placebo in preventing relapse of both manic and depressive episodes.
In another 12-month relapse prevention clinical trial in patients with a manic episode who achieved remission on olanzapine in combination with lithium and were subsequently randomized to either olanzapine alone or lithium alone, olanzapine was found to be statistically noninferior to lithium in achieving the primary endpoint of relapse of bipolar disorder (olanzapine group – 30%, lithium group – 38.23%; p=0.055).
In an 18-month clinical trial of combination therapy with olanzapine in combination with a mood stabilizer (lithium or valproic acid) in patients with a manic or mixed episode, there was no statistically significant superiority of long-term combination therapy over lithium or valproic acid monotherapy with respect to the time to relapse of bipolar disorder, defined in accordance with diagnostic (syndromic) criteria.
Pharmacokinetics
Suction
After oral administration, olanzapine is well absorbed, its maximum concentration (Cmax) in blood plasma is reached after 5-8 hours. Eating does not affect absorption. Absolute bioavailability after oral administration versus intravenous administration was not determined.
Distribution
The binding of olanzapine to plasma proteins is 93% (in the concentration range of 7-1000 ng/ml). Olanzapine binds preferentially to albumin and α1-acid glycoprotein.
Metabolism
Olanzapine is metabolized in the liver through conjugation and oxidation. The main circulating metabolite is 10-N-glucuronide, which does not cross the blood-brain barrier. The isoenzymes CYP1A2 and CYP2D6 are involved in the formation of N-desmethyl and 2-hydroxymethyl metabolites; in animal studies, both metabolites had significantly less pronounced pharmacological activity in vivo than olanzapine. The main pharmacological activity of the drug is due to the parent compound – olanzapine.
Withdrawal
After oral administration, the mean terminal half-life (T1/2) of olanzapine in healthy volunteers varies by age and gender.
Pharmacokinetics in certain groups of patients
Elderly patients
In healthy elderly volunteers (65 years and older), compared with younger individuals, the average T1/2 increased (51.8 hours versus 33.8 hours) and clearance decreased (17.5 l/hour versus 18.2 l/hour). Pharmacokinetic variability in elderly volunteers was consistent with that in younger subjects. In 44 patients with schizophrenia over 65 years of age, the use of olanzapine in doses of 5-20 mg/day did not lead to differences in the profile of adverse events.
Gender
The average T1/2 in women compared to men is slightly increased (36.7 hours versus 32.3 hours), and clearance is reduced (18.9 l/hour versus 27.3 l/hour). However, the safety profile of olanzapine (at doses of 5-20 mg/day) in female patients (n=467) is comparable to that in male patients (n=869).
Kidney failure
In patients with renal failure (creatinine clearance [CC] < 10 ml/min) compared with healthy volunteers, there were no significant differences in mean T1/2 (37.7 hours vs. 32.4 hours) or clearance (21.2 L/hour vs. 25.0 L/hour). A material balance study showed that approximately 57% of radiolabeled olanzapine was found in urine, mainly as metabolites.
Liver failure
A small study of the effect of hepatic impairment with oral olanzapine (2.5-7.5 mg single dose) in 6 patients with clinically significant Child-Pugh class A (n=5) and class B (n=1) cirrhosis revealed a minor effect on pharmacokinetics: patients with mild to moderate hepatic impairment had a slight increase in systemic clearance and shortening T1/2 compared with patients without impairment liver function (n=3). There were more smokers among people with liver cirrhosis (4/6; 67%) than among people without liver dysfunction (0/3; 0%).
Smoking
In smoking individuals with mild liver failure (class A according to the Child-Pugh classification), the average T1/2 increased (39.3 hours) and clearance decreased (18 l/hour) similar to non-smoking healthy individuals (48.8 hours and 14.1 l/hour, respectively).
In non-smoking patients compared to smokers (men and women), the average T1/2 lengthened (38.6 hours versus 30.4 hours), and clearance decreased (18.6 l/hour versus 27.7 l/hour).
Plasma clearance of olanzapine is lower in older people compared to younger people, in men compared to women, and in non-smokers compared to smokers. However, the dependence of olanzapine clearance and T1/2 on age, gender and smoking is small compared to the overall interindividual variability.
Race
In a study involving subjects of European, Japanese and Chinese descent, no differences in the pharmacokinetics of olanzapine were established.
Storage conditions
Storage conditions
At a temperature not exceeding 25 ºС, in the original packaging.
Keep out of reach of children
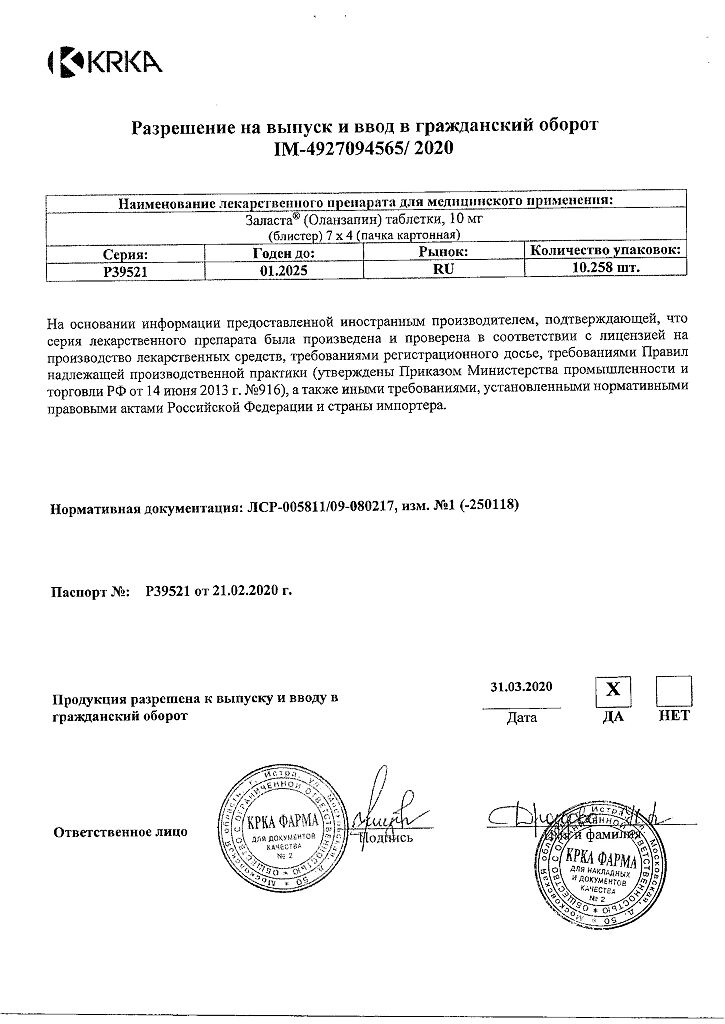
Shelf life
Shelf life
5 years.
Do not use the drug after the expiration date.
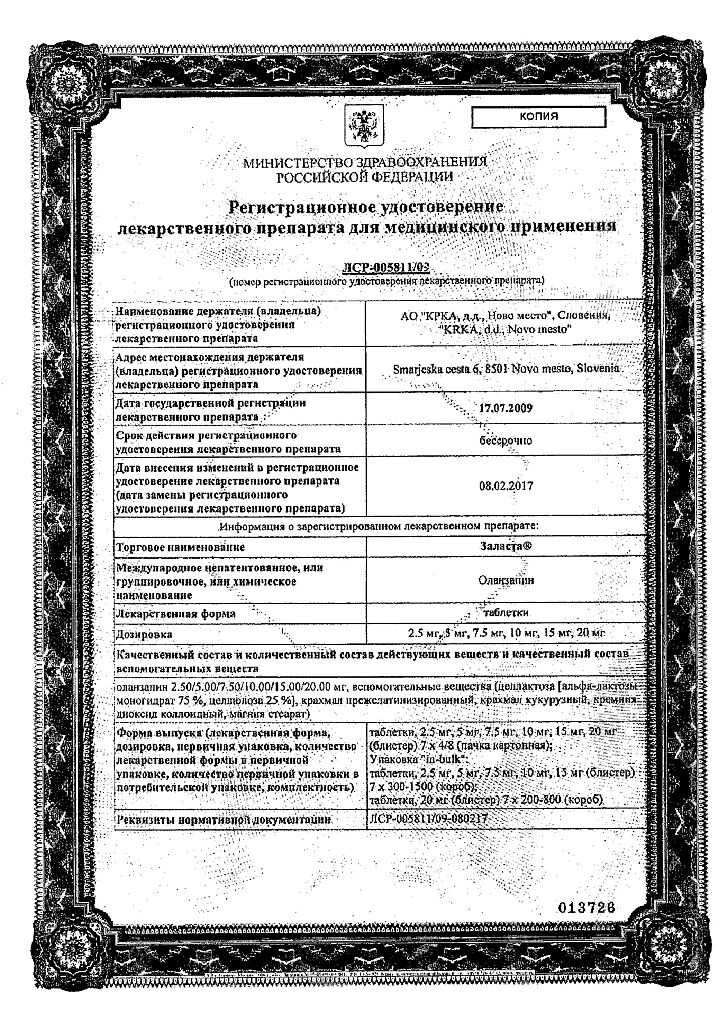
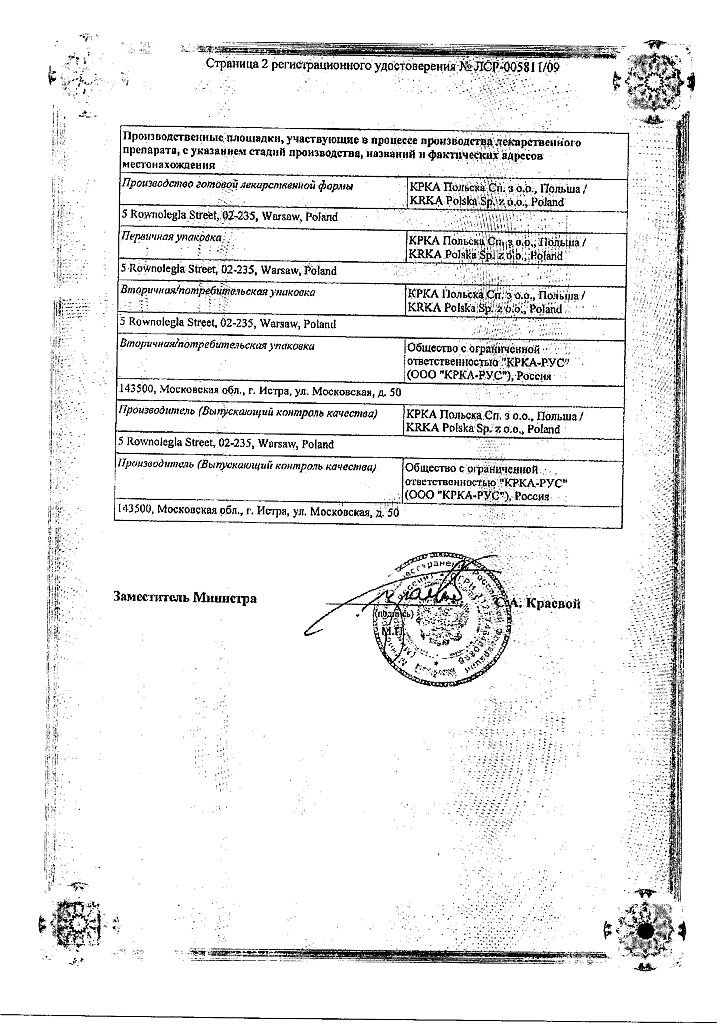
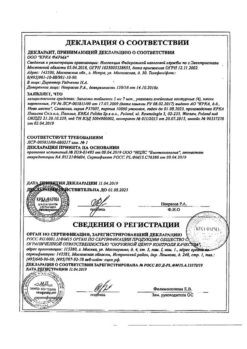
Manufacturer
Manufacturer
KRKA dd Novo Mesto, Slovenia
Additional information
| Shelf life | 5 years. Do not use the product after the expiration date. |
|---|---|
| Conditions of storage | At the temperature not more than 25 ºC, in the original package. Keep out of reach of children . |
| Manufacturer | KRKA-RUS/KRKA, Russia |
| Medication form | pills |
| Brand | KRKA-RUS/KRKA |
Other forms…
Related products
Buy Zalasta, tablets 10 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.