No products in the cart.
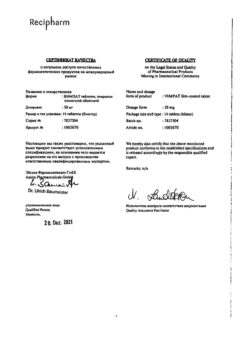
Vimpat, 100 mg 14 pcs
€30.46 €26.40
Description
Pharmacodynamics
The active substance, lacosamide (R-2-acetamido-N-benzyl-3-methoxypropionamide), is a functionalized amino acid.
The exact mechanism of the antiepileptic action of lacosamide has not been established. In in vitro electrophysiological studies, lacosamide enhances the slow inactivation of potential-dependent sodium channels selectively, leading to stabilization of hyperexcitable neuronal membranes.
Lacosamide prevented the development of seizures of partial and primary generalized epilepsy in most animal models and also delayed the development of increased seizure readiness. In preclinical studies, lacosamide in interaction with levetiracetam, carbamazepine, phenytoin, valproate, lamotrigine, topiramate or gabapentin showed synergistic additive anticonvulsant effects.
Clinical efficacy and safety
The efficacy of Vimpat® as adjunctive therapy at recommended doses (200, 400 mg/day) has been proven in 3 multicenter, randomized, placebo-controlled clinical trials with a 12-week maintenance period. The efficacy of Vimpat® at a dose of 600 mg/day has also been demonstrated in controlled, additional therapeutic studies, although efficacy was comparable to the 400 mg/day dose, but tolerability of this dose (600 mg/day) was worse because of CNS and GI side effects. Therefore, the use of 600 mg/day is not recommended. The maximum recommended dose is 400 mg/day. These studies involving 1308 patients with a history of partial seizures over a mean period of 23 years were designed to evaluate the efficacy and safety of lacosamide with concomitant administration of 1-3 antiepileptic drugs in patients with uncontrolled partial seizures with or without secondary generalization. The overall proportion of patients with a 50% reduction in seizure frequency in the placebo, lacosamide 200 mg/day, and lacosamide 400 mg/day groups was 23, 34, and 40%, respectively.
There is currently insufficient data on the feasibility of withdrawing concomitant antiepileptic medications for the use of lacosamide monotherapy.
The pharmacokinetics and safety of a single saturation dose of infused lacosamide were determined in a multicenter open-label safety and tolerability study of rapid initiation of lacosamide therapy using a single IV saturation dose (200 mg), followed by oral administration of the drug twice daily (at a dose equivalent to the IV dose) as adjunctive therapy in adult patients 16 to 60 years old with partial seizures.
Pharmacokinetics
Intake
The infusion solution. Cmax is reached by the time the infusion is completed. Plasma concentrations of lacosamide increase in proportion to dose after IV (50-300 mg) administration.
The film-coated tablets. Lacosamide is quickly and completely absorbed after oral administration. Bioavailability of lacosamide in tablets is approximately 100%. After oral administration, plasma concentration of lacosamide increases rapidly, Tmax is 0.5-4 h. Food intake does not affect the rate and extent of absorption.
Distribution
Vd is approximately 0.6 l/kg, the degree of binding to plasma proteins is less than 15%.
Metabolism
95% of lacosamide is excreted through the kidneys unchanged (about 40%) and as O-desmethylmetabolite (less than 30%). The polar fraction (presumably serine derivatives) is approximately 20% in the urine and only in small amounts (0-2%) detected in plasma. Other metabolites are detected in the urine in amounts of 0.5-2%.
In vitro data show that formation of O-desmethylmetabolite occurs mainly under the action of CYP2C19, 2C9 and 3A4 cytochrome isoenzymes. When comparing the pharmacokinetics of lacosamide in extensive metabolizers (with a functional CYP2C19 cytochrome isoenzyme) and slow metabolizers (lacking a functional CYP2C19 cytochrome isoenzyme), no clinically significant difference in lacosamide excretion was observed. In addition, studies on interaction with omeprazole (an inhibitor of the CYP2C19 isoenzyme) showed no clinically significant changes in plasma concentrations of lacosamide, indicating the low significance of this pathway.
The plasma concentration of O-desmethylmetabolite is approximately 15% of that of lacosamide. This metabolite has no pharmacological activity.
Lacosamide is excreted by renal excretion and biotransformation. After oral ingestion and intravenous administration of lacosamide labeled with the radioactive isotope, approximately 95% radioactivity was noted in the urine and less than 0.5% in the feces. The T1/2 of unchanged lacosamide is approximately 13 h. Pharmacokinetic parameters are dose proportional, constant over time, and characterized by low individual variability. When lacosamide is administered 2 times daily, Css in plasma is reached within 3 days. Cumulation is accompanied by an increase in plasma concentrations of approximately 2-fold.
The Css with a single loading dose of 200 mg is comparable to that with oral administration of 100 mg twice daily.
Particular patient groups
Gender. Clinical studies show that gender has no significant effect on plasma concentrations of lacosamide.
Race. There are no clinically significant differences in the pharmacokinetics of lacosamide in Asian, Negroid and Caucasoid races.
Renal dysfunction. The AUC is increased to approximately 30% in mild to moderate renal failure and up to 60% in severe and terminal renal failure requiring hemodialysis compared to healthy patients, while the Cmax is unchanged. Lacosamide is removed from plasma by hemodialysis. During the 4 h of the hemodialysis procedure, the AUC decreases by approximately 50%. Therefore, an additional dose is recommended after the hemodialysis procedure. In patients with moderate to severe renal insufficiency, the excretion of O-desmethylmetabolite decreased several times. In patients with terminal renal failure in the absence of hemodialysis, levels were increased and continuously increased during the 24-hour follow-up. It is not fully understood whether reduced metabolite excretion in patients with terminal renal failure may result in a change in the number of side effects, but it has been confirmed that O-desmethylmetabolite has no pharmacological activity.
Hepatic impairment. In patients with moderate hepatic impairment, increased plasma concentrations of lacosamide have been observed (increased AUC by approximately 50%). One of the reasons for the increased exposure was decreased renal function in the patients who participated in the studies. Reduced nonrenal clearance in study patients was estimated as a 20% increase in the AUC of lacosamide. In patients with severe hepatic impairment, pharmacokinetics has not been studied.
Elderly patients. Four elderly patients over 75 years of age participated in the study. AUC was increased by “30% in men and 50% in women compared to younger patients. This was partially due to decreased body weight, 26% in men and 23% in women of normal body weight. In studies in elderly patients, renal clearance of lacosamide was slightly decreased.
Indications
Indications
As monotherapy or adjunctive therapy for partial seizures, with or without secondary generalization, in adults, adolescents and children 4 years of age and older with epilepsy.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antiepileptic drug, other antiepileptic drugs.
ATX code: N03AX18
Pharmacological properties
Pharmacodynamic properties
Mechanism of action
The active substance – lacosamide (R-2-acetamido-N-benzyl-3-methoxypropionamide) is a functionalized amino acid.
The exact mechanism of the antiepileptic action of lacosamide has not been established. In in vitro electrophysiological studies, lacosamide selectively enhances the slow inactivation of voltage-gated sodium channels, which leads to the stabilization of hyperexcitable neuronal membranes.
Pharmacodynamics
Lacosamide prevented the development of seizures in a large number of animal models of partial and primary generalized epilepsy, and also delayed the development of increased seizure activity. In preclinical studies, lacosamide in combination with levetiracetam, carbamazepine, phenytoin, valproate, lamotrigine, topiramate, or gabapentin demonstrated synergistic or additive anticonvulsant effects.
Clinical efficacy and safety
Adults
Monotherapy
The efficacy of lacosamide as monotherapy was demonstrated in a double-blind, parallel-group, double-blind efficacy study compared with carbamazepine (controlled release) in 886 patients 16 years of age or older with newly or previously diagnosed epilepsy. The study included patients with unprovoked partial seizures with or without secondary generalization. Patients were randomized into 2 groups in a 1:1 ratio, receiving carbamazepine and lacosamide (in tablet dosage form), respectively. Doses were selected depending on the response to therapy and ranged from 400 to 1200 mg/day for carbamazepine and 200 to 600 mg for lacosamide. Duration of therapy was up to 121 weeks, depending on response.
The expected 6-month seizure-free period was achieved in 89.8% of patients treated with lacosamide and 91.1% in the carbamazepine group (Kaplan-Meier survival analysis was used). The adjusted absolute difference between groups was 1.3% (95% confidence interval: -5.5, 2.8). The expected 12-month Kaplan-Meier seizure-free period was 77.8% for lacosamide therapy and 82.7% for carbamazepine (controlled release) therapy.
In older patients (over 65 years of age, 62 patients in the lacosamide group, 57 in the carbamazepine group), the proportion achieving a 6-month seizure-free period was similar in both groups. It was also comparable to that observed in the rest of the population. Among elderly patients, 55 (88.7%) received lacosamide as a maintenance dose of 200 mg/day, 6 (9.7%) received 400 mg/day, the dose exceeded 400 mg/day in 1 patient (1.6%).
Switching to monotherapy
The efficacy and safety of lacosamide when switching to monotherapy was studied in a multicenter, double-blind, randomized study with retrospective control. In this study, 425 patients aged 16 to 70 years with partial seizures taking stable doses of one or two antiepileptic drugs were randomized into 2 groups to switch to lacosamide monotherapy in a 3:1 ratio, receiving 400 mg or 300 mg lacosamide per day, respectively. The starting dose was 200 mg per day (100 mg twice daily). The maintenance dose was taken for at least three days before switching to monotherapy. The percentage of patients who met prespecified study exit criteria was compared with historical controls. Historical controls were provided by a pooled analysis of control groups from 8 similarly designed studies that used a subtherapeutic dose of an antiepileptic drug. Statistical superiority of lacosamide 400 mg daily was demonstrated over historical controls, indicating achievement of the primary efficacy endpoint. In addition, lacosamide 300 mg daily has been shown to be superior to historical controls. In patients who completed titration and began antiepileptic drug withdrawal (284 and 99, respectively), monotherapy was maintained in 71.5% and 70.7% of patients, respectively, for an average of 71 days. The safety profile of lacosamide when converted to monotherapy was comparable to that reported in studies of lacosamide as add-on therapy.
Complementary therapy
The effectiveness of lacosamide in adjunctive therapy at recommended doses (200 mg/day, 400 mg/day) has been proven in 3 multicenter, randomized, placebo-controlled clinical trials with a 12-week maintenance period. The effectiveness of lacosamide in adjunctive therapy at a dose of 600 mg/day has also been shown in controlled studies, although the effectiveness was comparable to a dose of 400 mg/day, but the tolerability of this dose (600 mg/day) was worse due to side effects from the central nervous system and gastrointestinal tract. Therefore, the use of a dose of 600 mg/day is not recommended. The maximum recommended dose is 400 mg/day. These studies, involving 1308 patients with a history of partial-onset seizures over an average period of 23 years, were designed to evaluate the efficacy and safety of lacosamide when given in addition to 1-3 antiepileptic drugs in patients with uncontrolled partial-onset seizures with or without secondary generalization. The overall proportion of patients with a 50% reduction in seizure frequency in the placebo, lacosamide 200 mg/day and lacosamide 400 mg/day groups was 23%, 34% and 40%, respectively.
The pharmacokinetics and safety of a single loading dose of lacosamide infusion were determined in a multicenter, open-label study of the safety and tolerability of rapid initiation of lacosamide therapy using a single intravenous loading dose (200 mg), followed by twice daily oral dosing (at a dosage equivalent to the intravenous dose) as adjunctive therapy in adult patients 16 to 60 years of age with partial-onset seizures.
Children and teenagers
Clinical manifestations of partial seizures in children over 4 years of age were comparable to those in adults. The effectiveness of lacosamide in children aged 4 years and older was calculated based on data from adolescent and adult patients with partial seizures; Thus, when selecting doses appropriate for children and adolescents (see section “Dosage and Administration”) and confirming safety (see section “Side Effects”), a similar response to lacosamide therapy was expected. The effectiveness predicted by the extrapolation method (see above) was confirmed by the results of the clinical trials.
The initial dose was 2 mg/kg/day in patients weighing up to 50 kg or 100 mg/day in patients weighing 50 kg or more; The daily dose was divided into 2 doses. During the titration period, lacosamide dosage adjustments were made in stages, increasing by 1 or 2 mg/kg/day in patients weighing up to 50 kg or by 50 or 100 mg/day in patients weighing 50 kg or more at one-week intervals to achieve the target maintenance dose.
A statistically and clinically significant reduction in the frequency of partial seizures was observed within 28 days from the start of therapy to the maintenance period when comparing data in the lacosamide and placebo groups. Overall, the proportion of patients with at least a 50% reduction in partial-onset seizure frequency between 28 days from initiation of therapy to the maintenance period was 52.9% in the lacosamide-treated group, compared with 33.3% in the placebo group.
Pharmacokinetics
Suction
Lacosamide is rapidly and completely absorbed after oral administration. The bioavailability of lacosamide in tablets is approximately 100%. After oral administration, the concentration of lacosamide in plasma increases rapidly, the maximum concentration (Cmax) is reached after 0.5-4 hours. Food intake does not affect the rate and extent of absorption.
Distribution
The volume of distribution is approximately 0.6 l/kg, the degree of binding to plasma proteins is less than 15%.
Metabolism
95% of lacosamide is excreted through the kidneys unchanged (about 40%) and in the form of O-desmethyl metabolite (less than 30%). The polar fraction (presumably serine derivatives) makes up approximately 20% in the urine and is only found in small quantities (0 – 2%) in the blood plasma. Other metabolites are determined in urine in an amount of 0.5-2%.
In vitro data indicate that the isoenzymes CYP2C9, CYP2C19 and CYP3A4 are capable of catalyzing the formation of the O-desmethyl metabolite, but the effect of the main isoenzyme has not been confirmed in vivo. When comparing the pharmacokinetics of lacosamide in extensive metabolizers (with a functional isoenzyme of the cytochrome CYP2C19) and slow metabolizers (with a deficiency of the functional isoenzyme of the cytochrome CYP2C19), no clinically significant difference in the excretion of lacosamide was noted. In addition, interaction studies with omeprazole (an inhibitor of the CYP2C19 isoenzyme) showed no clinically significant changes in lacosamide plasma concentrations, indicating the low significance of this pathway.
The concentration of O-desmethyl lacosamide in plasma is approximately 15% of the concentration of lacosamide. This metabolite has no pharmacological activity.
Removal
Lacosamide is eliminated by renal excretion and biotransformation. Following oral and intravenous administration of radiolabeled lacosamide, approximately 95% of the radioactivity was observed in urine and less than 0.5% in feces. The half-life of unchanged lacosamide is approximately 13 hours. Pharmacokinetic parameters are proportional to the dose, constant over time and characterized by low individual variability. When administered twice daily, steady-state plasma concentrations are achieved within 3 days. Cumulation is accompanied by an increase in plasma concentration by approximately 2 times.
Steady-state concentrations following a single loading dose of 200 mg are comparable to those following oral administration of 100 mg twice daily.
Pharmacokinetics in special groups of patients
Floor
Clinical studies show that gender does not have a significant effect on lacosamide plasma concentrations.
Race
There are no clinically significant differences in the pharmacokinetics of lacosamide in Asian, Negroid and Caucasian races.
Kidney failure
The area under the concentration-time curve (AUC) increases to approximately 30% in mild to moderate renal failure and up to 60% in severe and end-stage renal disease requiring hemodialysis compared with healthy patients, while Cmax does not change. Lacosamide is effectively removed from plasma by hemodialysis. Within 4 hours of a hemodialysis procedure, the area under the concentration-time curve decreases by approximately 50%. Therefore, after the hemodialysis procedure, it is recommended to take an additional dose. In patients with moderate and severe renal failure, the excretion of O-desmethyl metabolite increased several times. In patients with end-stage renal disease without hemodialysis, levels were increased and increased continuously during 24-hour follow-up. It has not been fully studied whether increased excretion of the metabolite in patients with end-stage renal failure can lead to an increase in the number of side effects, but it has been confirmed that O-desmethyl metabolite does not have pharmacological activity.
Liver failure
In patients with moderate hepatic impairment, increased lacosamide plasma concentrations were observed (approximately 50% above AUC norms). One reason for the increased exposure was decreased renal function in patients participating in the studies. The decrease in non-renal clearance in study patients was estimated as a 20% increase in lacosamide AUC. Pharmacokinetics have not been studied in patients with severe hepatic impairment.
Elderly (over 65 years old)
The studies involved 4 patients of both sexes over 75 years of age. AUC was increased by about 30% in men and 50% in women compared with younger patients. This is partly explained by reduced body weight, 26% in men and 23% in women of normal body weight. Increased lacosamide release was also observed. In studies in elderly patients, the renal clearance of lacosamide was slightly reduced.
Children and teenagers
The pharmacokinetic profile of lacosamide in children and adolescents was determined using a population pharmacokinetic analysis using individual plasma concentrations obtained in a clinical trial of 414 children with epilepsy aged 6 months to 17 years. Lacosamide was prescribed in doses ranging from 2 to 17.8 mg/kg/day twice daily. The maximum dose for children weighing 50 kg and above was 600 mg/day. Typical plasma clearances were 1.04 L/h, 1.32 L/h, and 1.86 L/h in children weighing 20 kg, 30 kg, and 50 kg, respectively. For comparison, plasma clearance in adults weighing 70 kg was 1.92 L/h.
Special instructions
Special instructions
Heart rate and conduction
Clinical studies of lacosamide have described a dose-dependent increase in the PR interval. Lacosamide should be used with caution in patients with proarrhythmic conditions, such as known cardiac conduction problems, or severe cardiac disease (eg, myocardial ischemia/infarction, heart failure, structural heart disease, or cardiac sodium channelopathies) or in patients receiving medications that affect cardiac conduction, including antiarrhythmics and antiepileptic drugs of the sodium channel blocker group, and also in elderly patients.
Such patients should have an ECG before increasing the dose of lacosamide above 400 mg/day, and also after achieving a stable concentration.
In placebo-controlled studies of lacosamide in patients with epilepsy, no atrial fibrillation or flutter was observed, but both events were identified in patients with epilepsy in open-label clinical studies, as well as in post-marketing analysis of the drug.
In post-registration practice, cases of atrioventricular block (including 2nd degree atrioventricular block) were observed. Ventricular tachyarrhythmia has been observed in patients with proarrhythmic conditions. In rare cases, these events have resulted in asystole, cardiac arrest, and death in patients with underlying proarrhythmic conditions.
Patients should be informed about the symptoms of cardiac arrhythmia (eg, slow, fast or irregular pulse, rapid heartbeat, irregular breathing, dizziness, fainting). If they occur, they should consult a doctor.
Dizziness
Treatment with lacosamide may be associated with dizziness, potentially leading to an increased risk of injury or falls. Therefore, patients should exercise caution until it is known what potential adverse reactions they may experience.
Suicidal thoughts and behavior
Suicidal ideation and behavior have been reported in patients receiving antiepileptic drugs for several indications. A meta-analysis of randomized placebo-controlled clinical trials of antiepileptic drugs suggests a small increase in the risk of suicidal ideation and suicidal behavior. The mechanism of the increased risk is not clear; existing data do not allow us to deny the existence of such a risk when taking lacosamide. Therefore, patients should be monitored for signs of suicidal ideation and behavior and appropriate treatment considered. Patients and caregivers should be advised of the risk and the need for specialist consultation if suicidal behavior occurs.
Impact on the ability to drive vehicles and machinery
The degree of influence of lacosamide on the ability to drive vehicles or operate machinery varies from minor to moderate. Treatment with lacosamide may be accompanied by dizziness or blurred vision. Patients are not recommended to drive vehicles or engage in other activities that require concentration.
Active ingredient
Active ingredient
Lacosamide
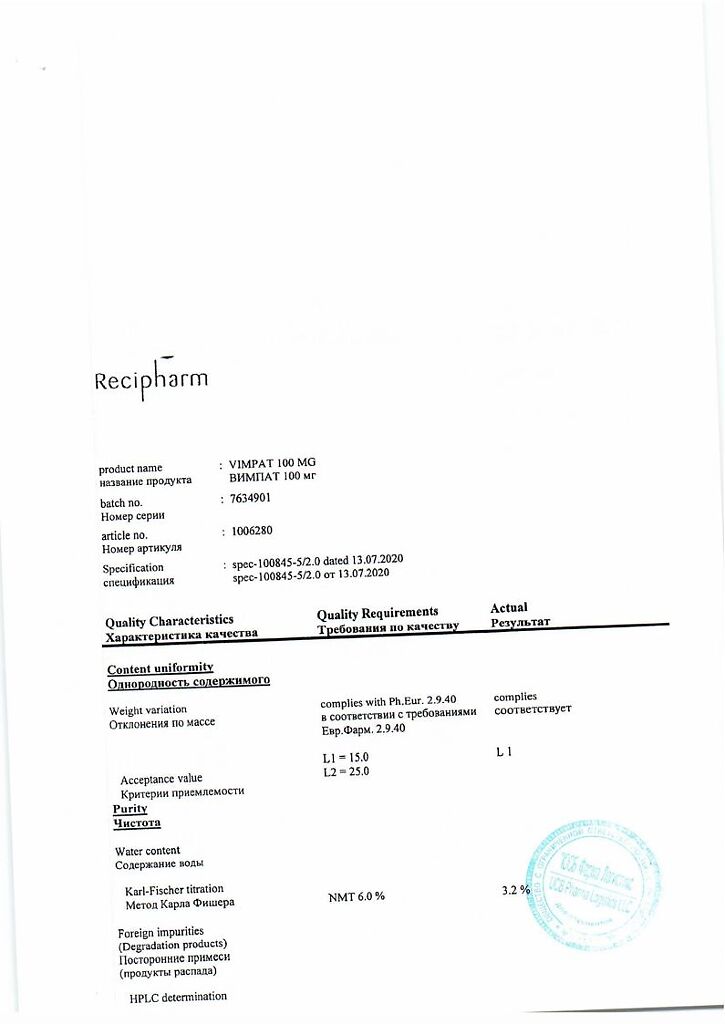
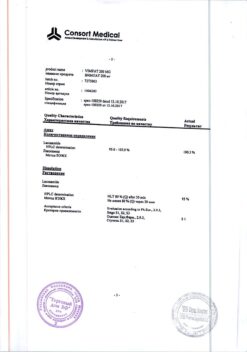
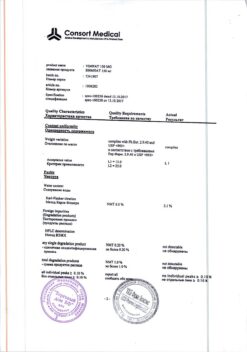
Composition
Composition
1 film-coated tablet contains:
Active ingredient: lacosamide 100 mg.
Excipients: microcrystalline cellulose (TYP102) 28.0 mg, low-substituted hyprolose 25.0 mg, silicified microcrystalline cellulose* 62.6 mg, crospovidone 20.0 mg, magnesium stearate 2.4 mg, hyprolose 2.0 mg.
Coating: opadry II (colored) 9.6 mg.
*Microcrystalline silicified cellulose consists of 98% microcrystalline cellulose and 2% colloidal anhydrous silica.
Quantitative composition of Opadry II (color):
Components
Opadry II (color)
85F38040
Yellow
Dosage
(color)
100 mg (dark yellow)
Polyvinyl alcohol
40.00%
Talc
14.80%
Macrogol 3350
20.20%
Titanium dioxide, E 171
19.17%
Iron oxide yellow dye, E172
5.83%
Pregnancy
Pregnancy
Pregnancy
General risk associated with epilepsy and antiepileptic drugs
For all antiepileptic drugs, it has been shown that the incidence of congenital malformations in children of women with epilepsy receiving such therapy is 2-3 times higher compared with the general population (in the latter case this figure is 3%). In patients receiving treatment, an increase in the incidence of congenital malformations in children was observed during polytherapy, but the extent to which treatment and/or disease contribute to this increase in risk is still unknown.
In addition, effective antiepileptic treatment should not be stopped, since the worsening of the disease has a negative impact on the mother and the fetus.
Risk associated with lacosamide use
There are no clinical data on the use of lacosamide in pregnant women. No teratogenic effects have been reported in animal studies, but embryotoxicity has been reported in rabbits and rats at maternally toxic doses. The potential risk to humans is unknown.
Lacosamide should not be used during pregnancy unless the benefit to the mother clearly outweighs the possible risk to the fetus. If a woman is planning a pregnancy, then it is necessary to carefully weigh the advisability of using this drug. To monitor the effects of using Vimpat® in pregnant women, doctors are recommended to register patient data in the European and International Register of Antiepileptic Drugs and Pregnancy (EURAP).
Lactation period
There are no data on the excretion of lacosamide into breast milk.
Excretion of lacosamide into milk has been reported in animal studies.
Breastfeeding should be discontinued during treatment with lacosamide.
Fertility
No adverse effects on fertility or reproduction were observed in rats of either sex at doses producing plasma concentrations (AUC) approximately 2 times the human plasma AUC at the maximum recommended human dose.
Contraindications
Contraindications
Hypersensitivity to the active substance or to any of the components of the drug.
Atrioventricular block II or III degree.
Age up to 4 years.
With caution
In patients with severe renal impairment (creatinine clearance ≤ 30 ml/min).
In patients with a history of conduction disturbances or severe cardiac disease, such as heart failure and a history of myocardial infarction.
Elderly patients at increased risk of heart disease.
In combination with drugs that cause a prolongation of the PR interval.
Side Effects
Side Effects
Based on an analysis of pooled placebo-controlled adjunctive therapy clinical trials that included 1308 patients with partial-onset seizures, 61.9% of patients randomized to lacosamide and 35.2% of patients randomized to placebo reported at least 1 adverse reaction. The most common adverse reactions (≥ 10%) with lacosamide were dizziness, headache, nausea and diplopia. As a rule, they were mild or moderate. The severity of some adverse reactions was dose dependent and decreased after dose reduction. The frequency and severity of central nervous system (CNS) and gastrointestinal adverse reactions generally decreased over time.
In all controlled clinical trials, the rate of discontinuation due to adverse reactions was 12.2% for patients randomized to lacosamide and 1.6% for patients randomized to placebo. The most common adverse reaction leading to discontinuation of lacosamide therapy was dizziness. The incidence of central nervous system adverse reactions, such as dizziness, may be higher after a loading dose.
Based on an analysis of data from a clinical study of lacosamide monotherapy versus carbamazepine (controlled release), the most common adverse reactions (≥ 10%) with lacosamide were headache and dizziness. The discontinuation rate due to adverse reactions was 10.6% for patients taking lacosamide and 15.6% for patients taking carbamazepine (controlled release).
The table shows adverse reactions noted during clinical trials and in post-registration practice, indicating their frequency. The frequency is distributed according to the following categories: very common (≥1/10); often (from ≥1/100 to <1/10); uncommon (≥1/1000 to <1/100), frequency unknown (cannot be determined from available data). Within each category, adverse reactions are presented in descending order of severity.
Organs, systems
Very often
Often
Uncommon
Frequency unknown
Blood and lymphatic system disorders
Agranulocytosis1
Immune system disorders
Hypersensitivity1
Hypersensitivity reactions affecting various organs and systems (including drug reaction with eosinophilia and systemic manifestations (DRESS syndrome))1
Mental disorders
Depression,
confusion, insomnia1
Aggression1, agitation1, euphoria1, mental disorders1, suicide attempts1, suicidal thoughts1, hallucinations1
Nervous system disorders
Dizziness,
headache
Balance imbalance, memory impairment, cognitive impairment, drowsiness, tremor, nystagmus, hypoesthesia, dysarthria, attention impairment, paresthesia
Fainting2,
impaired coordination of movements,
dyskinesia
Seizures3
Visual disorders
Diplopia
Blurred vision
Disorders of the hearing organ and labyrinth
Vertigo,
tinnitus
Heart disorders
Atrioventricular block1,2,
bradycardia1,2, atrial fibrillation1,2, atrial flutter1,2
Ventricular tachyarrhythmia(1)
Gastrointestinal disorders
Nausea
Vomit,
constipation, flatulence, dyspepsia, dry mouth, diarrhea
Disorders of the liver and biliary tract
Changes in liver tests2
Increased liver enzyme levels (> 2 times the upper limit of normal) 1
Skin and subcutaneous tissue disorders
Itching,
Rash1
Angioedema (Quincke’s edema)1,
hives1
Syndrome
Stevens-Johnson1, toxic epidermal necrolysis1
Muscle, skeletal and connective tissue disorders
Muscle spasm
General disorders and reactions at the injection site
Gait disturbance
asthenia, fatigue, irritability, feeling of intoxication
Injuries, intoxications and complications of procedures
Falls,
skin damage,
bruises
adverse reactions identified in post-registration practice
see section Description of selected adverse reactions
According to open prospective studies
Description of selected adverse reactions
The use of lacosamide is associated with a dose-dependent prolongation of the PR interval. Adverse reactions associated with prolongation of the PR interval (eg, atrioventricular block, syncope, bradycardia) may occur.
In clinical trials of adjunctive therapy in patients with epilepsy, the percentage of episodes of first degree atrioventricular block was low – 0.7%, 0%, 0.5% and 0% when using lacosamide at dosages of 200 mg, 400 mg, 600 mg and placebo, respectively. No atrioventricular block of degree II or higher was observed in these studies. However, in post-registration practice, cases of II and III degree atrioventricular blockade have been reported during treatment with lacosamide. In a comparative clinical study of lacosamide monotherapy versus carbamazepine (controlled release), the increase in PR interval was comparable for both drugs.
Syncope was uncommon in clinical trials of lacosamide adjunctive therapy, and the percentage of episodes that occurred did not differ between the lacosamide (n = 944) (0.1%) and placebo (0.3%) groups of epilepsy patients. In clinical studies of lacosamide monotherapy versus carbamazepine (controlled release), syncope occurred in 7 of 444 (1.6%) patients receiving lacosamide and 1 of 442 (0.2%) patients receiving carbamazepine (controlled release).
Atrial fibrillation and flutter were not observed in short-term clinical studies, but both events were noted in open-label studies in epilepsy, as well as in post-marketing practice.
Deviations in laboratory parameters
In controlled studies, changes in liver function tests were observed in placebo-controlled studies of lacosamide in adult patients with partial-onset seizures when treated with 1 to 3 antiepileptic drugs simultaneously. An increase in ALT of 3 times or more was observed in 0.7% (7 out of 935) of patients taking Vimpat® and in 0% (0 out of 356) taking placebo.
Hypersensitivity reactions affecting various organs and systems
Hypersensitivity reactions involving multiple organ systems (also known as drug reaction with eosinophilia and systemic manifestations, DRESS syndrome) have been reported in patients receiving certain antiepileptic drugs. These reactions vary in manifestation, but most often manifest as fever and rash and may affect other systems. If there is a suspicion of a hypersensitivity reaction affecting various organs and systems, then lacosamide should be discontinued.
Children and teenagers
The safety profile of lacosamide in placebo-controlled (see details of the study in the section “Pharmacodynamics. Clinical efficacy and safety”) and open-label CT (n = 408) during add-on therapy in children over 4 years of age was consistent with that in adults, although the frequency of some adverse reactions (drowsiness, vomiting and convulsions) was increased. Additional adverse reactions also appeared in children and adolescents (nasopharyngitis, fever, pharyngitis, decreased appetite, lethargy and behavioral disturbances): nasopharyngitis (15.7%), vomiting (14.7%), drowsiness (14.0%), dizziness (13.5%), fever (13.0%), convulsions (7.8%), decreased appetite (5.9%), pharyngitis (4.7%), lethargy (2.7%) and behavioral disturbances (1.7%). A total of 67.8% of patients randomized to lacosamide and 58.1% of patients randomized to placebo reported at least one adverse reaction.
Elderly patients
In a comparative study of lacosamide and carbamazepine monotherapy (controlled release), the types of adverse reactions in elderly patients (over 65 years of age) were similar to those observed in patients under 65 years of age. However, in older patients, compared with younger adults, a higher incidence (≥ 5% difference) was observed for the following adverse reactions: falls, diarrhea, and tremor. The most common adverse reaction from the cardiovascular system in elderly patients, compared with younger ones, was first degree atrioventricular block. It was observed with lacosamide in 4.8% (3 of 62) of older patients, compared with 1.6% (6 of 382) in younger adults, and for carbamazepine (controlled release) the corresponding values were 5.3% (3 of 57) in older patients and 1.3% (5 of 385) in younger adults. The incidence of adverse events observed in elderly patients during lacosamide therapy was 21.0% (13 of 62), compared with 9.2% (35 of 382) in younger adult patients. These differences between older and younger adult patients were similar to those observed in the comparator group.
Interaction
Interaction
Lacosamide should be used cautiously in combination with drugs that prolong the PR interval (including sodium channel blocker drugs) and class I antiarrhythmic drugs. However, in a subgroup analysis of clinical trials, no additional prolongation of the PR interval was observed in patients who simultaneously took lacosamide in combination with carbamazepine or lamotrigine.
In vitro data
Research results indicate a low likelihood of interaction between lacosamide and other drugs.
In vitro metabolism studies show that lacosamide does not induce CYP1A2, 2B6 and 2C9 isoenzymes. At concentrations measured in blood during clinical studies, lacosamide did not inhibit CYP1A1, 1A2, 2A6, 2B6, 2C8, 2C9, 2D6 and 2E1 isoenzymes. In vitro studies indicate that lacosamide is not transported by P-glycoprotein in the intestine. In vitro data indicate that the isoenzymes CYP2C9, CYP2C19 and CYP3A4 are capable of catalyzing the formation of the O-desmethyl metabolite.
In vivo data
Clinical data indicate that lacosamide does not inhibit or induce CYP2C19 and 3A4 isoenzymes to clinically significant levels.
Lacosamide had no effect on the area under the curve (AUC) of midazolam (metabolized via CYP3A4 at a dosage of lacosamide 200 mg twice daily), but the Cmax of midazolam was slightly increased (30%). Lacosamide does not affect the pharmacokinetics of omeprazole (metabolized through isoenzymes CYP2C19 and 3A4, at a dosage of lacosamide 300 mg twice daily).
Omeprazole, an inhibitor of the CYP2C19 isoenzyme (40 mg 4 times a day), did not increase clinically significant exposure to lacosamide. Thus, it is unlikely that moderate inhibitors of the CYP2C19 isoenzyme can affect the systemic exposure of lacosamide to a clinically significant level.
Caution should be exercised during simultaneous use with strong inhibitors of the CYP2C19 isoenzyme (for example, fluconazole) and the CYP3A4 isoenzyme (for example, itraconazole, ketoconazole, ritonavir, clarithromycin), which may lead to an increase in the systemic exposure of lacosamide. These interactions have not been established in vivo, but are possible based on in vitro data.
Potent inducers of liver microsomal enzymes, such as rifampicin or St. John’s wort (Hypericum perforatum), may cause a moderate decrease in systemic concentrations of lacosamide. In this regard, caution should be exercised when prescribing or discontinuing such drugs.
Antiepileptic drugs
In interaction studies, lacosamide did not have a significant effect on plasma concentrations of carbamazepine and valproic acid. Carbamazepine and valproic acid had no effect on lacosamide plasma concentrations.
Based on a population pharmacokinetic analysis, it was concluded that concomitant therapy with antiepileptic drugs that induce liver microsomal enzymes (carbamazepine, phenytoin, phenobarbital in various doses) reduced the total systemic exposure of lacosamide by 25% in adult patients and by 17% in children and adolescents.
Oral contraceptives
There were no signs of significant interaction between lacosamide and oral contraceptives: ethinyl estradiol and levonorgestrel. Lacosamide has no effect on progesterone concentrations.
Other interactions
Lacosamide does not affect the pharmacokinetics of digoxin. No clinically significant interaction between lacosamide and metformin has been identified.
There is no data on the interaction of lacosamide with alcohol.
The degree of binding of lacosamide to plasma proteins is less than 15%. In this regard, clinically significant interaction with other drugs that bind to plasma proteins is unlikely.
When used concomitantly with warfarin, lacosamide does not have a clinically significant effect on the pharmacodynamics and pharmacokinetics of warfarin.
Overdose
Overdose
Symptoms
Symptoms occurring after accidental or intentional overdose of lacosamide were predominantly due to damage to the central nervous system and gastrointestinal tract.
The types of adverse reactions in patients taking doses from 400 mg to 800 mg and taking recommended doses of lacosamide were not clinically different.
Reactions noted after taking more than 800 mg included dizziness, nausea, vomiting, epileptic seizures (generalized tonic-clonic seizures, status epilepticus). Cardiac conduction abnormalities, shock, and coma have also been reported. Fatalities have been reported in patients following an acute overdose of several grams of lacosamide.
Treatment
There is no antidote for lacosamide. Treatment of overdose is symptomatic. If necessary, hemodialysis can be used.
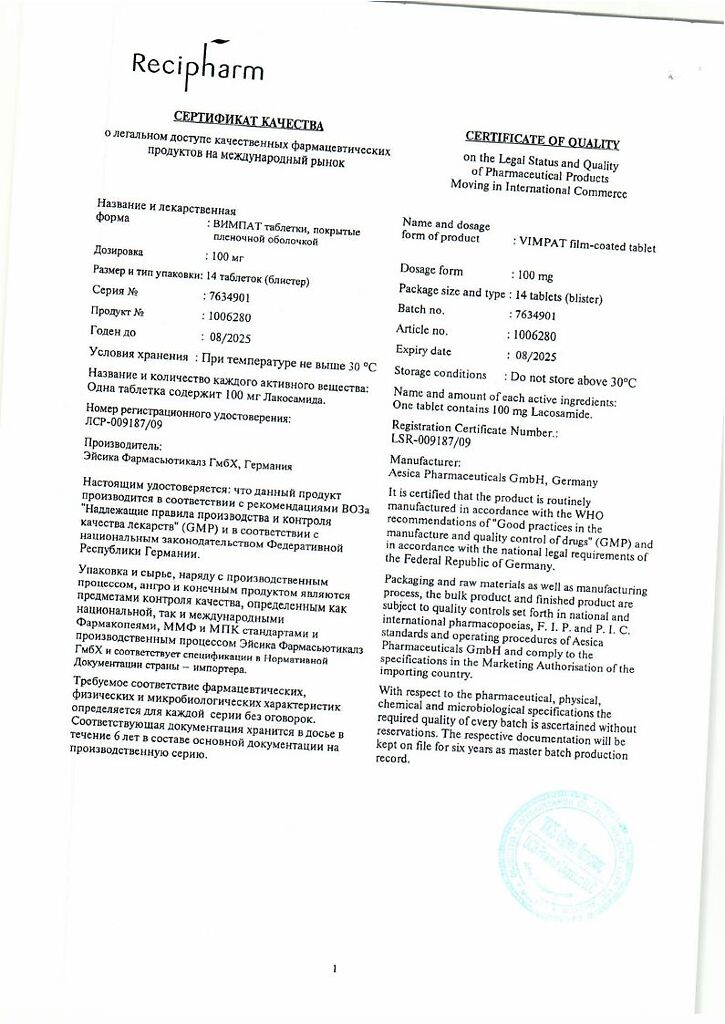
Storage conditions
Storage conditions
Store at a temperature not exceeding 30 C.
Keep out of the reach of children.
Shelf life
Shelf life
5 years.
Do not use the drug after the expiration date.
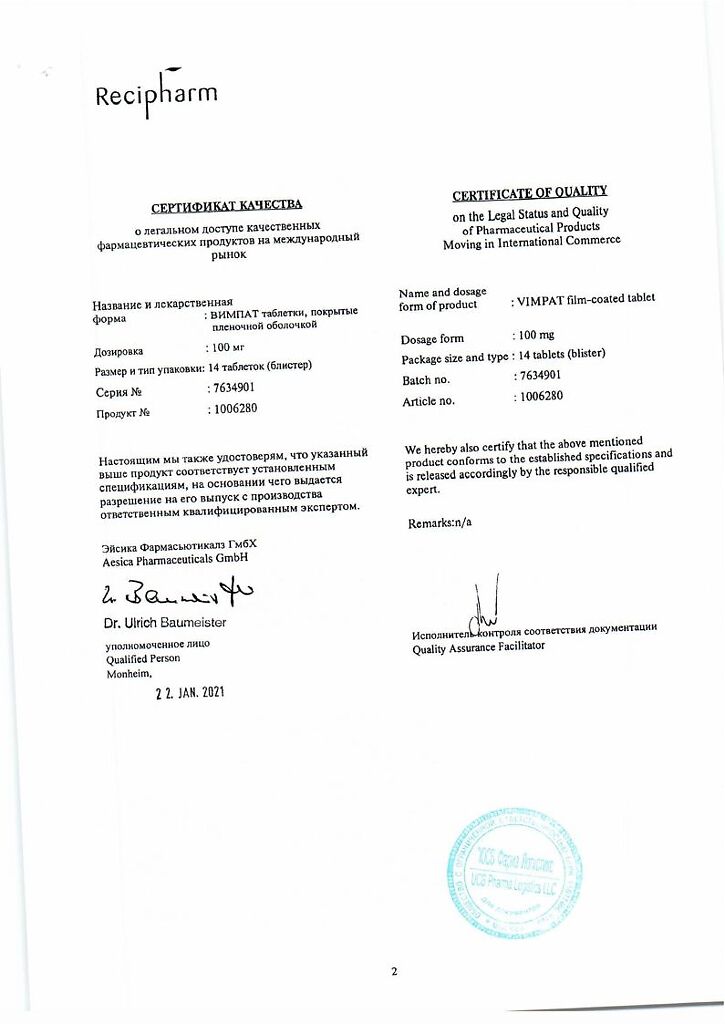
Manufacturer
Manufacturer
Eisika Pharmaceuticals GmbH, Germany
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Eisika Pharmaceuticals GmbH, Germany |
| Medication form | pills |
| Brand | Eisika Pharmaceuticals GmbH |
Other forms…
Related products
Buy Vimpat, 100 mg 14 pcs with delivery to USA, UK, Europe and over 120 other countries.