No products in the cart.
Xarelto, 10 mg 30 pcs
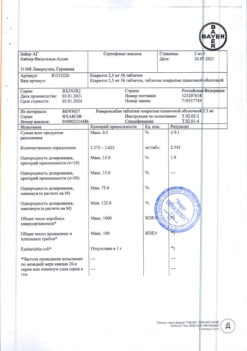
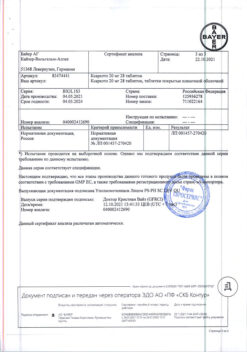
€103.78 €86.49
Description
Rivaroxaban is a highly selective direct factor Xa inhibitor with high bioavailability when administered orally. Activation of factor X with the formation of factor Xa through the internal and external clotting pathways plays a central role in the coagulation cascade. Factor Xa is a component of the forming prothrombinase complex, the action of which leads to the conversion of prothrombin to thrombin. As a result, these reactions lead to the formation of fibrin thrombus and platelet activation by thrombin. One molecule of factor 2 Xa catalyzes the formation of more than 1,000 molecules of thrombin, which has been called the “thrombin burst”.
Indications
Indications
Prevention of venous thromboembolism (VTE) in patients undergoing major orthopedic surgery on the lower extremities.
Prevention of recurrence of deep vein thrombosis (DVT) or pulmonary embolism (PE) after at least 6 months of treatment for DVT or PE.
Pharmacological effect
Pharmacological effect
Rivaroxaban is a highly selective direct factor Xa inhibitor with high oral bioavailability. Activation of factor X to form factor Xa through the intrinsic and extrinsic coagulation pathways plays a central role in the coagulation cascade. Factor Xa is a component of the developing prothrombinase complex, the action of which leads to the conversion of prothrombin to thrombin. As a result, these reactions lead to the formation of a fibrin thrombus and activation of platelets by thrombin. One molecule of factor 2 Xa catalyzes the formation of more than 1000 molecules of thrombin, which is called the “thrombin burst”.
Special instructions
Special instructions
Antithrombotic drugs, including rivaroxaban, should be used with caution in the treatment of patients with an increased risk of bleeding.
In patients with severe renal impairment (CrCl < 30 ml/min), plasma concentrations of rivaroxaban may be significantly increased, which may lead to an increased risk of bleeding. Due to the underlying disease, these patients are at increased risk of both bleeding and thrombosis.
The use of rivaroxaban has not been studied in clinical trials during surgery for hip fractures.
If there is an unexplained decrease in hemoglobin or blood pressure, it is necessary to look for the source of bleeding.
No prolongation of the QT interval was observed during treatment with rivaroxaban.
When performing lumbar puncture and epidural/spinal anesthesia in patients receiving platelet aggregation inhibitors to prevent thromboembolic complications, there is a risk of developing epidural or spinal hematoma, which can lead to long-term paralysis. The risk of these events is further increased by the use of indwelling catheters or concomitant use of drugs that affect hemostasis.
Trauma during epidural or spinal puncture or repeat puncture may also increase the risk. Patients should be monitored for signs or symptoms of neurological impairment (eg, numbness or weakness of the legs, bowel or bladder dysfunction).
If neurological disorders are detected, urgent diagnosis and treatment are necessary. Physicians should weigh the potential benefits and risks before performing spinal surgery in patients receiving or about to receive anticoagulants to prevent thrombosis. The epidural catheter should be removed no earlier than 18 hours after the last dose of rivaroxaban. Rivaroxaban should not be administered earlier than 6 hours after removal of the epidural catheter. In case of traumatic puncture, the administration of rivaroxaban should be postponed for 24 hours.
If an invasive procedure or surgery is necessary, Xarelto should be discontinued at least 24 hours before the procedure and based on the doctor’s opinion.
If the procedure cannot be delayed, the increased risk of bleeding should be weighed against the need for urgent intervention.
Xarelto should be restarted after an invasive procedure or surgery, provided appropriate clinical indicators and adequate hemostasis are present.
Use for liver dysfunction
Rivaroxaban is contraindicated in patients with liver disease associated with coagulopathy that carries a clinically significant risk of bleeding. Patients with other liver diseases do not require dose changes.
Available limited clinical data obtained in patients with moderate hepatic impairment (class B according to the Child-Pugh classification) indicate a significant increase in the pharmacological activity of the drug. For patients with severe hepatic impairment (Child-Pugh class C), clinical data are not available.
Use for renal impairment
When prescribing rivaroxaban to patients with mild (creatinine clearance 80-50 ml/min) or moderate (creatinine clearance <50-30 ml/min) renal failure, no dose reduction is required.
Available limited clinical data obtained in patients with severe renal impairment (creatinine clearance <30-15 ml/min) show a significant increase in rivaroxaban concentrations in these patients. Rivaroxaban should be used with caution in treating this category of patients.
The use of rivaroxaban is not recommended in patients with CC < 15 ml/min.
Safety data obtained from nonclinical studies
With the exception of effects associated with enhanced pharmacological action (bleeding), analysis of preclinical data obtained in pharmacological safety studies did not reveal any specific hazard to humans.
Impact on the ability to drive vehicles and machinery
Studies of the effect of rivaroxaban on the ability to drive vehicles and work with potentially dangerous moving mechanisms have not been conducted.
In the postoperative period, cases of fainting and dizziness were reported infrequently. Patients who experience these adverse reactions should not drive vehicles or operate moving machinery.
Active ingredient
Active ingredient
Rivaroxaban
Composition
Composition
1 film-coated tablet contains:
active ingredient:
Pregnancy
Pregnancy
Contraindicated for children under 18 years of age, pregnant women and lactation.
Pregnancy
There are no data on the use of rivaroxaban in pregnant women.
Data obtained in experimental animals have shown pronounced maternal toxicity of rivaroxaban, associated with the pharmacological action of the drug (for example, complications in the form of hemorrhages) and leading to reproductive toxicity.
Due to the possible risk of bleeding and ability to cross the placenta, rivaroxaban is contraindicated during pregnancy.
Women with preserved reproductive capacity should use effective methods of contraception during treatment with rivaroxaban.
Lactation
There are no data on the use of rivaroxaban for the treatment of women during lactation.
Data obtained in experimental animals show that rivaroxaban is excreted in breast milk. Rivaroxaban can only be used after breastfeeding has been stopped.
Contraindications
Contraindications
Hypersensitivity to rivaroxaban or any of the excipients contained in the tablet.
Clinically significant active bleeding (eg, intracranial bleeding, gastrointestinal bleeding).
Injury or condition associated with an increased risk of major bleeding (eg, current or recent gastrointestinal ulcer, presence of malignancies with a high risk of bleeding, recent brain or spinal cord injury, recent brain, spinal cord or eye surgery, recent intracranial hemorrhage, diagnosed or suspected esophageal varices, arteriovenous malformations, vascular aneurysms or large anomalies in the structure of blood vessels in the brain or spinal cord).
Concomitant therapy with any other anticoagulants, for example, unfractionated heparin (UFH), low molecular weight heparins (enoxaparin, dalteparin, etc.), heparin derivatives (fondaparinux, etc.), oral anticoagulants (warfarin, apixaban, dabigatran, etc.), except in cases where the patient is transferred from therapy or to drug therapy Xarelto®, or when UFH is prescribed in low doses to maintain the patency of a central venous or arterial catheter.
Liver diseases associated with coagulopathy that pose a clinically significant risk of bleeding, including patients with Child-Pugh class B and C cirrhosis.
Pregnancy and breastfeeding period.
Children and adolescents up to 18 years of age (efficacy and safety in patients in this age group have not been established).
Severe renal impairment (CrCl < 15 ml/min) (there are no clinical data on the use of rivaroxaban in this category of patients).
Hereditary lactose or galactose intolerance (for example, congenital lactase deficiency or glucose-galactose malabsorption) because this medicinal product contains lactose.
WITH CAUTION
The drug should be used with caution:
In the treatment of patients with an increased risk of bleeding (including congenital or acquired tendency to bleeding, uncontrolled severe arterial hypertension, gastric and duodenal ulcers in the acute stage, recently suffered gastric and duodenal ulcers, vascular retinopathy, recently suffered intracranial or intracerebral hemorrhage, with pathology of the vessels of the spinal cord or brain, after recently previous surgery on the brain, spinal cord or eyes, with a history of bronchiectasis or pulmonary hemorrhage).
When treating patients with moderate renal impairment (CrCl 30-49 ml/min) who are simultaneously receiving drugs that increase the concentration of rivaroxaban in the blood plasma (see section “Interaction with other drugs”).
When treating patients with severe renal impairment (ClCr15-29 ml/min) (see section “Special Instructions”).
Rivaroxaban is not recommended for use in patients receiving systemic treatment with azole antifungals (for example, ketoconazole) or HIV protease inhibitors (for example, ritonavir) (see sections “Interaction with other drugs”, “Special instructions”).
Patients with severe renal impairment (CrCl 15-29 ml/min), an increased risk of bleeding, and patients receiving concomitant systemic treatment with azole antifungals or HIV protease inhibitors should be closely monitored after initiation of treatment for timely detection of complications in the form of bleeding. Such monitoring may include regular physical examination of patients, 8 close monitoring of surgical wound drainage, and periodic measurements of hemoglobin levels. Any decrease in hemoglobin or blood pressure for which there is no explanation is grounds for searching for the source of bleeding.
In patients receiving concomitant medications that affect hemostasis, such as nonsteroidal anti-inflammatory drugs (NSAIDs), antiplatelet agents, other antithrombotics or selective serotonin reuptake inhibitors (SSRIs) and selective serotonin norepinephrine reuptake inhibitors (SNRIs).
In patients at risk of exacerbation of gastric and duodenal ulcers, prophylactic antiulcer treatment may be justified.
Side Effects
Side Effects
The safety of Xarelto® was assessed in four phase III studies involving 6097 patients undergoing major lower extremity orthopedic surgery (total knee or total hip replacement) and 3997 medically hospitalized patients treated with Xarelto® 10 mg for up to 39 days, and in three phase III studies for the treatment of venous thromboembolism, including 4566 patients receiving Xarelto® either 15 mg twice daily for 3 weeks followed by 20 mg once daily or 20 mg once daily for up to 21 months.
In addition, two phase III studies, including 7,750 patients, provided safety data in patients with non-valvular atrial fibrillation who received at least one dose of Xarelto® for up to 41 months, as well as 10,225 patients with ACS who received at least one dose of 2.5 mg (2 times / day) or 5 mg (2 times / day). Xarelto® in addition to therapy with acetylsalicylic acid or acetylsalicylic acid with clopidogrel or ticlopidine, treatment duration up to 31 months.
Given the mechanism of action, the use of Xarelto may be accompanied by an increased risk of latent or overt bleeding from any organs and tissues, which can lead to posthemorrhagic anemia. The risk of bleeding may increase in patients with uncontrolled arterial hypertension and/or when used together with drugs that affect hemostasis.
Signs, symptoms, and severity (including possible death) vary depending on the location, intensity, or duration of bleeding and/or anemia.
Hemorrhagic complications can manifest as weakness, pallor, dizziness, headache, shortness of breath, as well as enlargement of the limb or shock, which cannot be explained by other reasons. In some cases, symptoms of myocardial ischemia, such as chest pain and angina, developed as a result of anemia.
Known complications secondary to severe bleeding, such as interfascial space syndrome and renal failure, have been reported with Xarelto®. Therefore, the possibility of bleeding should be considered when assessing the condition of a patient receiving anticoagulants.
A summary of the incidence of adverse reactions reported for Xarelto® is given below. In groups divided by frequency, undesirable effects are presented in order of decreasing severity, as follows: very often (≥1/10); often (≥1/100 and <1/10); uncommon (≥1/1000 and <1/100); rare (≥1/10,000 and <1/1000).
All adverse reactions that occurred during treatment in patients participating in phase III clinical trials
From the hematopoietic system: often – anemia (including relevant laboratory parameters); uncommon – thrombocythemia (including elevated platelet counts)*.
From the cardiovascular system: often – marked decrease in blood pressure, hematoma; infrequently – tachycardia.
From the organ of vision: often – hemorrhage in the eye (including hemorrhage in the conjunctiva).
From the digestive system: often – bleeding gums, gastrointestinal bleeding (including rectal bleeding), pain in the gastrointestinal tract, dyspepsia, nausea, constipation*, diarrhea, vomiting*; infrequently – dry mouth.
From the liver: infrequently – impaired liver function; rarely – jaundice.
From laboratory parameters: often – increased activity of liver transaminases; infrequently – increased bilirubin concentration, increased alkaline phosphatase activity*, increased LDH activity*, increased lipase activity*, increased amylase activity*, increased GGT activity*; rarely – an increase in the concentration of conjugated bilirubin (with or without a concomitant increase in ALT activity).
From the nervous system: often – dizziness, headache; infrequently – intracerebral and intracranial hemorrhage, short-term fainting.
From the genitourinary system: often – bleeding from the urogenital tract (including hematuria and menorrhagia**), renal failure (including increased creatinine concentration, increased urea concentration)*.
From the respiratory system: often – nosebleeds, hemoptysis.
From the skin and subcutaneous tissues: often – itching (including rare cases of generalized itching), rash, ecchymosis, skin and subcutaneous hemorrhages; infrequently – urticaria.
From the immune system: rarely – allergic reactions, allergic dermatitis.
From the musculoskeletal system: often – pain in the limbs*; infrequently – hemarthrosis; rarely – hemorrhage into the muscles.
From the body as a whole: often – fever*, peripheral edema, deterioration of general muscle strength and tone (including weakness, asthenia); infrequently – deterioration in general health (including malaise); rarely – local swelling*.
Other: often – hemorrhages after procedures (including postoperative anemia and bleeding from a wound), excessive hematoma from a bruise; infrequently – discharge from the wound*; rarely – vascular pseudoaneurysm***.
* – were registered after major orthopedic operations.
** – recorded during the treatment of VTE as very common in women <55 years of age.
*** – registered as infrequent in the prevention of sudden death and myocardial infarction in patients after acute coronary syndrome (after percutaneous interventions).
During post-marketing monitoring, cases of the following adverse reactions were reported, the development of which had a temporary connection with the use of Xarelto®. It is not possible to assess the frequency of occurrence of such adverse reactions within the framework of post-registration monitoring.
From the immune system: angioedema, allergic edema. In the phase III RCT, such adverse effects were considered infrequent (>1/1000 to <1/100).
From the liver: cholestasis, hepatitis (including hepatocellular damage). In the phase III RCT, such adverse effects were considered rare (>1/10,000 to <1/1000).
From the hematopoietic system: thrombocytopenia. In the phase III RCT, such adverse effects were considered infrequent (>1/1000 to <1/100).
From the musculoskeletal system: frequency unknown – increased subfascial pressure syndrome (compartment syndrome) due to hemorrhage into the muscles.
From the urinary system: frequency unknown – renal failure/acute renal failure due to bleeding leading to renal hypoperfusion.
Interaction
Interaction
Pharmacokinetic interaction
Rivaroxaban is eliminated primarily through hepatic metabolism mediated by the cytochrome P450 system (CYP3A4, CYP2J2), as well as through renal excretion of unchanged drug using the P-gp/Bcrp (P-glycoprotein/breast cancer resistance protein) transporter systems.
Rivaroxaban does not suppress or induce the CYP3A4 isoenzyme and other important cytochrome isoforms.
Concomitant use of rivaroxaban and strong inhibitors of CYP3A4 and P-glycoprotein may result in decreased renal and hepatic clearance and thus significantly increase systemic exposure.
The combined use of rivaroxaban and the azole antifungal agent ketoconazole (400 mg 1 time / day), which is a strong inhibitor of CYP3A4 and P-glycoprotein, led to an increase in the average steady-state AUC of rivaroxaban by 2.6 times and an increase in the average Cmax of rivaroxaban by 1.7 times, which was accompanied by a significant increase in the pharmacodynamic effect of the drug.
The combined use of rivaroxaban and the HIV protease inhibitor ritonavir (600 mg 2 times / day), which is a strong inhibitor of CYP3A4 and P-glycoprotein, led to an increase in the average steady-state AUC of rivaroxaban by 2.5 times and an increase in the average Cmax of rivaroxaban by 1.6 times, which was accompanied by a significant increase in the pharmacodynamic effect of the drug. Therefore, rivaroxaban is not recommended for use in patients receiving systemic treatment with azole antifungals or HIV protease inhibitors.
Other drugs that strongly inhibit only one of the pathways of rivaroxaban elimination, either CYP3A4 or P-glycoprotein, are expected to increase rivaroxaban plasma concentrations to less significant levels.
Clarithromycin (500 mg 2 times / day), a strong inhibitor of the CYP3A4 isoenzyme and a moderate inhibitor of P-glycoprotein, caused an increase in AUC values by 1.5 times and Cmax of rivaroxaban by 1.4 times. This increase is of the order of normal variability in AUC and Cmax and is considered clinically insignificant.
Erythromycin (500 mg 3 times/day), a moderate inhibitor of the CYP3A4 isoenzyme and P-glycoprotein, caused an increase in the AUC and Cmax values of rivaroxaban by 1.3 times. This increase is of the order of normal variability in AUC and Cmax and is considered clinically insignificant.
In patients with renal failure (creatinine clearance ≤ 80-50 ml/min), erythromycin (500 mg 3 times/day) caused an increase in rivaroxaban AUC by 1.8 times and Cmax by 1.6 times compared with patients with normal renal function who did not receive concomitant therapy. In patients with renal failure (creatinine clearance 50-30 ml/min), erythromycin caused an increase in rivaroxaban AUC by 2.0 times and Cmax by 1.6 times compared with patients with normal renal function who did not receive concomitant therapy.
Fluconazole (400 mg 1 time / day), a moderate inhibitor of the CYP3A4 isoenzyme, caused an increase in the average AUC of rivaroxaban by 1.4 times and an increase in the average Cmax by 1.3 times. This increase is of the order of normal variability in AUC and Cmax and is considered clinically insignificant.
Concomitant use of rivaroxaban with dronedarone should be avoided due to limited clinical data on coadministration.
Co-administration of rivaroxaban and rifampicin, a strong inducer of CYP3A4 and P-glycoprotein, resulted in a decrease in the mean AUC of rivaroxaban by approximately 50% and a parallel decrease in its pharmacodynamic effects. Concomitant use of rivaroxaban with other strong CYP3A4 inducers (eg, phenytoin, carbamazepine, phenobarbital or St. John’s wort) may also result in decreased rivaroxaban plasma concentrations. The decrease in plasma concentrations of rivaroxaban was considered clinically insignificant.
Pharmacodynamic interaction
After co-administration of enoxaparin sodium (single dose 40 mg) and rivaroxaban (single dose 10 mg), a net effect on anti-factor Xa activity was observed, without additional net effects on blood clotting tests (prothrombin time, aPTT). Enoxaparin did not change the pharmacokinetics of rivaroxaban.
After co-administration of rivaroxaban 15 mg and naproxen 500 mg, no clinically significant prolongation of bleeding time was observed. However, a more pronounced pharmacodynamic response is possible in some individuals.
No pharmacokinetic interaction was found between rivaroxaban at a dose of 15 mg and clopidogrel (loading dose of 300 mg followed by a maintenance dose of 75 mg), but in some patients a significant increase in bleeding time was found, which did not correlate with the degree of platelet aggregation and the content of P-selectin or GPIIb/IIIa receptor.
Switching patients from warfarin (IHO 2 to 3) to rivaroxaban (20 mg) or from rivaroxaban (20 mg) to warfarin (MHO 2 to 3) was associated with a more than additive increase in prothrombin time/INR (Neoplastin) (in some cases up to 12), while the effects of changes in aPTT, suppression of factor Xa activity and endogenous thrombin potential (ETP) were additive.
To assess the pharmacodynamic effects of Xarelto® during the transition period, anti-Factor Xa, PiCT and HepTest® tests can be performed if the parameters determined during the transition period are not affected by warfarin.
Starting on the 4th day after warfarin discontinuation, all tests (including PT, APTT, factor Xa suppression and EPT (endogenous thrombin potential)) reflected exclusively the effect of Xarelto®.
To assess the pharmacodynamic effects of warfarin during the transition period, the MHO measured at the time the Cmax of rivaroxaban is reached (24 hours after dosing of rivaroxaban) can be used, since at this point in time the effect of rivaroxaban on test results is minimal.
No pharmacokinetic interaction was detected between warfarin and rivaroxaban.
The drug interaction of Xarelto® with VKA phenindione has not been studied. It is recommended, whenever possible, to avoid transferring patients from Xarelto® therapy to VKA phenindione therapy and vice versa.
There is limited experience converting patients from VKA acenocoumarol therapy to Xarelto®.
If there is a need to transfer a patient from Xarelto® therapy to VKA therapy with phenindione or acenocoumarol, then special care should be taken; daily monitoring of the pharmacodynamic effect of the drugs (MHO, prothrombin time) should be carried out immediately before taking the next dose of Xarelto®. If there is a need to transfer a patient from VKA therapy with phenindione or acenocoumarol to therapy with Xarelto®, then special care should be taken; monitoring of the pharmacodynamic effect of the drugs is not required.
Concomitant use with other drugs
No clinically significant pharmacokinetic or pharmacodynamic interactions were observed when rivaroxaban was co-administered with midazolam (CYP3A4 substrate), digoxin (P-glycoprotein substrate) or atorvastatin (CYP3A4 and P-glycoprotein substrate).
No clinically significant interactions with food were observed.
Incompatibility
Unknown.
Effect on laboratory parameters
The effect on blood clotting parameters (PT, APTT, HepTest®) is consistent with what would be expected given the mechanism of action of Xarelto®.
Overdose
Overdose
Rare cases of overdose up to 600 mg have been reported without complications such as bleeding or other adverse reactions. Due to limited absorption, a saturation effect is expected without a further increase in the mean plasma concentration of rivaroxaban at hypertherapeutic doses of 50 mg or higher.
The specific antidote for rivaroxaban is unknown. In case of overdose, activated charcoal can be used to reduce the absorption of rivaroxaban. Given its extensive plasma protein binding, rivaroxaban is not expected to be eliminated by dialysis.
Treatment of bleeding
If a complication occurs in the form of bleeding, the next dose of the drug should be postponed or treatment should be canceled, depending on the situation. The half-life of rivaroxaban is approximately 5-13 hours. Treatment should be individualized according to the severity and location of bleeding.
If necessary, appropriate symptomatic treatment may be used, such as mechanical compression (eg, in cases of severe epistaxis), surgical hemostasis with bleeding control procedures, fluid resuscitation and hemodynamic support, the use of blood products (packed red blood cells or fresh frozen plasma, depending on the underlying anemia or coagulopathy) or platelets.
If the above measures do not resolve the bleeding, a specific procoagulant, such as prothrombin complex concentrate, activated prothrombin complex concentrate, or recombinant factor VIIa (rf VIIa), may be prescribed. However, to date, experience with the use of these drugs in the treatment of patients receiving rivaroxaban is very limited.
Protamine sulfate and vitamin K are not expected to affect the anticoagulant activity of rivaroxaban. There is limited experience with tranexamic acid and no experience with aminocaproic acid and aprotinin in patients receiving 20 Xarelto®. There is no scientific basis for or experience with the use of the systemic hemostatic drug desmopressin in patients receiving Xarelto®
Recommendations for use
Recommendations for use
Inside, regardless of food intake. If the patient is unable to swallow the tablet whole, the Xarelto® tablet may be crushed and mixed with water or a liquid food such as applesauce immediately before ingestion. A crushed Xarelto® tablet can be given through a gastric tube. The position of the probe in the gastrointestinal tract must be further agreed with the doctor before taking Xarelto®. The crushed tablet should be administered through a gastric tube in a small amount of water, after which a small amount of water should be injected in order to wash away any remaining drug from the walls of the tube.
Prevention of venous thromboembolism (VTE) in patients undergoing major orthopedic surgery on the lower extremities.
In order to prevent VTE during major orthopedic operations, it is recommended to prescribe 1 tablet of 10 mg 1 time per day. Duration of treatment:
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C.
Shelf life
Shelf life
3 years
Do not use after expiration date.
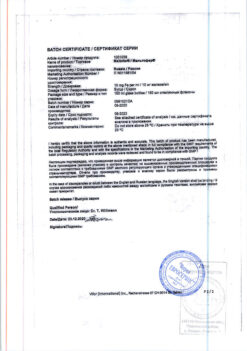
Manufacturer
Manufacturer
Bayer AG, Germany
Additional information
| Shelf life | 3 years Do not use after the expiration date. |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 ° C. |
| Manufacturer | Bayer AG, Germany |
| Medication form | pills |
| Brand | Bayer AG |
Other forms…
Related products
Buy Xarelto, 10 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.