No products in the cart.
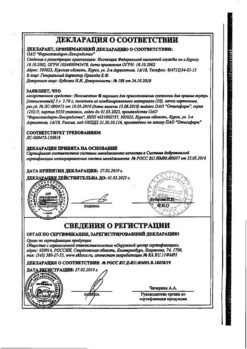
Venlafaxine-ALSI, tablets 75 mg 30 pcs
€16.11 €13.43
Out of stock
(E-mail when Stock is available)
Description
Venlafaxine is an antidepressant chemically unrelated to any class of antidepressants (tricyclic, tetracyclic, or other) and is a racemate of two active enantiomers. Venlafaxine and its main metabolite, O-desmethylvenlafaxine (ODV), are potent serotonin and noradrenaline reuptake inhibitors (abbreviated: SSRIs or SSRIs) and weak dopamine reuptake inhibitors.
Indications
Indications
Depression. Prevention and treatment.
Pharmacological effect
Pharmacological effect
Venlafaxine is an antidepressant that does not chemically belong to any class of antidepressants (tricyclic, tetracyclic or others) and is a racemate of two active enantiomers. Venlafaxine and its main metabolite, O-desmethylvenlafaxine (ODV), are potent serotonin and norepinephrine reuptake inhibitors (abbreviated as SNRIs or SNRIs) and weak dopamine reuptake inhibitors.
Special instructions
Special instructions
Suicide and suicidal behavior
Depression is associated with an increased risk of suicidal ideation, self-harm, and suicide (suicidal behavior). This risk persists until significant remission occurs. Since improvement may not be observed during the first few weeks of therapy or even longer, patients should be closely monitored until such improvement occurs. Based on accumulated clinical experience, the risk of suicide may increase in the early stages of recovery.
Patients with a history of suicide attempts or high levels of suicidal ideation prior to treatment are at greater risk for suicidal ideation or suicide attempts and should be closely monitored. A meta-analysis of placebo-controlled clinical trials of antidepressants in adult patients with mental disorders found that antidepressants were at increased risk of suicidal behavior compared with placebo in patients under 25 years of age. Drug treatment of these patients, and in particular those at high risk of suicide, should be accompanied by careful monitoring, especially early in therapy and during dose adjustment. Patients (and caregivers of such patients) should be warned to monitor for any signs of clinical worsening, suicidal behavior or ideation, or unusual changes in behavior, and to seek immediate medical attention if these symptoms occur.
In a small number of patients taking antidepressants, including venlafaxine, aggression may occur during treatment initiation, dose changes, or discontinuation.
Clinical studies conducted to date have not revealed tolerance or dependence to venlafaxine. Despite this, as with other drugs that act on the central nervous system, the physician should closely monitor patients for signs of drug abuse, as well as patients with a history of such symptoms.
Special patient groups
Venlafaxine is not approved for use in children.
In patients with a history of aggression, venlafaxine should be used with caution. In patients with affective disorders and bipolar disorder, hypomanic and manic states may occur when treated with antidepressants, including venlafaxine. Like other antidepressants, venlafaxine should be used with caution in patients with a history of mania. Such patients require medical supervision.
Convulsive disorders may occur during therapy with venlafaxine. As with all antidepressants, venlafaxine should be used with caution in patients with a history of seizure disorders and such patients should be closely monitored. Treatment should be discontinued if seizures develop.
Akathisia
The use of venlafaxine has been associated with the development of akathisia, which is characterized by an unpleasant feeling of internal motor restlessness for the patient and manifested in the patient’s inability to sit quietly in one position for a long time or remain motionless for a long time. This condition may occur at the beginning of treatment and during the first weeks of treatment. In patients who develop such symptoms, increasing the dose is not recommended.
Bipolar disorder
Before starting treatment, it is necessary to identify those patients who are at risk for bipolar disorder. Such a check should include a detailed study of the medical history, including family history, to identify cases of suicide and bipolar disorder. It should be noted that venlafaxine is not recommended for use in the treatment of bipolar depression.
Use in patients with concomitant diseases
Clinical experience with the use of venlafaxine in patients with concomitant diseases is limited.
It should be used with caution in patients with diseases in which the effect of venlafaxine on hemodynamic parameters and/or metabolism may be significant.
Patients should be warned to immediately consult a doctor if a rash, urticaria or other allergic reactions occur.
Some patients while taking venlafaxine experienced a dose-dependent increase in blood pressure and/or an increase in heart rate, therefore regular monitoring of blood pressure and ECG is recommended, especially during the period of adjusting or increasing the dosage of venlafaxine. In post-marketing experience with venlafaxine (overdose), fatal cardiac arrhythmias have been reported. Before prescribing venlafaxine to patients at high risk of developing serious cardiac arrhythmias, the ratio of the likely benefit to the possible risk of use should be assessed.
Patients, especially the elderly, should be warned about the possibility of dizziness and impaired balance in order to prevent injury.
While taking venlafaxine, especially in conditions of dehydration or decreased circulating blood volume (including in elderly patients and patients taking diuretics), hyponatremia and/or syndrome of insufficient secretion of antidiuretic hormone may occur.
Venlafaxine has not been studied in patients with recent myocardial infarction and decompensated heart failure. The drug should be prescribed to such patients with caution.
Taking SSRIs or venlafaxine in patients with diabetes may cause changes in plasma glucose levels. Dosage adjustments of insulin and/or antidiabetic medications may be required.
During treatment, it is recommended to refrain from drinking any alcohol-containing drinks.
The safety and effectiveness of venlafaxine in combination with weight loss medications (including phentermine) have not been established. The simultaneous use of venlafaxine and drugs that reduce body weight is not recommended.
Women of childbearing potential should use appropriate methods of contraception while taking venlafaxine.
Explanations of special symptoms and conditions that may occur during treatment with the drug
Dry mouth occurs in 10% of patients receiving venlafaxine. This may increase your risk of developing tooth decay. Patients should practice good oral hygiene.
The use of venlafaxine may cause the development of akathisia, characterized by subjective discomfort or restlessness and the need to move frequently, often accompanied by an inability to sit or stand still. This mostly occurs during the first few weeks of treatment. Increasing the dose in patients who develop these symptoms may cause undesirable effects.
In placebo-controlled clinical trials, 5.3% of patients experienced a clinically significant increase in serum cholesterol. Cholesterol level control is necessary during long-term treatment.
Withdrawal syndrome
When stopping treatment, withdrawal symptoms are common, especially if it is stopped abruptly. The risk of withdrawal syndrome may depend on several factors, including the duration of treatment, the size of therapeutic doses and the rate of dose reduction. These symptoms are very rarely reported in patients who accidentally missed taking the drug.
Withdrawal symptoms usually occur within the first few days after stopping treatment. These symptoms usually go away within 2 weeks, although in some people they may last 2-3 months or more. It is recommended to gradually reduce the dose of venlafaxine when stopping the drug – over several weeks or months, depending on the severity of the clinical symptoms of the disease.
Serotonin syndrome
Taking venlafaxine, like other serotonergic drugs, can cause serotonin syndrome, a potentially life-threatening condition, especially when used concomitantly with other drugs that can affect the serotonergic neurotransmitter systems, such as MAO inhibitors (see section “Interactions with other drugs”).
Symptoms of serotonin syndrome may include mental status changes (agitation, hallucinations, coma), autonomic instability (tachycardia, blood pressure lability, hyperthermia), neuromuscular disorders (hyperreflexia, incoordination), and/or gastrointestinal symptoms (nausea, vomiting, diarrhea).
Information about the possible effect of the drug on the ability to drive vehicles and machinery
During the treatment period, care should be taken when performing potentially hazardous types of work that require increased concentration and speed of psychomotor reaction (including driving a car and operating machinery).
Active ingredient
Active ingredient
Venlafaxine
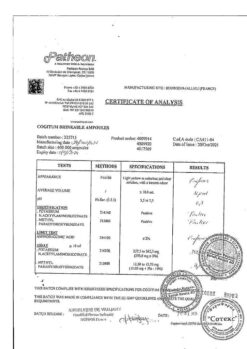
Composition
Composition
One tablet contains:
active substance:
venlafaxine hydrochloride – 84.84 mg, which corresponds to 75 mg of venlafaxine;
excipients:
microcrystalline cellulose – 134.62 mg,
pregelatinized starch – 99.00 mg,
colloidal silicon dioxide (aerosil) – 1.64 mg,
talc – 6.60 mg,
magnesium stearate – 3.30 mg
Contraindications
Contraindications
Hypersensitivity to venlafaxine or to any of the excipients, simultaneous use with MAO inhibitors (see also section “Interaction with other drugs”), severe renal and/or liver dysfunction (glomerular filtration rate (GFR) less than 10 ml/min).
Taking the drug is contraindicated in people under 18 years of age, during pregnancy and lactation.
With caution:
Recent myocardial infarction, unstable angina, arterial hypertension, arrhythmias (especially tachycardia), history of convulsive syndrome, increased intraocular pressure, closed-angle glaucoma, history of manic states, suicidal tendencies, predisposition to bleeding from the skin and mucous membranes, initially reduced body weight, hyponatremia, dehydration, simultaneously with diuretics or with drugs used to treat obesity (see also section “Special instructions”).
Pregnancy and lactation
Venlafaxine should not be prescribed to pregnant and breastfeeding women, because The safety of the drug during pregnancy and lactation in women has not been sufficiently established, due to the fact that there are no adequately controlled clinical studies on a sufficiently large sample of such patients. This concerns the health of both the mother and, to a greater extent, the fetus/child. Women of childbearing age should be warned about this before starting treatment and should immediately consult a doctor if they become pregnant or plan to become pregnant during treatment with the drug. Venlafaxine and its metabolite (EFV) are excreted into breast milk. If it is necessary to take the drug during lactation, breastfeeding must be stopped.
In practice, there are cases of prescribing venlafaxine to mothers during pregnancy and shortly before childbirth, when in a particular situation the expected benefit to the mother outweighs the potential risk to the fetus. In these cases, newborns often experienced complications that required: increased hospitalization, maintenance of breathing and tube feeding. These complications can develop immediately after childbirth and are also typical when taking other antidepressants from the SNRI group or SSRIs (not containing venlafaxine). In such cases, the following clinical symptoms have been reported in newborns: respiratory disorders, cyanosis, apnea, convulsions, temperature instability, feeding difficulties, vomiting, hypoglycemia, muscle hypertension or hypotonia, hyperreflexia, tremor, trembling, irritability, lethargy, constant crying, drowsiness or insomnia. Such disturbances may indicate the serotonergic effects of the drug Venlafaxine. If venlafaxine was used during pregnancy and maternal treatment was completed shortly before delivery, the newborn may experience withdrawal symptoms. In such a newborn, the presence of serotonin syndrome or neuroleptic malignant syndrome should be excluded. Epidemiological evidence suggests that use of SSRIs during pregnancy, especially late in pregnancy, may increase the risk of persistent neonatal pulmonary hypertension.
Side Effects
Side Effects
Frequency of side effects: very common (≥ 1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1000 to < 1/100), rare (≥ 1/10,000 to < 1/1000), very rare (< 1/10,000), frequency not established (currently there are no data on the prevalence of adverse reactions).
General symptoms: often – weakness, increased fatigue, chills; infrequently – Quincke’s edema, photosensitivity reactions; frequency not established – anaphylactic reactions.
From the nervous system: very often – dry mouth, headache; often – unusual dreams, decreased libido, dizziness, insomnia, increased excitability, paresthesia, stupor, confusion, depersonalization, increased muscle tone, tremor; infrequently – apathy, agitation, hallucinations, myoclonus, impaired coordination of movements and balance; rarely – akathisia, psychomotor agitation, epileptic seizures, manic reactions; frequency not established – dizziness, neuroleptic malignant syndrome (NMS), serotonin syndrome, delirium, extrapyramidal reactions (including dystonia and dyskinesia), tardive dyskinesia, suicidal thoughts and behavior, aggression.
From the gastrointestinal tract: very often – nausea; often – loss of appetite (anorexia), constipation, vomiting; infrequently – bruxism, diarrhea; rarely – hepatitis; frequency not established – pancreatitis.
From the respiratory system: often – yawning, bronchitis, shortness of breath; rarely: interstitial lung diseases (ILD) and eosinophilic pneumonia, chest pain.
From the cardiovascular system: often – arterial hypertension, hyperemia of the skin; uncommon – postural hypotension, tachycardia, fainting; frequency not established – hypotension, QT interval prolongation, ventricular fibrillation, ventricular tachycardia (including bidirectional tachycardia).
From the hematopoietic system: infrequently – hemorrhages into the skin (ecchymosis), gastrointestinal bleeding; frequency not established – hemorrhages in the mucous membranes, prolongation of bleeding time, thrombocytopenia, pathological changes in the blood (including agranulocytosis, aplastic anemia, neutropenia and pancytopenia).
From the side of metabolism: often – increased cholesterol levels in the blood serum, decreased body weight; infrequently – weight gain; very rarely – an increase in prolactin levels; frequency not established – changes in laboratory tests of liver function, hepatitis, hyponatremia, syndrome of insufficient secretion of antidiuretic hormone.
From the genitourinary system: often – ejaculation/orgasm disorders (in men), erectile dysfunction (impotence), anorgasmia, dysuric disorders (mainly difficulties at the beginning of urination), pollakiuria, menstrual disorders associated with increased bleeding or increased irregular bleeding (menorrhagia, metrorrhagia); infrequently – orgasm disorders (in women), urinary retention; rarely – urinary incontinence.
From the senses: often – disturbances of accommodation, mydriasis, blurred vision; infrequently – disturbance of taste, noise or ringing in the ears; frequency not established – angle-closure glaucoma.
From the skin: very often – sweating; infrequently – alopecia, a rapidly passing rash; frequency not established – erythema multiforme, toxic epidermal necrolysis, Stevens-Johnson syndrome, itching, urticaria.
From the musculoskeletal system: frequency not established – rhabdomyolysis.
When you stop taking venlafaxine, abruptly stop or reduce the dose, symptoms may be observed that relate to the so-called withdrawal syndrome: increased fatigue, asthenia, headache, dizziness, sleep disturbances (drowsiness or insomnia, difficulty falling asleep, unusual dreams), hypomania, anxiety, agitation (increased nervous excitability and irritability), confusion, paresthesia (spontaneously occurring unpleasant sensation of numbness, tingling, burning, crawling, etc.), increased sweating, dry mouth, decreased appetite, nausea, vomiting, diarrhea (most of these reactions are mild and do not require treatment).
Interaction
Interaction
Venlafaxine, which itself does not have increased binding to plasma proteins, practically does not increase the concentration of concomitantly taken drugs, which are characterized by high binding to plasma proteins. No clinically significant interaction with antihypertensive (many pharmacological groups, including beta blockers, angiotensin-converting enzyme inhibitors and diuretics) and antidiabetic drugs was detected. Caution should be exercised when co-administered with other drugs that affect the central nervous system (CNS), since combinations of venlafaxine with all such drugs have not been studied.
Monoamine oxidase inhibitors (MAO)
The simultaneous use of venlafaxine with MAO inhibitors, as well as within 14 days after their discontinuation, is contraindicated (the risk of severe side effects, including death, is likely). Therapy with MAO inhibitors can be prescribed no less than 7 days after discontinuation of the drug Venlafaxine. Venflaxin should be discontinued at least 7 days before starting reversible selective MAO inhibitors (moclobemide). The weakly reversible and non-selective inhibitor MAOlinezolid (an antimicrobial drug) and methylene blue (intravenous dosage form) are also not recommended for simultaneous use with venlafaxine.
Serotonergic agents
Caution should be exercised in the simultaneous use of drugs that affect the serotonin system of mediators, such as triptans (sumatriptan, zolmitriptan, etc.), selective serotonin reuptake inhibitors (SSRIs) and SNRIs (prolonged seizures have been reported), tricyclic antidepressants, lithium, sibutramine or fentanyl (and its analogues dextromethorphan, tramadol and etc.), as well as excess sources of tryptophan due to the increased potential risk of serotonin syndrome.
Alcohol
During treatment with venlafaxine, alcohol should be completely avoided. Alcohol increases the psychomotor dysfunction that venlafaxine can cause.
Lithium
Lithium preparations do not have a significant effect on the pharmacokinetics of venlafaxine.
Diazepam
There was no effect of orally administered diazepam on the pharmacokinetics of venlafaxine and EDV, and, conversely, venlafaxine did not change the pharmacokinetics of diazepam and its metabolite desmethyldiazepam. In addition, the administration of both of these drugs does not impair the psychomotor and psychometric effects caused by diazepam.
Cimetidine
The simultaneous administration of cimetidine and venlafaxine resulted in a delay in metabolism during the “first pass” of venlafaxine. Oral clearance of venlafaxine decreased by 43%, and the area under the pharmacokinetic curve (AUC) and maximum concentration (Cmax) of this drug increased by 60%. However, no similar impact was found for EFA. Since the total activity of venlafaxine and EFA is expected to increase only slightly, no dose adjustment will be required for most normal patients. However, in patients with existing (detected) hypertension, elderly patients and those with impaired liver or kidney function, the dose of venlafaxine may be adjusted.
Haloperidol
In a study where venlafaxine was administered at steady state at a dose of 150 mg/day, a 42% decrease in total oral haloperidol clearance was observed after a 2 mg oral dose; while the area under the pharmacokinetic curve (AUC) increased by 70%, and Cmax increased by 88%, while the half-life of haloperidol (T 1/2) did not change. This should be taken into account when choosing the correct dose of haloperidol.
Imipramine
Venlafaxine does not impair the pharmacokinetics of imipramine and 2-hydroxyimipramine. However, the AUC, Cmax and Cmin of desipramine (the active metabolite of imipramine) increased by approximately 35% when co-administered with venlafaxine. The concentration of 2-hydroxydesipramine also increases from 2.5 to 4.5 times (depending on the dose of venlafaxine: 37.5 mg for 12 hours or 75 mg for 12 hours), but the clinical significance of this fact is not known.
Metoprolol
When using metoprolol and venlafaxine simultaneously, caution should be exercised, since due to pharmacokinetic interaction, the concentration of metoprolol in the blood plasma increases by approximately 30-40%, without changing the concentration of its active metabolite α-hydroxymetoprolol. The clinical significance of this interaction has not been studied. Metoprolol does not affect the AUC of venlafaxine and EDV.
Risperidone
When used concomitantly with risperidone (despite an increase in the AUC of risperidone), the pharmacokinetics of a pair of active molecules (risperidone and 9-hydroxyrisperidone) do not change significantly when combined with venlafaxine.
Clozapine
During post-marketing studies of venlafaxine, it was found that when used simultaneously with clozapine, its concentration in the blood plasma increases. This was manifested by an increase in the side effects of clozapine, especially in relation to the incidence of seizures.
Indinavir
With simultaneous use, the pharmacokinetics of indinavir changes (AUC decreases by 28% and Cmax decreases by 36%). For venlafaxine, no changes in pharmacokinetics are observed. The clinical significance of this fact is unknown.
Ketoconazole
A pharmacokinetic study when combined with ketoconazole showed an increase in plasma concentrations of venlafaxine and EDV in subjects whose initial metabolism by the CYP2D6 isoenzyme is either good (X-Met) or poor (P-Met). In particular, the Cmax of venlafaxine increased by 26% for X-Met and by 48% for P-Met. EFA Cmax values increased by 14% and 29% in X-Met and P-Met subjects, respectively. The AUC of venlafaxine increased by 21% for X-Met and 70% for P-Met. EFA AUC values increased by 23% and 33% in X-Met and P-Met subjects, respectively.
Drugs that affect blood clotting and platelet function (NSAIDs, acetylsalicylic acid preparations and other anticoagulants)
Serotonin, released by platelets, plays an important role in hemostasis (stopping bleeding). Epidemiological studies demonstrate an association between the use of psychotropic drugs that interfere with serotonin reuptake and the incidence of upper gastrointestinal bleeding. This relationship is enhanced if non-steroidal anti-inflammatory drugs (NSAIDs), drugs containing acetylsalicylic acid or other anticoagulants are used simultaneously. The risk of bleeding has been shown to increase when SSRIs and SNRIs (including venlafaxine) are prescribed concomitantly with warfarin. Patients prescribed warfarin should be closely monitored for prothrombin time and/or partial thromboplastin time, especially when co-administration with venlafaxine is started or stopped.
Interaction with other drugs at the level of studied metabolism with cytochrome P450 isoenzymes
The main routes of metabolism of venlafaxine include the isoenzymes CYP2D6 and CYP3A4: the first of them converts venlafaxine into its active metabolite EDV, and the second is less important in the metabolism of venlafaxine compared to CYP2D6 and forms the product N-desmethylvenlafaxine with little pharmacological activity. Preclinical studies have shown, and subsequently confirmed clinically, that venlafaxine is a relatively weak inhibitor of CYP2D6. Therefore, even when prescribed with drugs that moderately suppress the activity of this enzyme (see the example with imipramine above), or in the case of patients with a genetically determined decrease in CYP2D6 function, no dose adjustment of venlafaxine is required, since the total concentration of the active substance and active metabolite (venlafaxine and EDV) does not change significantly. This characterizes venlafaxine positively when compared with other antidepressants. Caution should be exercised when co-administered with CYP2D6 inhibitors such as quinidine, paroxetine, fluoxetine, haloperidol, perphenazine, levomepromazine, as venlafaxine may potentially increase the plasma concentrations of these CYP2D6 substrates. In combination with drugs that inhibit both enzymes (CYP2D6 and CYP3A4), special caution is required. Such drug interactions have not yet been sufficiently studied, and in this case this combination of drugs is not recommended.
In addition, venlafaxine does not suppress the activity of the enzymes CYP3A4, CYP1A2 and CYP2C9, therefore, no significant interaction is observed with drugs such as alprozolam, caffeine, carbamazepine, diazepam, tolbutamide, terfenadine.
Interaction with ketoconazole is described above. CYP3A3/4 inhibitors such as itraconazole and ritonavir can have a similar effect.
Other interactions with various concomitant therapeutic factors and food
When using venlafaxine, special caution should be exercised during electroconvulsive therapy, as there is no experience with the use of venlafaxine in these conditions.
There was no significant effect of different types of food on the absorption of venlafaxine and its subsequent conversion to EDV. Foods (usually high in protein, such as hard cheeses, fish roe, turkey), as well as dietary supplements and fitness diets that are high sources of tryptophan, potentially increase the body’s production of serotonin, which may increase the serotonergic side effects of venlafaxine.
Undesirable pharmacodynamic interactions may occur when Venlafaxine is taken simultaneously with the medicinal plant St. John’s wort (herb or various preparations made from it); such a combination is not recommended.
There are reports of false-positive results of the immunochromatographic rapid urine test (test strip) for phencyclidine and amphetamines in patients taking venlafaxine, even several days after discontinuation of venlafaxine. This may be explained by the lack of specificity of this test. Only a confirmatory test in a specialized anti-doping laboratory can distinguish venlafaxine from phencyclidine and amphetamines.
According to the data available to date, venlafaxine has not shown itself to be a drug that causes drug abuse or addiction (both in preclinical receptor affinity studies and in clinical practice).
Overdose
Overdose
Symptoms of overdose: impaired consciousness (from drowsiness to coma), agitation, possible vomiting, diarrhea; tremor, decreased or (mild) increased blood pressure, dizziness, mydriasis, convulsive states, sinus or ventricular tachycardia or bradycardia; changes on the ECG (prolongation of the Q-T interval, bundle branch block, widening of the QRS complex).
Post-marketing experience indicates that the most common overdose of venlafaxine occurred with concomitant use of alcohol and/or other psychotropic drugs. There are repeated reports of deaths.
Published literature on retrospective studies of venlafaxine overdoses report that this increased risk of fatal outcomes may be inherent in venlafaxine when compared with commercially available SSRI antidepressants, but this risk is lower than the risk inherent in tricyclic antidepressants. Epidemiological studies have shown that those patients treated with venlafaxine have a greater risk of suicide compared with those patients treated with SSRIs (other than venlafaxine). However, it remains unclear to what extent these high rates of death (due to venlafaxine overdose) are due to the toxic properties of the drug itself or the special characteristics of the group of patients treated with venlafaxine. According to clinical experience, it is recommended that prescriptions for venlafaxine prescribe the minimum possible amount of the drug, sufficient only until the patient’s next visit, in order to reduce the risk of intentional overdose (see also section “Special Instructions”).
Treatment: symptomatic and supportive therapy is provided. Specific antidotes are unknown. Continuous monitoring of vital functions (respiration, circulation and heart rate) is recommended. In case of overdose, it is recommended to immediately lavage the stomach and take activated charcoal to reduce the absorption of the drug. Inducing vomiting is not recommended if there is a risk of aspiration of vomit. Forced diuresis, dialysis, and blood transfusion are ineffective.
Recommendations for use
Recommendations for use
Inside.
Venlafaxine is taken with food, preferably at the same time, without chewing and with liquid. The recommended starting dose is 75 mg in two divided doses daily (37.5 mg 2 times a day). Depending on tolerability and effectiveness, the dose may be gradually increased to 150 mg/day. If necessary, the dose is increased to 225 mg/day. Dose increases of 75 mg/day can be made at intervals of 2 weeks or more, if clinically necessary, due to the severity of symptoms, it is possible to increase the dose in a shorter period of time, but not less than 4 days. Higher doses (up to a maximum daily dose of 375 mg/day in 2-3 doses) require inpatient monitoring of patients. After achieving the required therapeutic effect, the daily dose can be gradually reduced to the minimum effective level.
Maintenance therapy and relapse prevention: Maintenance treatment can last 6 months or more. The minimum effective doses used in the treatment of a depressive episode are prescribed.
Renal failure: in case of mild renal failure (glomerular filtration rate (GFR) more than 30 ml/min), no dosage adjustment is required. In case of moderate renal failure (GFR 10-30 ml/min), the dose should be reduced by 25-50%. Due to the prolonged half-life of venlafaxine and its active metabolite (EAM), these patients should take the entire dose once daily. It is not recommended to use venlafaxine in severe renal failure (GFR less than 10 ml/min), since reliable data on such therapy are lacking. During hemodialysis, the daily dose should be reduced by 50%; the drug should be taken after the end of the hemodialysis session.
Liver failure: in case of mild liver failure (prothrombin time (PT) less than 14 seconds), no dosage adjustment is required. In case of moderate liver failure (PT from 14 to 18 seconds), the daily dose should be reduced by 50% or more. It is not recommended to use venlafaxine in severe liver failure, since there are no reliable data on such therapy.
Elderly patients: the elderly age of the patient in the absence of any acute or chronic diseases does not require dose changes, however (as when prescribing other drugs) caution is required when treating elderly patients. Elderly patients should use the lowest effective dose. When increasing the dose, the patient should be under close medical supervision.
Withdrawal of the drug
Discontinuation of the drug should be done gradually to minimize the risk associated with drug withdrawal. With a course of treatment of 6 weeks or more, the period of gradual withdrawal of the drug should be at least 2 weeks and depends on the dose, duration of therapy and the individual characteristics of the patient.
Functional features
Functional features
Absorption:
Absorption from the gastrointestinal tract is good, about 92% for a single dose, and is not quantitatively dependent on food intake.
Distribution:
Overall bioavailability is 40-45%, which is associated with intense first-pass metabolism in the liver. Venlafaxine and EDV bind to human plasma proteins by 27 and 30%, respectively; they both pass into breast milk. In the range of daily doses of venlafaxine 75-450 mg, venlafaxine itself and EDV have linear kinetics. The time to reach the maximum plasma concentration (TCmax) of venlafaxine and EDV is 2 and 3 hours, respectively, after taking Venlafaxine tablets orally. When taking long-acting forms of venlafaxine, TCmax is 5.5 and 9 hours, respectively.
The half-life (T1/2) was 5 ± 2 hours and 11 ± 2 hours for venlafaxine and EDV, respectively. Equilibrium plasma concentrations (Css) for venlafaxine and EDV are achieved after 3 days of multiple doses of therapeutic doses.
Metabolism:
Metabolized mainly in the liver with the participation of the CYP2D6 isoenzyme to the only pharmacologically active metabolite (EFA), as well as to the inactive metabolite N-desmethylvenlafaxine. Venlafaxine is a weak inhibitor of the CYP2D6 isoenzyme and does not inhibit CYP1A2, CYP2C9 or CYP3A4.
Removal:
Excreted primarily by the kidneys: approximately 87% of a single dose taken is excreted in the urine within 48 hours (5% unchanged, 29% as unconjugated EDV, 26% as conjugated EDV, 27% as other inactive metabolites), and after 72 hours 92% of the drug is excreted by the kidneys.
The mean ± standard deviation for plasma clearance of venlafaxine and EDV is 1.3 ± 0.6 and 0.4 ± 0.2 L/h/kg, respectively; apparent half-life 5 ± 2 and 11 ± 2 hours, respectively; apparent (at steady state) volume of distribution 7.5 ± 3.7 and 5.7 ± 1.8 l/kg, respectively.
Special groups
The gender and age of the patient do not have a significant effect on the pharmacokinetic parameters of venlafaxine and EFA.
For elderly patients, no special dose adjustment is required depending on age.
In patients with low activity of the CYP2D6 isoenzyme, there is no need to select individual doses. Despite the multidirectional changes in concentrations taken separately, namely venlafaxine (increases) and EDV (decreases), the sum of the areas under the pharmacokinetic curves of these two active substances does not actually change due to a decrease in the activity of the CYP2D6 isoenzyme, and accordingly no dose adjustment is required.
In patients with moderate to severe hepatic and renal insufficiency, the metabolism of venlafaxine and the excretion of EDV is reduced, the Cmax of venlafaxine and EDV is increased, and T1/2 is prolonged. The decrease in the total clearance of venlafaxine is most pronounced in patients with renal creatinine clearance (CC) below 30 ml/min, as well as in patients on renal dialysis (T1/2 increases by 180% for venlafaxine and by 142% for EDV, and the clearance of both active substances decreases by approximately 57%). For such patients, especially on hemodialysis, individual selection of the dose of venlafaxine and monitoring of kinetics is necessary, taking into account the duration of treatment with this drug.
Although data for patients with severe Child-Pugh hepatic impairment are limited, it should be borne in mind that individual variations in pharmacokinetics, in particular drug clearance and T1/2, are very variable, which should be taken into account when prescribing venlafaxine to such patients.
In patients with Child-Pugh class A (mild liver dysfunction) and Child-Pugh class B (moderate impairment), T1/2 of venlafaxine and EDV are approximately 2 times longer than in healthy patients, and clearance is reduced by more than half.
Storage conditions
Storage conditions
Store in a place protected from light at a temperature not exceeding 25°C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years. Do not use after the expiration date stated on the package.
Manufacturer
Manufacturer
ALSI Pharma, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date printed on the package. |
|---|---|
| Conditions of storage | Store in the dark place at a temperature not exceeding 25°C. Store out of the reach of children. |
| Manufacturer | ALSI Pharma, Russia |
| Medication form | pills |
| Brand | ALSI Pharma |
Other forms…
Related products
Buy Venlafaxine-ALSI, tablets 75 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.