No products in the cart.
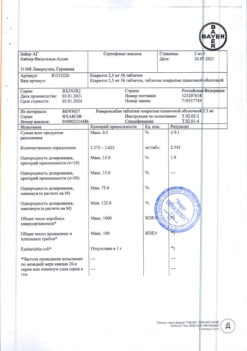
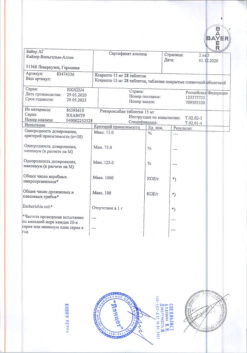
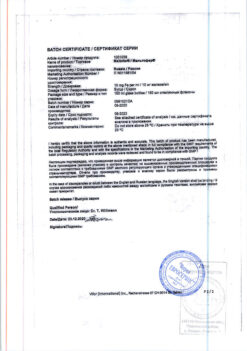
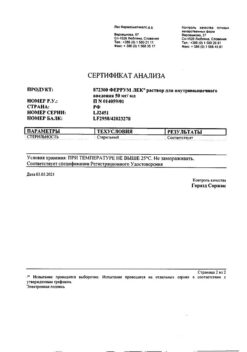
Xarelto, 20 mg 100 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Rivaroxaban is a highly selective direct factor Xa inhibitor with high bioavailability when taken orally.
The activation of factor X to form factor Xa through the internal and external clotting pathways plays a central role in the coagulation cascade.
Pharmacodynamic effects
Dose-dependent inhibition of factor Xa has been observed in humans. Rivaroxaban has a dose-dependent effect on prothrombin time and correlates well with plasma concentrations (r=0.98) when the Neoplastin® kit is used for the assay. Results will vary if other reagents are used. Prothrombin time should be measured in seconds, because MHO is only calibrated and certified for coumarin derivatives and cannot be used for other anticoagulants.
In patients with non-valvular atrial fibrillation taking rivaroxaban for prevention of stroke and systemic thromboembolism, the 5/95 percentile for prothrombin time (Neoplastin®) 1-4 h after taking the tablet (ie.i.e., at maximum effect) range from 14 to 40 seconds in patients taking 20 mg once daily and from 10 to 50 seconds in patients with renal impairment (CKR 49 to 30 mL/min) taking 15 mg once daily.
In patients receiving rivaroxaban for the treatment and prevention of recurrent deep vein thrombosis (DVT) and pulmonary embolism (PATE), 5/95 percentiles for prothrombin time (Neoplastin®) 2 to 4 h after taking the tablet (i.e.i.e., at maximum effect) range from 17 to 32 seconds in patients taking 15 mg 2 times/day and from 15 to 30 seconds in patients taking 20 mg once/day.
Rivaroxaban also dose-dependently increases the ABTV and HepTest® result; however, these parameters are not recommended for evaluating the pharmacodynamic effects of rivaroxaban. Also, if clinically warranted, rivaroxaban concentrations may be measured using a calibrated quantitative anti-Factor Xa test.
Monitoring of clotting parameters is not required during treatment with Xarelto® .
In healthy men and women over 50 years of age, no prolongation of the QT interval was observed with rivaroxaban.
Indications
Indications
– Prevention of stroke and systemic thromboembolism in patients with non-valvular atrial fibrillation;
Treatment of deep vein thrombosis and pulmonary embolism and prevention of recurrent DVT and TELA.
Active ingredient
Active ingredient
Composition
Composition
In 1 tablet contains:
Rivaroxaban micronized 20 mg.
How to take, the dosage
How to take, the dosage
The drug is taken orally with meals.
If the patient is unable to swallow the tablet whole, the Xarelto® tablet may be crushed and mixed with water or a liquid food such as apple puree immediately before ingestion. After taking the crushed Xarelto® 15 mg or 20 mg tablet, a meal should be taken immediately.
The crushed Xarelto® tablet can be administered via a gastric tube. The position of the tube in the gastrointestinal tract should be further coordinated with the physician before taking Xarelto®. The crushed tablet should be inserted through the gastric tube in a small amount of water, after which a small amount of water should be introduced to wash out the drug residues from the walls of the tube. After taking crushed Xarelto® 15 mg or 20 mg tablets, enteral feeding should be started immediately.
Prevention of stroke and systemic thromboembolism in patients with non-valvular atrial fibrillation
The recommended dose is 20 mg once daily.
For patients with impaired renal function (CKR 49-30 ml/min), the recommended dose is 15 mg once daily. The recommended maximum daily dose is 20 mg. Xarelto® therapy should be considered a long-term treatment as long as the benefit of treatment exceeds the risk of possible complications.
Activities for missed doses
If the next dose is missed, the patient should take Xarelto® immediately and continue regular administration the next day according to the recommended regimen.
The dose taken should not be doubled to make up for a previously missed dose.
Treatment of DVT and TELA and prevention of recurrent DVT and TELA
The recommended starting dose in the treatment of acute DVT or TELA is 15 mg 2 times daily for the first 3 weeks followed by transition to a dose of 20 mg once daily for further treatment and prevention of recurrent DVT and TELA.
The maximum daily dose is 30 mg for the first 3 weeks of treatment and 20 mg for further treatment.
The duration of treatment is determined on an individual basis after careful weighing of the ratio of the benefits of treatment to the risk of bleeding. The minimum duration of treatment (at least 3 months) should be based on an assessment regarding reversible risk factors (i.e., previous surgery, trauma, period of immobilization). The decision to extend treatment for a longer period of time is based on an assessment concerning permanent risk factors, or in the case of idiopathic DVT or TELA.
Activities for missed doses
It is important to adhere to the established dosing regimen.
If the next dose is missed on the 15 mg twice-daily dosing regimen, the patient should take Xarelto® immediately to reach the daily dose of 30 mg. Thus, two 15 mg tablets can be taken in one sitting. The next day, the patient should continue the regular intake of the drug according to the recommended regimen.
If the next dose is missed at 20 mg once daily, the patient should take Xarelto® immediately and continue regular administration the next day according to the recommended regimen.
Separate patient groups
There is no need for dose adjustments based on patient age (>65 years), gender, body weight, or ethnicity.
Xarelto® is contraindicated in patients with liver disease accompanied by coagulopathy, which causes a clinically significant risk of bleeding. Patients with other liver diseases do not require dose changes. The limited clinical data available in patients with moderate hepatic impairment (class B according to Child-Pugh classification) indicate a significant increase in pharmacological activity of the drug. No clinical data are available for patients with severe hepatic impairment (Child-Pugh class C).
When prescribing Xarelto® in patients with renal impairment (CK of 80-50 ml/min) no dose adjustment is required.
In prophylaxis of stroke and systemic thromboembolism in patients with atrial fibrillation of non-valvular origin with renal insufficiency (KC 49-30 ml/min), the recommended dose is 15 mg once daily.
When treating DVT and TELA and preventing recurrence of DVT and TELA in patients with renal insufficiency (KKR 49-30 ml/min) no dose adjustment is required.
Limited clinical data available in patients with renal impairment (KC 29-15 mL/min) demonstrate a significant increase in rivaroxaban concentrations in these patients. Xarelto® should be used with caution to treat this category of patients.
The use of Xarelto® in patients with CK<15 ml/min is not recommended.
Transfer patients from vitamin K antagonists (VKAs) to Xarelto®
In the prevention of stroke and systemic thromboembolism, discontinue VKA treatment and initiate Xarelto® treatment at MHOâ¤3.
For DVT and TELA, discontinue AVC treatment and start Xarelto® treatment at MHOâ¤2.5.
When patients switch from AVC to Xarelto®, MHO values will be erroneously elevated after taking Xarelto®. The MHO value is not suitable for determining the anticoagulant activity of Xarelto® and therefore should not be used for this purpose.
Transition from Xarelto® to vitamin K antagonists (VKAs)
There is a possibility of insufficient anticoagulant effect when switching from Xarelto® to VKAs. Therefore, it is necessary to ensure continuous sufficient anticoagulant effect during such transition with alternative anticoagulants. It should be noted that Xarelto® may contribute to increased MHO. Patients transitioning from Xarelto® to AVC should take AVC concomitantly until MHO reaches â¥2. During the first two days of the transition period, the standard dose of AVC should be used, followed by the dose of AVC determined according to the MHO value. Thus, during concomitant use of Xarelto® and AVC, MHO should be determined no earlier than 24 h after the previous dose, but before the next dose of Xarelto®. After discontinuation of Xarelto®, the MHO value can be reliably determined 24 hours after the last dose.
Transition from parenteral anticoagulants to Xarelto®
. In patients receiving parenteral anticoagulants, the use of Xarelto® should be started 0-2 h before the time of the next scheduled parenteral administration of the drug (e.g., low molecular weight heparin) or at the time of discontinuation of continuous parenteral administration of the drug (e.g., intravenous infusion of unfractionated heparin).
Transition from Xarelto® to parenteral anticoagulants
The first dose of Xarelto® should be stopped and the first dose of parenteral anticoagulant administered at the time the next dose of Xarelto® should be taken.
Cardioversion in the prevention of stroke and systemic thromboembolism
The treatment with Xarelto® may be initiated or continued in patients who may require cardioversion. In transesophageal echocardiography-controlled cardioversion (TECCG) in patients who have not previously received anticoagulant therapy, treatment with Xarelto® should be initiated at least 4 hours before cardioversion to ensure adequate anticoagulation.
Interaction
Interaction
Pharmacokinetic interaction
Excretion of rivaroxaban is primarily by metabolism in the liver mediated by the cytochrome P450 system (CYP3A4, CYP2J2) and also by renal excretion of unchanged drug substance using the P-gp/Bcrp (P-glycoprotein/milk cancer resistance protein) carrier systems.
Rivaroxaban does not inhibit or induce the CYP3A4 isoenzyme or other important cytochrome isoforms.
The concomitant use of rivaroxaban and strong CYP3A4 and P-glycoprotein isoenzyme inhibitors may lead to decreased renal and hepatic clearance and thus significantly increase systemic exposure.
The co-administration of rivaroxaban and the azole antifungal agent ketoconazole (400 mg once daily), which is a strong inhibitor of CYP3A4 and P-glycoprotein, resulted in a 2.6-fold and increased the mean Cmax of rivaroxaban by 1.7-fold, which was accompanied by a significant increase in the pharmacodynamic action of the drug.
The co-administration of Xarelto® and the HIV protease inhibitor ritonavir (600 mg 2 times/day), a potent CYP3A4 and P-glycoprotein inhibitor, resulted in a 2.5-fold and increased the mean Cmax of rivaroxaban by 1.6-fold, which was accompanied by a significant increase in the pharmacodynamic action of the drug. Therefore Xarelto® is not recommended for use in patients receiving systemic treatment with antifungal drugs of azole group or HIV protease inhibitors.
Clarithromycin (500 mg twice daily), a potent CYP3A4 isoenzyme inhibitor and moderate P-glycoprotein inhibitor, caused 1.5-fold increase in AUC values and 1.4-fold increase in Cmax of rivaroxaban. This increase is of the order of the normal variability of AUC and Cmax and is considered clinically insignificant.
Eritromycin (500 mg 3 times daily), a moderate inhibitor of the CYP3A4 isoenzyme and P-glycoprotein, caused a 1.3-fold increase in the AUC and Cmax values of rivaroxaban. This increase is of the order of the normal variability of AUC and Cmax and is considered clinically insignificant.
In patients with renal impairment (CK ⤠80-50 mL/min), erythromycin (500 mg 3 times/day) caused a 1.8-fold increase in AUC values of rivaroxaban and a 1.6-fold increase in Cmax compared with patients with normal renal function who were not receiving concomitant therapy. In patients with renal impairment (CKR 49-30 ml/min), erythromycin caused a 2.0-fold increase in the AUC of rivaroxaban and a 1.6-fold increase in Cmax compared to patients with normal renal function who were not receiving concomitant therapy.
Fluconazole (400 mg once daily), a moderate inhibitor of the CYP3A4 isoenzyme, caused a 1.4-fold increase in mean AUC of rivaroxaban and a 1.3-fold increase in mean Cmax. This increase is of the order of the normal variability of AUC and Cmax is considered clinically insignificant.
The concomitant use of rivaroxaban with dronedarone should be avoided due to limited clinical data on co-administration.
The co-administration of Xarelto® and rifampicin, which is a strong inducer of CYP3A4 and P-glycoprotein, resulted in a reduction of the mean AUC of rivaroxaban by approximately 50% and a concomitant reduction of its pharmacodynamic effects.
The co-administration of rivaroxaban with other strong CYP3A4 inducers (e.g., phenytoin, carbamazepine, phenobarbital or preparations of St. John’s wort) may also result in decreased plasma concentrations of rivaroxaban. Decreased plasma concentrations of rivaroxaban have been found to be clinically insignificant.
Powerful CYP3A4 inducers should be used with caution.
Pharmacodynamic interaction
After concomitant use of enoxaparin sodium (single dose of 40 mg) and Xarelto® (single dose of 10 mg) there was a summarized effect on anti-Factor Xa activity with no additional summarized effects on clotting tests (prothrombin time, ACTV). Enoxaparin did not alter the pharmacokinetics of rivaroxaban.
Due to the increased risk of bleeding, caution should be exercised when coadministering with any other anticoagulants.
No pharmacokinetic interaction was found between Xarelto® at a dose of 15 mg and clopidogrel (loading dose of 300 mg followed by a maintenance dose of 75 mg), but a significant increase in bleeding time was found in a subset of patients that was not correlated with the degree of platelet aggregation and P-selectin or GPIIb/IIIa-receptor content.
There was no clinically significant increase in bleeding time after co-administration of Xarelto® (15 mg) and naproxen (500 mg). However, a more pronounced pharmacodynamic response is possible in individuals.
Caution should be exercised when co-administering Xarelto® with NSAIDs (including acetylsalicylic acid) and platelet aggregation inhibitors, as use of these drugs generally increases the risk of bleeding.
. Switching patients from warfarin (MHO 2 to 3) to Xarelto® (20 mg) or from Xarelto® (20 mg) to warfarin (MHO 2 to 3) increased prothrombin time/MNO (Neoplastin) more than would be expected by simply summing the effects (individual MHO values can reach 12), whereas effects on ACTV, suppression of factor Xa activity and endogenous thrombin potential were additive.
If the pharmacodynamic effects of Xarelto® need to be investigated during the transition period, anti-Xa activity, PiCT and HepTest® determination may be used as necessary tests that are not affected by warfarin. From day 4 after discontinuation of warfarin, all test results (including PV, ACTV, inhibition of factor Xa activity, and on EPT (endogenous thrombin potential)) reflect only the effects of Xarelto®.
If it is necessary to investigate the pharmacodynamic effects of warfarin during the transient period, the measurement of MHO during the Spr. of rivaroxaban (24 h after the previous administration of rivaroxaban) may be used, since rivaroxaban has minimal effect on this parameter during this period.
No pharmacokinetic interaction has been reported between warfarin and Xarelto®.
The drug interaction of Xarelto® with phenyndione AVC has not been studied. It is recommended to avoid transfer of patients from Xarelto® therapy to AVC therapy with phenyndione and vice versa whenever possible. There is limited experience with transferring patients from AVC therapy with acenocoumarol to Xarelto®.
If it becomes necessary to transfer a patient from Xarelto® therapy to AVC therapy with phenindion or acenocoumarol, special caution should be exercised, daily monitoring of pharmacodynamic effects of drugs (MHO, prothrombin time) should be performed immediately before taking the next dose of Xarelto®. If it is necessary to switch a patient from AVC therapy with phenindion or acenocoumarol to therapy with Xarelto®, special caution should be exercised, control of pharmacodynamic actions of the drugs is not required.
Incompatibilities
It is unknown.
No interactions have been identified
No pharmacokinetic interactions have been identified between rivaroxaban and midazolam (CYP3A4 substrate), digoxin (P-glycoprotein substrate) or atorvastatin (CYP3A4 and P-glycoprotein substrate).
The co-administration with the proton pump inhibitor omeprazole, histamine H2-receptor blocker ranitidine, aluminum hydroxide/magnesium hydroxide antacids, naproxen, clopidogrel or enoxaparin does not affect bioavailability and pharmacokinetics of rivaroxaban.
No clinically significant pharmacokinetic or pharmacodynamic interactions have been observed when Xarelto® and acetylsalicylic acid at a dose of 500 mg are used together.
Impact on laboratory parameters
The drug Xarelto® affects parameters of blood coagulation (prothrombin time, ACTV, Hep-Test®) due to its mechanism of action.
Special Instructions
Special Instructions
The use of Xarelto® is not recommended in patients receiving concomitant systemic treatment with azole antifungals (e.g. ketoconazole) or HIV protease inhibitors (e.g. ritonavir). These drugs are strong inhibitors of CYP3A4 and P-glycoprotein. Thus, these drugs may increase plasma concentrations of rivaroxaban to clinically significant levels (2.6-fold on average), which may lead to an increased risk of bleeding. However, the azole antifungal drug fluconazole, a moderate CYP3A4 inhibitor, has a less pronounced effect on rivaroxaban exposure and can be used simultaneously with it.
Xarelto® should be used with caution in patients with moderate renal impairment (CKR 49-30 ml/min) receiving concomitant drugs that may increase plasma concentrations of rivaroxaban. In patients with renal impairment at KC <30 ml/min, plasma concentrations of rivaroxaban may be significantly increased (1.6 times on average), which may lead to an increased risk of bleeding. Therefore, due to the presence of the indicated underlying disease, these patients have an increased risk of developing both bleeding and thrombosis. Due to limited clinical data, Xarelto® should be used with caution in patients with a CK of 29-15 ml/min. There are no clinical data on the use of rivaroxaban in patients with severe renal impairment (CKR <15 ml/min). Therefore, the use of Xarelto® is not recommended in these patients.
Patients with severe renal impairment or increased risk of bleeding, as well as patients receiving concomitant systemic treatment with azole antifungal agents or HIV protease inhibitors should be monitored closely for signs of bleeding after initiation of treatment.
Xarelto®, like other antithrombotic agents, should be used with caution in patients with an increased risk of bleeding, including:
Patients with a congenital or acquired tendency to bleed;
Patients with uncontrolled severe arterial hypertension;
-Patients with gastric or duodenal ulcer in the acute phase;
Patients who have recently had a gastric or duodenal ulcer;
-Patients with vascular retinopathy;
Patients who have recently had intracranial or intracerebral hemorrhage;
Patients with cerebral or spinal vascular disease;
Patients who have recently had brain, spinal cord, or eye surgery;
Patients with a history of bronchiectasis or pulmonary bleeding.
Caution should be exercised if the patient is concomitantly receiving medications that affect hemostasis, such as NSAIDs, platelet aggregation inhibitors, or other antithrombotic drugs.
Patients at risk for gastric and duodenal ulcers may be prescribed appropriate prophylactic treatment.
If there is an unexplained decrease in hemoglobin or BP, look for the source of the bleeding.
The safety and efficacy of Xarelto® in patients with artificial heart valves has not been studied, therefore, there is no data to support that Xarelto® 20 mg (15 mg in patients with CK of 49-15 ml/min) provides sufficient anticoagulant effect in this category of patients.
Xarelto® is not recommended as an alternative to unfractionated heparin in patients with hemodynamically unstable pulmonary embolism or in patients who may require thrombolysis or thrombectomy because the safety and efficacy of Xarelto® in these clinical situations has not been established.
If an invasive procedure or surgery is necessary, Xarelto® should be discontinued at least 24 hours before the intervention and on the basis of a physician’s report.
If the procedure cannot be postponed, the increased risk of bleeding should be evaluated against the need for urgent intervention.
The administration of Xarelto® should be resumed after an invasive procedure or surgery, provided appropriate clinical signs and adequate hemostasis are present.
When performing epidural/spinal anesthesia or spinal tap in patients receiving platelet aggregation inhibitors to prevent thromboembolic complications, there is a risk of epidural or spinal hematoma, which may lead to prolonged paralysis.
The risk of these events is further increased by the use of a permanent epidural catheter or concomitant therapy with drugs that affect hemostasis. Traumatic epidural or spinal puncture or repeated puncture may also increase the risk.
Patients should be monitored for signs and symptoms of neurologic disorders (e.g., numbness or weakness in the legs, bowel or bladder dysfunction). Urgent diagnosis and treatment is needed if neurological disorders are found.
The physician should weigh the potential benefit against the relative risk before spinal intervention in patients receiving anticoagulants or who are scheduled to receive anticoagulants for thrombosis prevention. There is no experience with the clinical use of rivaroxaban at doses of 15 mg and 20 mg in the situations described.
In order to reduce the potential risk of bleeding associated with concomitant use of rivaroxaban and epidural/spinal anesthesia or spinal tap, the pharmacokinetic profile of rivaroxaban should be considered. Placement or removal of an epidural catheter or lumbar puncture is best performed when the anticoagulant effect of rivaroxaban is judged to be weak. However, the exact time to achieve a sufficiently low anticoagulant effect in each patient is unknown.
Based on general pharmacokinetic characteristics, the epidural catheter should be withdrawn after at least twice the T1/2, that is, no earlier than 18 h after the last dose of Xarelto® for younger patients and no earlier than 26 h for elderly patients. Xarelto® should be administered not earlier than 6 hours after removal of the epidural catheter.
In case of traumatic puncture, Xarelto® administration should be delayed for 24 h.
Safety data from preclinical studies
With the exception of effects associated with enhanced pharmacological action (bleeding), no specific hazards to humans were found in the analysis of preclinical data from pharmacological safety studies.
Impact on driving and operating machinery
In the use of Xarelto® there have been cases of fainting and dizziness. Patients who have these adverse reactions should not drive vehicles or operate moving machinery.
Features
Features
Introduction
Rivaroxaban is rapidly absorbed; Cmax is reached 2-4 h after taking the tablet. The absolute bioavailability of rivaroxaban after a dose of 10 mg is high (80-100%). No AUC and Cmax changes are observed when rivaroxaban 10 mg is taken with food. The pharmacokinetics of rivaroxaban are characterized by moderate individual variability; individual variability (coefficient of variation) ranges from 30% to 40%.
A 66% bioavailability was observed when the drug was taken at an empty stomach dose of 20 mg, due to the reduced degree of absorption. Administration of Xarelto® in dose 20 mg with meal showed increase of average AUC by 39% in comparison with fasting dose, showing almost complete absorption and high bioavailability.
The absorption of rivaroxaban depends on the site of release in the GI tract. Reductions in AUC and Cmax of 29% and 56%, respectively, compared to whole tablet administration were observed when rivaroxaban pellet was released in the distal small intestine or the ascending colon. Administration of rivaroxaban in the GI tract distal to the stomach should be avoided because it may result in reduced absorption and, therefore, exposure to the drug.
The study evaluated the bioavailability (AUC and Cmax) of rivaroxaban taken orally at a dose of 20 mg as a crushed tablet mixed with apple puree or suspended in water and administered through a gastric tube followed by a liquid meal, compared to taking a whole tablet. The results demonstrated a predictable dose-dependent pharmacokinetic profile of rivaroxaban, with bioavailability at the above doses consistent with that of lower-dose rivaroxaban.
Distribution
In humans, most of rivaroxaban (92-95%) binds to plasma proteins, with serum albumin being the major binding component. Vd is moderate, Vss is approximately 50L.
Metabolism
On oral administration, approximately 2/3 of the administered dose of rivaroxaban is metabolized and subsequently excreted in equal amounts in the urine and feces. The remaining 1/3 of the dose is excreted via direct renal excretion unchanged, primarily through active renal secretion.
Rivaroxaban is metabolized by CYP3A4, CYP2J2 isoenzymes as well as by mechanisms independent of the cytochrome system. The main sites of biotransformation are oxidation of the morpholine group and hydrolysis of the amide bonds.
In vitro data show that rivaroxaban is a substrate for P-gp (P-glycoprotein) and Vsgp (breast cancer resistance protein) carrier proteins.
Unchanged rivaroxaban is the only active compound in plasma; no significant or active circulating metabolites were detected in plasma.
Elimination
Rivaroxaban, with a systemic clearance of approximately 10 L/h, may be classified as a low clearance drug.
In plasma excretion of rivaroxaban, the final T1/2 is 5 to 9 h in young patients.
Pharmacokinetics in Special Clinical Cases
In elderly patients, the plasma concentrations of rivaroxaban are higher than in younger patients; the average AUC is approximately 1.5 times greater than in younger patients, primarily due to seemingly lower total and renal clearance. In plasma excretion of rivaroxaban, the final T1/2 in elderly patients is 11 to 13 h.
There are no clinically significant differences in pharmacokinetics between men and women.
High or low body weight (less than 50 kg and more than 120 kg) only slightly affects the plasma concentration of rivaroxaban (less than 25% difference).
There are no data on pharmacokinetics in children.
There were no clinically significant differences in pharmacokinetics and pharmacodynamics in patients of Caucasian, Negroid, Asian, Hispanic, Japanese or Chinese ethnicity.
The effect of hepatic impairment on the pharmacokinetics of rivaroxaban has been studied in patients graded according to the Child-Pugh classification (according to standard procedures in clinical trials). The Child-Pugh classification provides an assessment of the prognosis of chronic liver disease, mainly cirrhosis. In patients scheduled for anticoagulant therapy, the most important consequence of impaired liver function is reduced synthesis of clotting factors in the liver. Because this index corresponds to only one of the five clinical/biochemical criteria that make up the Child-Pugh classification, the risk of bleeding does not correlate clearly with this classification. Treatment of such patients with anticoagulants should be decided regardless of the Child-Pugh classification.
Xarelto® is contraindicated in patients with liver disease with coagulopathy that causes clinically significant bleeding risk.
In patients with cirrhosis with mild hepatic impairment (Child-Pugh Class A) the pharmacokinetics of rivaroxaban were only slightly different from those in healthy controls (on average there was 1.2-fold AUC increase of rivaroxaban). There were no significant differences in pharmacodynamic properties between the groups.
In patients with cirrhosis and moderate hepatic impairment (Child-Pugh class B), the mean AUC of rivaroxaban was significantly increased (2.3-fold) compared to healthy volunteers due to significantly reduced drug clearance indicating severe liver disease. Suppression of factor Xa activity was more pronounced (2.6-fold) than in healthy volunteers. Prothrombin time was also 2.1 times that of healthy volunteers. Prothrombin time measurement assesses the external coagulation pathway, which includes clotting factors VII, X, V, II and I, which are synthesized in the liver. Patients with moderate hepatic impairment are more sensitive to rivaroxaban, which is a consequence of a closer relationship between pharmacodynamic effects and pharmacokinetic parameters, especially between concentration and prothrombin time.
There are no data for patients with Child-Pugh class C hepatic impairment.
In patients with renal impairment, increased exposure to rivaroxaban was observed inversely proportional to the degree of decreased renal function as assessed by CK.
In patients with renal impairment, a 1.4-, 1.5-, and 1.6-fold increase in plasma concentrations (AUC) of rivaroxaban, respectively, was observed in CKD 80-50 ml/min, CK 49-30 ml/min, and CK 29-15 ml/min compared with healthy volunteers. The corresponding increase in pharmacodynamic effects was more pronounced.
In patients with CK 80-50 mL/min, CK 49-30 mL/min, and CK 29-15 mL/min, total suppression of factor Xa activity was increased 1.5, 1.9, and 2-fold compared with healthy volunteers; prothrombin time due to factor Xa activity was also increased 1.3, 2.2, and 2.4-fold, respectively.
The data on the use of Xarelto® in patients with an IQ of 29-15 ml/min are limited, and therefore caution should be exercised when using the drug in this patient population. There is no data available about Xarelto® administration in patients with IQ of <15 ml/min, therefore it is not recommended to use the drug in this category of patients.
Contraindications
Contraindications
– hypersensitivity to rivaroxaban or any excipients of the drug;
– clinically significant active bleeding (e.g., intracranial bleeding, gastrointestinal bleeding);
– an injury or condition associated with an increased risk of major bleeding, such as an existing or recent gastrointestinal ulcer, the presence of malignant tumors with a high risk of bleeding, recent trauma to the brain or spinal cord, brain, spinal cord or eye surgery, intracranial bleeding, diagnosed or suspected esophageal varices, arteriovenous malformations, vascular aneurysms or pathology of cerebral or spinal cord vessels;
Side effects
Side effects
The safety of Xarelto® has been evaluated in four phase III studies involving 6097 patients who underwent major orthopedic lower extremity surgery (total knee or hip replacement) and 3997 patients hospitalized for medical reasons, treated with Xarelto® at a dose of 10 mg for up to 39 days and in three phase III trials of venous thromboembolism including 4556 patients receiving Xarelto® at a dose of either 15 mg twice daily for 3 weeks, followed by a dose of 20 mg once daily, or 20 mg once daily with a treatment duration up to 21 months.
In addition, safety data were available from two phase III studies involving 7,750 patients in patients with non-valvular atrial fibrillation who received at least one dose of Xarelto® for up to 41 months and 10,225 patients with ACS who received at least one dose of Xarelto® 25 mg (2 times/day) or 5 mg (2 times/day) in addition to therapy with acetylsalicylic acid or acetylsalicylic acid with clopidogrel or ticlopidine, duration of treatment up to 31 months.
Because of the mechanism of action, use of Xarelto® may be accompanied by an increased risk of occult or overt bleeding from any organs and tissues, which may lead to post-hemorrhagic anemia. The risk of bleeding may increase in patients with uncontrolled arterial hypertension and/or when co-administered with drugs that affect hemostasis. Signs, symptoms and severity (including possible death) vary depending on the location, intensity or duration of bleeding and/or anemia. Hemorrhagic complications may be manifested by weakness, pallor, dizziness, headache, shortness of breath, and limb enlargement or shock, which cannot be explained by other causes. In some cases, symptoms of myocardial ischemia, such as chest pain and angina, have developed due to anemia.
Known complications secondary to severe bleeding, such as compartment syndrome and renal failure due to hypoperfusion, have also been reported with Xarelto®. Thus, the possibility of bleeding should be considered in the evaluation of any patient receiving anticoagulants.
The frequency of adverse reactions reported for Xarelto® is summarized below. In groups divided by frequency, adverse effects are presented in decreasing order of severity as follows: frequently: â¥1% to < 10% (â¥1/100 to < 1/10); infrequently: â¥0.1% to < 1% (â¥1/1000 to < 1/100); rare: â¥0.01% to < 0.1% (â¥1/10,000 to < 1/1000); very rare: < 0.01% (< 1/10,000).
All adverse reactions occurred during treatment in patients enrolled in phase III clinical trials
Hematopoietic system: frequently – anemia (including appropriate laboratory parameters); infrequently – thrombocythemia (including increased platelet count)*.
Cardiovascular system: frequently – significant decrease of BP, hematoma; infrequently – tachycardia.
Visual system disorders: often – ocular hemorrhage (including conjunctival hemorrhage).
The digestive system: frequently – bleeding gums, gastrointestinal bleeding (including rectal bleeding), gastrointestinal pain, dyspepsia, nausea, constipation*, diarrhea, vomiting*; infrequently – dry mouth.
Systemic disorders and reactions at the site of administration: frequently, fever*, peripheral edema, decreased overall muscle strength and tone (including weakness, asthenia); infrequently, worsening of general well-being (including malaise); rarely, local edema*.
Hepatic disorders: infrequent – impairment of liver function; rarely – jaundice.
Results of studies: frequent – increased liver transaminase activity; infrequent – increased bilirubin concentration, increased ALT activity*, increased LDH activity*, increased lipase activity*, increased amylase activity*, increased GGT activity*; rare – increased concentration of conjugated bilirubin (with or without accompanying increase in ALT activity).
Nervous system disorders: frequently – dizziness, headache; infrequent – intracerebral and intracranial hemorrhage, transient fainting.
Urogenital system disorders: often – bleeding from the urogenital tract (including hematuria and menorrhagia**), renal failure (including increased concentration of creatinine, increased concentration of urea)*.
Respiratory system disorders: often – nasal bleeding, hemoptysis.
Skin and subcutaneous tissue disorders: frequently – itching (including infrequent cases of generalized itching), rash, ecchymosis, cutaneous and subcutaneous hemorrhage; infrequently – urticaria.
Immune system disorders: infrequent allergic reactions, allergic dermatitis.
Muscular system: often – pain in the extremities *; infrequent – hemarthrosis; rarely – bleeding into the muscles.
Systemic disorders and reactions at the site of administration: frequently – fever*, peripheral edema, worsening of general well-being (including weakness, asthenia); infrequently – worsening of general well-being (including malaise); rarely – local edema*.
Trauma, poisoning and procedural complications: often – hemorrhage after procedures (including postoperative anemia and wound bleeding), excessive hematoma when bruised; infrequent – discharge from the wound*; rarely – vascular pseudoaneurysm***.
* have been reported after major orthopedic surgery.
**reported in VTE treatment as very frequent in women < 55 years of age.
*** were reported as infrequent in the prevention of sudden death and myocardial infarction in patients after acute coronary syndrome (after percutaneous interventions).
In post-registration monitoring, the following adverse reactions have been reported that were temporally associated with the use of Xarelto®. It is not possible to estimate the incidence of these adverse reactions in post-registration monitoring.
Immune system disorders: angioedema, allergic edema. In RCT phase III such adverse effects were considered infrequent (>1/1000 to <1/100).
Hepatic disorders: cholestasis, hepatitis (including hepatocellular damage). In a phase III RCT, such adverse effects were considered rare (>1/10,000 to <1/1000).
Hematopoietic system: thrombocytopenia. In a phase III RCT, such adverse effects were considered infrequent (>1/1000 to < 1/100).
Muscular system disorders: frequency is unknown – increased subfascial pressure syndrome (compartment syndrome) due to muscle hemorrhage.
Relinary system disorders: frequency unknown – renal failure/acute renal failure due to bleeding leading to renal hypoperfusion.
Overdose
Overdose
Rare cases of overdose have been reported when taking rivaroxaban up to 600 mg without the development of bleeding or other adverse reactions. Due to limited absorption, a low-level plateau of drug concentrations is expected with no further increase in mean plasma concentrations when administered in doses higher than the therapeutic (â¥50 mg).
Treatment
The specific antidote of rivaroxaban is unknown. In case of overdose, activated charcoal may be used to reduce absorption of rivaroxaban. Given the intense binding to plasma proteins, rivaroxaban is not expected to be excreted by dialysis.
If a patient receiving rivaroxaban has a bleeding complication, the next administration of the drug should be delayed or, if necessary, treatment with this drug should be discontinued. The T1/2 of rivaroxaban leaves approximately 5-13 h. The treatment should be chosen individually according to the severity and localization of bleeding.
If necessary, appropriate symptomatic treatment, such as mechanical compression (e.g., in severe nasal bleeding), surgical hemostasis with assessment of its effectiveness, infusion therapy and hemodynamic support, use of blood products (red blood cell mass or fresh frozen plasma, depending on concomitant anemia or coagulopathy) or platelets may be used.
If the above measures do not eliminate bleeding, specific procoagulant drugs of reverse action may be prescribed, such as clotting factors II, VII, IX and X in combination[Prothrombin complex], anti-inhibitor coagulant complex or eptacog alpha [activated]. However, there is currently very limited experience with these drugs in patients receiving Xarelto®.
Protamine sulfate and vitamin K are not expected to affect the anticoagulant activity of rivaroxaban.
There is limited experience with tranexamic acid and no experience with aminocaproic acid and aprotinin in patients receiving Xarelto®. There is no scientific justification for or experience with the systemic hemostatic drug desmopressin in patients receiving Xarelto®.
Additional information
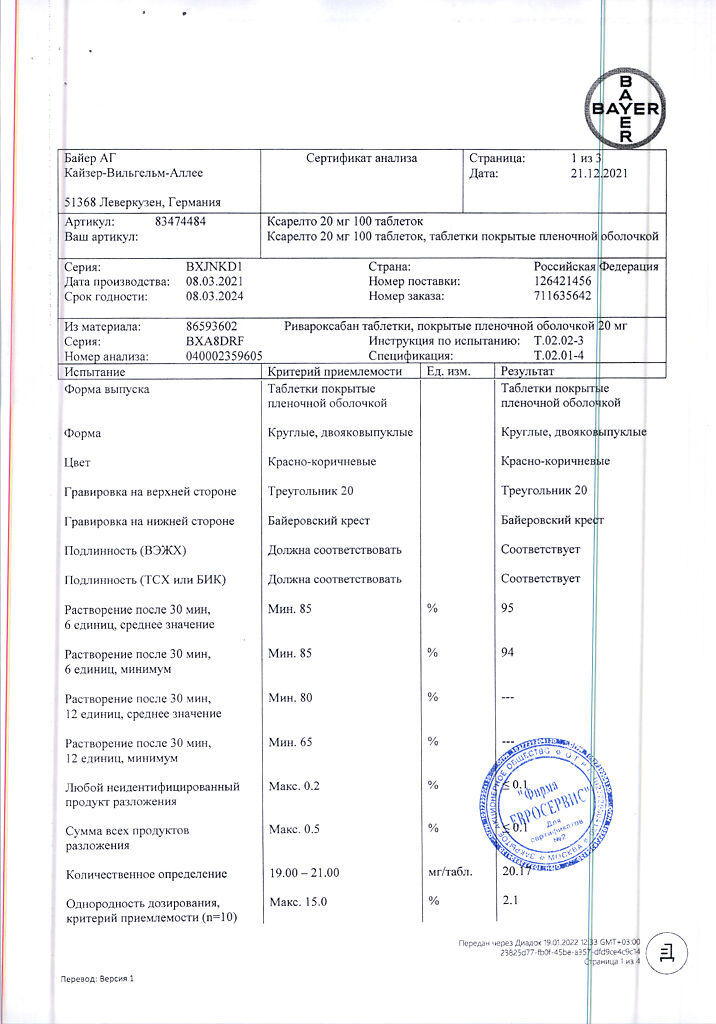
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Bayer AG, Germany |
| Medication form | pills |
| Brand | Bayer AG |
Other forms…
Related products
Buy Xarelto, 20 mg 100 pcs with delivery to USA, UK, Europe and over 120 other countries.