Subtotal: €63.56
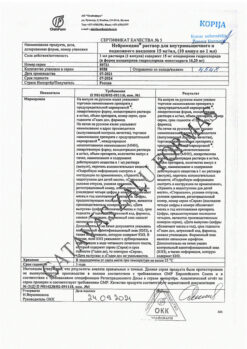
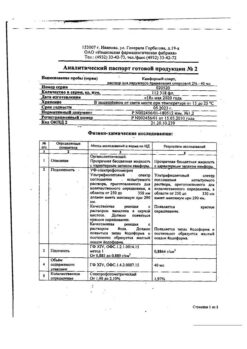
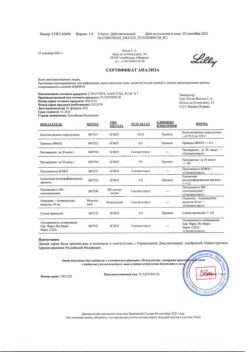
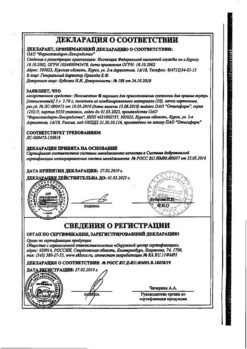
Topiramate-ALSI, 100 mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
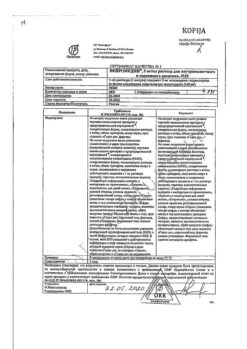
Pharmacotherapeutic group: Antiepileptic drug.
ATX code: N03AX11
Pharmacological properties
Pharmacodynamics
Topyramate is an antiepileptic drug belonging to the class of sulfamate-substituted monosaccharides.
Topiramate blocks sodium channels and suppresses the occurrence of repetitive action potentials against the background of prolonged depolarization of the neuron membrane. Topiramate increases the activity of gamma-aminobutyric acid (GABA) against several subtypes of GABA receptors (including GABAA-receptors), and also models the activity of GABAA-receptors, prevents kainat activation of kainat/AMPK (α-amino-3-hydroxy-5-methylisoxalol-4-propionic acid)-receptor subtype sensitivity to glutamate, and does not affect N-methyl-D-aspartate (NMDA) activity with respect to the NMDA-receptor subtype. These effects of topiramate are dose-dependent at plasma concentrations from 1 µmol to
200 µmol, with minimal activity between 1 µmol and 10 µmol.
In addition, topiramate inhibits the activity of some carboanhydrase isoenzymes. Topiramate is considerably inferior to acetazolamide, a known carbonic anhydrase inhibitor, in terms of the severity of this pharmacological effect; therefore, this activity of topiramate is not considered to be the main component of its antiepileptic activity.
Pharmacokinetics
absorption
Topiramate is absorbed rapidly and efficiently. Its bioavailability is 81%. Food intake has no clinically significant effect on the bioavailability of topiramate.
Distribution
13-17% of topiramate is bound to plasma proteins. After a single dose of up to 1200 mg the average volume of distribution is 0.55-0.8 l/kg. Distribution volume depends on sex: in women it is about 50% of that in men, which is associated with a higher content of adipose tissue in women.
Metabolism
After oral administration about 20% of the taken dose is metabolized. However, in patients receiving concomitant therapy with antiepileptic drugs that induce enzymes responsible for drug metabolism, the metabolism of topiramate is increased up to 50%.
Elimation
Six virtually inactive metabolites have been isolated and identified from human plasma, urine, and feces. The main route of excretion of unchanged topiramate (70%) and its metabolites is the kidneys. After oral administration the plasma clearance of topiramate is 20-30 ml/min.
Linearity/non-linearity
.The pharmacokinetics of topiramate are linear, plasma clearance remains constant, and the area under the concentration-time curve (AUC) in the
100 to 400 mg dose range increases in proportion to the dose. In patients with normal renal function, it may take 4 to 8 days to reach steady-state plasma concentrations. The value of maximum concentration (Cmax) after multiple oral doses of 100 mg of the drug twice a day averaged 6.76 mcg/ml. After multiple doses of 50 and 100 mg twice daily, the plasma half-life of topiramate averaged 21 hours.
Kidney function disorders
In patients with moderate to severe renal impairment, plasma and renal clearance of topiramate is decreased (creatinine clearance (Kk) ≤ 70 ml/min), as a consequence, the equilibrium plasma concentrations of topiramate may be higher compared to patients with normal renal function. In addition, patients with impaired renal function take longer to reach equilibrium blood concentrations of topiramate. In patients with moderate to severe renal impairment, half the recommended initial and maintenance doses are recommended.
Hemodialysis
Topiramate is effectively eliminated from plasma by hemodialysis. Prolonged hemodialysis may cause blood concentrations of topiramate to fall below the amount required to maintain anticonvulsant activity. An additional dose of topiramate may need to be administered to avoid a rapid drop in plasma concentrations during hemodialysis. When adjusting the dose, consideration should be given to:
- length of hemodialysis;
- the clearance rate of the hemodialysis system used;
- the effective renal clearance of topiramate in the patient on dialysis.
Hepatic disorders
The plasma clearance of topiramate is reduced by an average of 26% in patients with moderate to severe hepatic impairment. Therefore, patients with hepatic impairment should use topiramate with caution.
Elderly patients
In elderly patients without renal disease, the plasma clearance of topiramate is not altered.
Pharmacokinetics in children (children under 12 years of age)
The pharmacokinetic parameters of topiramate in children, as well as in adults receiving this drug as adjuvant therapy, are linear, with its clearance independent of the dose and equilibrium plasma concentrations increasing in proportion to increasing the dose. However, the fact that in children, topiramate clearance is higher and the elimination half-life is shorter should be taken into account. Therefore, at the same dose per 1 kg of body weight, plasma concentrations of topiramate in children may be lower than in adults. In children, as in adults, antiepileptic drugs that induce microsomal liver enzymes cause lower plasma concentrations of topiramate.
Indications
Epilepsy
As a monotherapy:
In adults and children over 3 years of age with epilepsy (including patients with newly diagnosed epilepsy).
As part of complex therapy:
In adults and children over 3 years of age with partial or generalized tonic-clonic seizures, as well as for the treatment of seizures associated with Lennox-Gastaut syndrome.
Migraine
Prevention of migraine attacks in adults. The use of topiramate for the treatment of acute migraine attacks has not been studied.
Pharmacological effect
Pharmacotherapeutic group: antiepileptic drug.
ATC code: N03AX11
Pharmacological properties
Pharmacodynamics
Topiramate is an antiepileptic drug belonging to the class of sulfamate-substituted monosaccharides.
Topiramate blocks sodium channels and suppresses the occurrence of repeated action potentials against the background of prolonged depolarization of the neuron membrane. Topiramate increases the activity of gamma-aminobutyric acid (GABA) in relation to certain subtypes of GABA receptors (including GABAA receptors), and also models the activity of GABAA receptors themselves, prevents activation by kainate of the sensitivity of the subtype kainate/AMPK (α-amino-3-hydroxy-5-methylisoxalol-4-propionic acid) receptors to glutamate, does not affect the activity N-methyl-D-aspartate (NMDA) in relation to the NMDA receptor subtype. These effects of topiramate are dose-dependent at drug plasma concentrations ranging from 1 µM to
200 µM, with trough activity ranging from 1 µM to 10 µM.
In addition, topiramate inhibits the activity of some carbonic anhydrase isoenzymes. In terms of the severity of this pharmacological effect, topiramate is significantly inferior to acetazolamide, a known inhibitor of carbonic anhydrase, therefore this activity of topiramate is not considered the main component of its antiepileptic activity.
Pharmacokinetics
Suction
Topiramate is absorbed quickly and efficiently. Its bioavailability is 81%. Food intake does not have a clinically significant effect on the bioavailability of topiramate.
Distribution
13-17% of topiramate is bound to plasma proteins. After a single dose of up to 1200 mg, the average volume of distribution is 0.55-0.8 l/kg. The value of the volume of distribution depends on gender: in women it is approximately 50% of the values observed in men, which is associated with a higher content of adipose tissue in the body of women.
Metabolism
After oral administration, about 20% of the dose taken is metabolized. However, in patients receiving concomitant therapy with antiepileptic drugs that induce enzymes responsible for drug metabolism, the metabolism of topiramate increases up to 50%.
Withdrawal
Six practically inactive metabolites were isolated and identified from human plasma, urine and feces. The main route of elimination of unchanged topiramate (70%) and its metabolites is the kidneys. After oral administration, plasma clearance of topiramate is 20-30 ml/min.
Linearity/non-linearity
The pharmacokinetics of topiramate is linear, plasma clearance remains constant, and the area under the concentration-time curve (AUC) in the dose range from
100 to 400 mg increases proportionally to the dose. In patients with normal renal function, it may take 4 to 8 days to achieve steady-state plasma concentrations. The maximum concentration (Cmax) after repeated oral administration of 100 mg of the drug twice a day averaged 6.76 mcg/ml. After multiple doses of 50 and 100 mg twice daily, the plasma half-life of topiramate averaged 21 hours.
Renal dysfunction
In patients with moderate to severe renal impairment, the plasma and renal clearance of topiramate is reduced (creatinine clearance (Kk) ≤ 70 ml/min), as a result, the equilibrium concentration of topiramate in the blood plasma may increase compared to patients with normal renal function. In addition, patients with impaired renal function require more time to achieve equilibrium concentrations of topiramate in the blood. For patients with moderate or severe renal impairment, half the recommended initial and maintenance dose is recommended.
Hemodialysis
Topiramate is effectively removed from plasma by hemodialysis. Long-term hemodialysis may result in a decrease in blood concentrations of topiramate below the amount required to maintain anticonvulsant activity. To avoid a rapid fall in plasma concentrations of topiramate during hemodialysis, an additional dose of topiramate may be required. When adjusting the dose, you should take into account:
duration of hemodialysis;
the clearance value of the hemodialysis system used;
effective renal clearance of topiramate in a patient on dialysis.
Liver dysfunction
Plasma clearance of topiramate is reduced by an average of 26% in patients with moderate or severe hepatic impairment. Therefore, patients with liver failure should use topiramate with caution.
Elderly patients
In elderly patients without renal disease, the plasma clearance of topiramate does not change.
Pharmacokinetics in childhood (in children under 12 years of age)
The pharmacokinetic parameters of topiramate in children, as well as in adults receiving this drug as adjuvant therapy, are linear, while its clearance does not depend on the dose, and equilibrium plasma concentrations increase in proportion to the dose. However, it should be taken into account that in children the clearance of topiramate is increased and its half-life is shorter. Therefore, at the same dose per 1 kg of body weight, plasma concentrations of topiramate in children may be lower than in adults. In children, as in adults, antiepileptic drugs that induce liver microsomal enzymes cause a decrease in plasma concentrations of topiramate.
Special instructions
Antiepileptic drugs, including Topiramate-ALSI, should be discontinued gradually to minimize the possibility of an increase in the frequency of seizures. To reduce the dose by 25-50 mg, use the drug Topiramate-ALSI at a dosage of 25 mg. In clinical studies, doses were reduced by 50-100 mg at weekly intervals for adults treated for epilepsy and by 25-50 mg in adults receiving 100 mg of Topiramate-ALSI per day for migraine prophylaxis. If, for medical reasons, rapid discontinuation of topiramate is necessary, it is recommended that appropriate monitoring of the patient’s condition be carried out.
As with other antiepileptic drugs, some patients taking topiramate experience an increase in the frequency of seizures or new types of seizures. This phenomenon may be a consequence of an overdose, a decrease in the concentration of concomitantly used antiepileptic drugs, disease progression, or a paradoxical effect. The rate of excretion through the kidneys depends on renal function and is independent of age. In patients with moderate or severe renal impairment, it may take 10 to 15 days to reach steady-state plasma concentrations, compared with 4 to 8 days in patients with normal renal function.
As with any disease, dose selection should be based on clinical effect (i.e., degree of seizure control, absence of side effects) and take into account that in patients with impaired renal function, a longer time may be required to establish stable plasma concentrations for each dose.
During treatment with topiramate, oligohidrosis (decreased sweating) and anhidrosis may occur. Decreased sweating and hyperthermia (increased body temperature) may occur in children exposed to high ambient temperatures. In this regard, when treating with topiramate, it is very important to adequately increase the volume of fluid intake, which can reduce the risk of developing nephrolithiasis, as well as side effects that may occur under the influence of physical activity or elevated temperatures.
Mood disorders/depression
An increased incidence of mood disorders and depression has been observed with topiramate treatment.
Suicidal attempts
When using antiepileptic drugs, including the drug Topiramate-ALSI, the risk of suicidal thoughts and suicidal behavior increases in patients taking these drugs for any of the indications.
In double-blind clinical studies, the incidence of suicide-related events (suicidal thoughts, suicide attempts, suicide) was 0.5% in patients receiving topiramate (46 of 8652 people), which is approximately 3 times higher compared to patients receiving placebo (0.2%: 8 of 4045 people). One suicide was reported in a double-blind study of bipolar disorder in a patient receiving topiramate.
It is therefore necessary to monitor patients for signs of suicidal ideation and prescribe appropriate treatment. Patients (and, if appropriate, caregivers) should be advised to seek immediate medical attention if signs of suicidal thoughts or behavior occur.
Nephrolithiasis
Some patients, especially those with a predisposition to nephrolithiasis, may have an increased risk of developing kidney stones and associated symptoms such as renal colic, kidney pain, or flank pain. To reduce this risk, an adequate increase in fluid intake is necessary. Risk factors for the development of nephrolithiasis are a history of nephrolithiasis (including family history), hypercalciuria, and concomitant therapy with drugs that contribute to the development of nephrolithiasis.
Impaired kidney function
Caution should be exercised when prescribing topiramate to patients with renal failure (creatinine clearance <70 ml/min). This is due to the fact that in such patients the clearance of the drug is reduced.
Liver dysfunction
In patients with impaired liver function, topiramate should be used with caution due to the possible decrease in clearance of this drug.
Myopia and secondary angle-closure glaucoma
When using topiramate, a syndrome has been described that includes acute myopia with concomitant secondary angle-closure glaucoma. Symptoms include acute loss of visual acuity and/or eye pain. An ophthalmological examination may reveal myopia, flattening of the anterior chamber of the eye, hyperemia (redness) of the eyeball, and increased intraocular pressure. Mydriasis may occur. This syndrome may be accompanied by fluid secretion, leading to forward displacement of the lens and iris with the development of secondary angle-closure glaucoma. Symptoms usually appear 1 month after starting use of Topiramate-ALSI. Unlike primary open-angle glaucoma, which is rarely observed in patients under 40 years of age, secondary angle-closure glaucoma is observed with the use of topiramate in both adults and children. If a syndrome involving myopia associated with angle-closure glaucoma occurs, treatment includes discontinuation of Topiramate-ALSI as soon as deemed possible by the attending physician and appropriate measures aimed at lowering intraocular pressure. Typically, these measures lead to normalization of intraocular pressure.
Increased intraocular pressure of any etiology, in the absence of adequate treatment, can lead to serious complications, including loss of vision.
When prescribing topiramate to patients with a history of eye diseases, it is necessary to assess the ratio of the expected benefit to the possible risk of use.
Visual field defects
Visual field defects have been observed in patients taking topiramate, regardless of whether they had elevated intraocular pressure. In clinical studies, most of these cases were reversible, and visual field defects disappeared after discontinuation of topiramate therapy. If vision problems occur while taking topiramate, discontinuation of therapy should be considered.
Metabolic acidosis
When using topiramate, hyperchloremic metabolic acidosis not associated with anion deficiency may occur (for example, a decrease in plasma bicarbonate concentrations below normal levels in the absence of respiratory alkalosis). This decrease in serum bicarbonate concentrations is a consequence of the inhibitory effect of topiramate on renal carbonic anhydrase. In most cases, a decrease in the concentration of bicarbonates occurs at the beginning of taking the drug, although this effect can occur at any time during treatment with topiramate. The degree of reduction in concentration is usually mild to moderate (average value is 4 mmol/L when used in adult patients at doses above
100 mg per day and about 6 mg per day per kg of body weight when used in pediatric practice). In rare cases, patients experienced a decrease in bicarbonate concentrations below 10 mmol/l. Certain medical conditions or treatments that predispose to the development of acidosis (eg, kidney disease, severe respiratory disease, status epilepticus, diarrhea, surgery, ketogenic diet, certain medications) may be additional factors that enhance the bicarbonate-lowering effect of topiramate.
In children, chronic metabolic acidosis can lead to growth retardation. The effect of topiramate on growth and possible complications related to the skeletal system have not been systematically studied in children and adults.
In connection with the above, when treating with topiramate, it is recommended to carry out the necessary studies, including determination of the concentration of bicarbonates in the serum. If symptoms of metabolic acidosis occur (eg, deep Kussmaul breathing, dyspnea, anorexia, nausea, vomiting, fatigue, tachycardia or arrhythmia), determination of serum bicarbonate concentrations is recommended. If metabolic acidosis occurs and persists, it is recommended to reduce the dose or stop taking topiramate.
Cognitive impairment
Impaired cognitive functions in epilepsy are multifactorial in nature and can be caused by the underlying cause of the disease, epilepsy itself or antiepileptic therapy. In adult patients taking topiramate, cases of cognitive impairment requiring dose reduction or discontinuation of therapy have been reported. Data on the effects of topiramate on cognitive function in children are insufficient, and its effects require further study.
Hyperammonemia and encephalopathy
When using topiramate, the development of hyperammonemia with or without encephalopathy was observed (see section “Side effects”). The risk of developing hyperammonemia with topiramate is dose-dependent. Hyperammonemia is more often observed with simultaneous use of topiramate and valproic acid (see section “Other drug interactions”).
Clinical symptoms of hyperammonemic encephalopathy often include severe impairment of consciousness and/or cognitive function and lethargy. In most cases, hyperammonemic encephalopathy regresses when therapy is discontinued. In patients who have developed lethargy or unexplained changes in mental status receiving topiramate as monotherapy or as part of combination therapy, it is recommended to take into account the possibility of hyperammonemic encephalopathy and determine the level of ammonia in the blood.
Enhanced nutrition
If a patient loses weight during treatment with Topiramate-ALSI, then it is necessary to consider the advisability of enhanced nutrition.
Influence on the ability to drive vehicles and machinery
Topiramate-ALSI acts on the central nervous system and may cause drowsiness, dizziness and other symptoms. It can also cause vision problems. These adverse events may pose a danger to patients driving cars and moving machinery, especially until the patient’s response to the drug is established.
Active ingredient
Topiramate
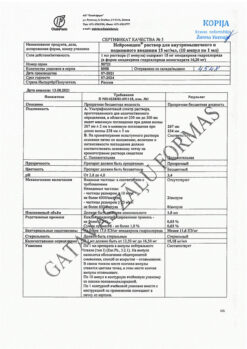
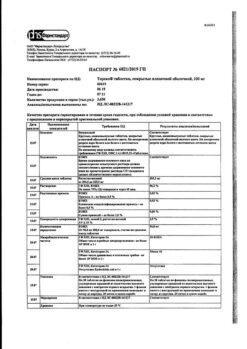
Composition
One film-coated tablet contains:
active ingredient: topiramate – 25.0 mg or 100.0 mg;
excipients: microcrystalline cellulose – 31.4/125.6 mg, pregelatinized starch – 23.0/92.0 mg, magnesium stearate – 0.4/1.6 mg, silicon dioxide colloidal (Aerosil) – 0.2/0.8 mg,
tablet shell: opadry II yellow (85F32830) – 3.2/12.8 mg (polyvinyl alcohol – 1.28/5.12 mg, macrogol (polyethylene glycol) – 0.65/2.60 mg, talc – 0.47/1.89 mg, titanium dioxide – 0.23/0.93 mg, quinoline yellow aluminum varnish dye – 0.53/2.10 mg and sunset yellow aluminum varnish dye – 0.04/0.16 mg).
Pregnancy
Pregnancy
Topiramate exhibited teratogenic properties in mice, rats and rabbits. In rats, topiramate penetrated the placental barrier.
There have been no specific controlled studies in which topiramate was used to treat pregnant women. Topiramate may cause fetal harm when used in pregnant women. Pregnancy data indicate that infants exposed to topiramate in utero during the first trimester of pregnancy have an increased risk of developing congenital malformations (eg, craniofacial defects such as cleft lip or palate, hypospadias, and developmental anomalies of various body systems). These malformations were recorded both during topiramate monotherapy and when it was used as part of polytherapy.
Data from one pregnancy registry showed that with topiramate monotherapy, the incidence of significant congenital malformations increases by approximately 3 times compared with a comparison group not taking antiepileptic drugs.
In addition, it has been shown that the risk of developing teratogenic effects associated with taking antiepileptic drugs is higher when using combination therapy than when using monotherapy.
Compared to a group of patients not taking antiepileptic drugs, data from pregnancies with topiramate monotherapy indicate an increased likelihood of having children with low body weight (less than 2500 g). One pregnancy registry showed an increase in the relative number of infants small for gestational age (SGA; defined as birth weight below the 10th percentile, adjusted for gestational age and stratified by sex) among infants exposed to topiramate in utero. The long-term consequences of NGB have not been determined. The cause of decreased birth weight and NGV has not been established.
During topiramate therapy, women of childbearing potential should use reliable methods of contraception.
The use of topiramate during pregnancy in women with uncontrolled epilepsy is justified only when the potential benefit of the drug for the mother outweighs the possible risk to the fetus. The use of topiramate for the prevention of migraine attacks is contraindicated during pregnancy, as well as in women with preserved childbearing potential who do not use reliable methods of contraception.
When treating and counseling women of childbearing potential, the treating physician should weigh the benefits and risks of treatment and consider alternative treatment options. If topiramate is used during pregnancy, or if the patient becomes pregnant while taking this drug, she should be warned of the potential risk to the fetus.
Breastfeeding
A limited number of patient observations suggests that topiramate is excreted into breast milk in women, so the physician should decide whether to breastfeed or discontinue the drug.
Fertility
In animal studies, no effect of topiramate on fertility was found. The effect of topiramate on fertility in humans has not been established.
Contraindications
Hypersensitivity to the active substance and to other components of the drug;
Children under 3 years of age;
The use of topiramate for the prevention of migraine attacks is contraindicated during pregnancy, as well as in women with preserved childbearing potential who do not use reliable methods of contraception.
With caution
Should be used with caution in case of renal and liver failure, nephrourolithiasis (including in the past or family history), hypercalciuria.
Side Effects
Adverse reactions are given with a distribution by frequency and organ system. The frequency of adverse reactions was classified as follows: very often (≥1/10); often (from ≥1/100 to <1/10); uncommon (from ≥1/1,000 to <1/100); rare (from ≥1/10,000 to <1/1,000); very rare (<1/10,000, including isolated cases) and frequency unknown (frequency cannot be estimated from available data).
The most common adverse reactions (the frequency of which was more than 5% and exceeded that in the placebo group for at least one of the indications during controlled clinical trials of topiramate) are: anorexia, decreased appetite, slow thinking, depression, impaired free speech, insomnia, impaired motor coordination, impaired concentration, dizziness, dysarthria, dysgeusia, hypoesthesia, lethargy, memory impairment, nystagmus, paresthesia, drowsiness, tremor, diplopia, blurred vision, diarrhea, nausea, fatigue, irritability and weight loss.
Infectious and parasitic diseases: very often – nasopharyngitis*.
Blood and lymphatic system disorders: often – anemia; uncommon – leukopenia, lymphadenopathy, thrombocytopenia, eosinophilia; rarely – neutropenia*.
Immune system disorders: often – hypersensitivity; frequency unknown – allergic edema*, conjunctival edema*.
Metabolism and nutritional disorders: often – anorexia, loss of appetite; uncommon – metabolic acidosis, hypokalemia, increased appetite, polydipsia; rarely – hyperchloremic acidosis, hyperammonemia, hyperammonemic encephalopathy.
Mental disorders: very often – depression; often – slow thinking, insomnia, impaired speech, anxiety, confusion, disorientation, aggressive reactions, mood disorders, agitation, emotional lability, depressed mood, anger, behavioral disturbances; uncommon – suicidal thoughts, suicide attempts, hallucinations, psychotic disorders, auditory hallucinations, visual hallucinations, apathy, difficulty speaking, sleep disturbances, affective lability, decreased libido, agitation, crying, dysphemia, euphoric mood, paranoia, perseveration of thinking, panic attacks, tearfulness, impaired reading skills, difficulty falling asleep, flattening emotions, pathological thinking, loss of libido, lethargy, intrasomnic disorder, absent-mindedness, early morning awakenings, panic reactions, high spirits; rarely – mania, panic disorder, feelings of hopelessness*, hypomania.
Nervous system disorders: very often – paresthesia, drowsiness, dizziness; often – impaired concentration, memory impairment, amnesia, cognitive disorders, impaired thinking, psychomotor impairment, convulsions, incoordination, tremor, lethargy, hypoesthesia, nystagmus, dysgeusia, impaired sense of balance, dysarthria, intention tremor, sedation; uncommon – depressed consciousness, tonic-clonic seizures of the “grand mal” type, visual field impairment, complex partial seizures, speech impairment, psychomotor hyperactivity, fainting, sensory disturbances, drooling, hypersomnia, aphasia, repetitive speech, hypokinesia, dyskinesia, postural dizziness, poor quality of sleep, burning sensation, loss of sensitivity, parosmia, cerebral syndrome, dysesthesia, hypogeusia, stupor, clumsiness, aura, ageusia, dysgraphia, dysphasia, peripheral neuropathy, presyncope, dystonia, sensation of “pins and needles” throughout the body; rarely – apraxia, disturbance of the circadian rhythm of sleep, hyperesthesia, hyposmia, anosmia, essential tremor, akinesia, lack of reactions to stimuli.
Visual disorders: often – blurred vision, diplopia, visual impairment; uncommon – decreased visual acuity, scotoma, myopia*, strange sensations in the eyes*, dry eyes, photophobia, blepharospasm, increased lacrimation, photopsia, mydriasis, presbyopia; rarely – one-sided blindness, transient blindness, glaucoma, impaired accommodation, impaired visual spatial perception, atrial scotoma, eyelid edema*, night blindness, amblyopia; frequency unknown – angle-closure glaucoma*, maculopathy*, eye mobility disorders*.
Hearing and labyrinthine disorders: often – vertigo, tinnitus, ear pain; uncommon – deafness, one-sided deafness, sensorineural deafness, ear discomfort, hearing impairment.
Heart disorders: uncommon – bradycardia, sinus bradycardia, palpitations.
Vascular disorders: uncommon – hypotension, orthostatic hypotension, hot flashes, hot flushes; rarely – Raynaud’s phenomenon.
Disorders of the respiratory system, chest and mediastinal organs: often – shortness of breath, nosebleeds, nasal congestion, rhinorrhea, cough*; uncommon – shortness of breath on exertion, hypersecretion in the paranasal sinuses, dysphonia.
Gastrointestinal tract disorders: very often – nausea, diarrhea; often – vomiting, constipation, pain in the epigastric region, dyspepsia, abdominal pain, dry mouth, stomach discomfort, impaired sensitivity in the oral cavity, gastritis, abdominal discomfort; uncommon – pancreatitis, flatulence, gastroesophageal reflux, pain in the lower abdomen, decreased sensitivity in the oral cavity, bleeding gums, bloating, discomfort in the epigastric region, sensitivity in the abdominal area, hypersalivation, pain in the oral cavity, bad breath, glossodynia.
Disorders of the liver and biliary tract: rarely – hepatitis, liver failure.
Skin and subcutaneous tissue disorders: often – alopecia, rash, itching; infrequently – anhidrosis, impaired sensitivity in the facial area, urticaria, erythema, generalized itching, macular rash, skin pigmentation disorder, allergic dermatitis, facial swelling; uncommon – Stevens-Johnson syndrome*, erythema multiforme*, change in skin odor, periorbital edema*, localized urticaria; frequency unknown – toxic epidermal necrolysis*.
Musculoskeletal and connective tissue disorders: often – arthralgia, muscle spasms, myalgia, muscle cramps, muscle weakness, musculoskeletal chest pain; uncommon – joint swelling*, muscle stiffness, side pain, muscle fatigue; rarely – discomfort in the limbs*.
Disorders of the kidneys and urinary tract: often – nephrolithiasis, pollakiuria, dysuria; uncommon – exacerbation of urolithiasis (kidney stones), stress urinary incontinence, hematuria, urinary incontinence, frequent urge to urinate, renal colic, pain in the kidney area; rarely – exacerbation of urolithiasis (stones in the urethra), renal tubular acidosis*.
Genital and breast disorders: uncommon – erectile dysfunction, sexual dysfunction.
General disorders and disorders at the injection site: very often – fatigue; often – increased body temperature, asthenia, irritability, gait disturbances, poor health, anxiety; uncommon – hyperthermia, thirst, flu-like syndrome*, slowness, cold extremities, feeling of intoxication, feeling of restlessness; rarely – facial swelling, calcification.
Influence on the results of laboratory and instrumental studies: very often – loss of body weight; often – weight gain*; uncommon – crystalluria, abnormal tandem gait test result, leukopenia, increased activity of liver enzymes in the blood serum; rarely – a decrease in the content of bicarbonates in the blood.
Influence on social factors: infrequently – learning disability.
* – an adverse reaction was registered in the post-registration period from spontaneous reports. Frequency calculated based on data from clinical studies.
Special groups:
Children:
The following is a list of adverse reactions that, during controlled clinical studies, were recorded in children 2 or more times more often than in adults: decreased appetite, increased appetite, hyperchloremic acidosis, hypokalemia, behavioral disturbances, aggressive reactions, apathy, difficulty falling asleep, suicidal ideation, impaired concentration, lethargy, disturbance of the circadian rhythm of sleep, poor quality of sleep, increased lacrimation, sinus bradycardia, poor health, gait disturbances.
The following is a list of adverse reactions that were recorded only in children during controlled clinical trials: eosinophilia, psychomotor hyperactivity, vertigo, vomiting, pyrexia, pyrexia, learning disability.
Interaction
Effect of topiramate on concentrations of other antiepileptic drugs (AEDs)
Concomitant use of topiramate with other AEDs (phenytoin, carbamazepine, valproic acid, phenobarbital, primidone) does not affect the values of their equilibrium concentrations in plasma, with the exception of certain patients in whom the addition of topiramate to phenytoin may cause an increase in the concentration of phenytoin in plasma. This may be due to inhibition of a specific polymorphic isoform of the cytochrome P450 enzyme (CYP2C19 isoenzyme). Therefore, phenytoin plasma concentrations should be monitored in any patient taking phenytoin who develops clinical signs or symptoms of toxicity. In a pharmacokinetic study in patients with epilepsy, the addition of topiramate to lamotrigine did not affect the steady-state concentration of the latter at doses of topiramate 100-400 mg per day. During therapy and after discontinuation of lamotrigine (average dose 327 mg per day), the equilibrium concentration of topiramate did not change.
Effect of other antiepileptic drugs on topiramate concentrations
Phenytoin and carbamazepine reduce plasma concentrations of topiramate. The addition or removal of phenytoin or carbamazepine during treatment with Topiramate-ALSI may require a change in the dose of the latter. The dose should be selected based on achieving the desired clinical effect. The addition or removal of valproic acid does not cause clinically significant changes in the plasma concentration of topiramate and, therefore, does not require a change in the dose of Topiramate-ALSI.
The results of these interactions are summarized in the following table:
Added probe
PEP concentration
Concentration of the drug Topiramate-ALSI
Phenytoin
↔**
↓ (48%)
Carbamazepine
↔
↓ (40%)
Valproic acid
↔
↔
Phenobarbital
↔
NOR
Primidone
↔
NOR
↔ = no effect;
** = increased concentration in isolated patients;
↓ = decrease in plasma concentration;
NOR = not studied;
AED = antiepileptic drug.
Other drug interactions
Digoxin: In a single-dose study, the area under the plasma concentration-time curve (AUC) of digoxin decreased by 12% when coadministered with topiramate. The clinical significance of this observation is unclear. When prescribing or discontinuing the drug Topiramate-ALSI in patients taking digoxin, special attention should be paid to monitoring the concentration of digoxin in the serum.
CNS depressants: The effects of concomitant use of topiramate with alcohol or other CNS depressants have not been studied in clinical trials. It is recommended not to take Topiramate-ALSI together with alcohol or other drugs that cause depression of central nervous system function.
Hypericum perforatum
When taking topiramate and drugs based on St. John’s wort (Hypericum perforatum L.) together, the concentration of topiramate in plasma may decrease and, as a result, the effectiveness of the drug may also decrease. Clinical studies of the interaction of the drug Topiramate-ALSI and drugs based on St. John’s wort have not been conducted.
Oral contraceptives: In a drug interaction study with oral contraceptives using a combination product containing norethisterone (1 mg) and ethinyl estradiol (35 mcg), topiramate at doses of 50-800 mg per day had no significant effect on the effectiveness of norethisterone and at doses
50-200 mg per day on the effectiveness of ethinyl estradiol. A significant dose-dependent decrease in the effectiveness of ethinyl estradiol was observed at doses of topiramate
200-800 mg per day. The clinical significance of the described changes is unclear. The risk of decreased contraceptive effectiveness and increased breakthrough bleeding should be taken into account in patients taking oral contraceptives in combination with Topiramate-ALSI. Patients taking estrogen-containing contraceptives should be informed of any changes in the timing and nature of menstruation. The effectiveness of contraceptives may be reduced even in the absence of breakthrough bleeding.
Lithium: In healthy volunteers, an 18% decrease in lithium AUC was observed when co-administering topiramate 200 mg daily. In patients with manic-depressive psychosis, the use of topiramate in doses up to 200 mg per day did not affect the pharmacokinetics of lithium, however, at higher doses (up to 600 mg per day), the AUC of lithium was increased by 26%. When using topiramate and lithium simultaneously, the concentration of the latter in the blood plasma should be monitored.
Risperidone: Drug interaction studies conducted with single and multiple doses of topiramate in healthy volunteers and patients with bipolar disorder yielded similar results. When co-administered with topiramate at doses of 250 or 400 mg per day, the AUC of risperidone taken at doses of 1-6 mg per day is reduced by 16% and 33%, respectively. At the same time, the pharmacokinetics of 9-hydroxyrisperidone did not change, and the total pharmacokinetics of the active substances (risperidone and 9-hydroxyrisperidone) changed slightly. The change in systemic exposure of risperidone/9-hydroxyrisperidone and topiramate was not clinically significant and this interaction is unlikely to be of clinical significance.
Hydrochlorothiazide: drug interactions were assessed in healthy volunteers with the separate and combined use of hydrochlorothiazide (25 mg) and topiramate (96 mg). Study results showed that when topiramate and hydrochlorothiazide were taken concomitantly, the maximum concentration of topiramate increased by 27% and the area under the AUC curve of topiramate increased by 29%. The clinical significance of these studies has not been established. Prescribing hydrochlorothiazide to patients taking topiramate may require a dose adjustment of topiramate. The pharmacokinetic parameters of hydrochlorothiazide were not significantly altered by concomitant therapy with topiramate.
Metformin: Drug interactions were assessed in healthy volunteers receiving metformin or a combination of metformin and topiramate. Study results showed that when topiramate and metformin were co-administered, the maximum concentration and area under the AUC curve of metformin increased by 18% and 25%, respectively, while the clearance of metformin when used concomitantly with topiramate decreased by 20%. Topiramate had no effect on the time to reach maximum metformin plasma concentrations. The clearance of topiramate is reduced when used concomitantly with metformin. The extent of the observed changes in clearance has not been studied. The clinical significance of the effect of metformin on the pharmacokinetics of topiramate is unclear. If Topiramate-ALSI is added or discontinued in patients receiving metformin, the patient’s condition should be carefully monitored to assess the course of diabetes mellitus.
Pioglitazone: drug interactions were assessed in healthy volunteers with the separate and simultaneous use of pioglitazone and topiramate. A decrease in the area under the AUC curve of pioglitazone by 15% was detected, without changing the maximum concentration of the drug. These changes were not statistically significant. The active hydroxymetabolite pioglitazone also showed a 13% and 16% decrease in maximum concentration and AUC, respectively, and the active ketometabolite showed a 60% decrease in maximum concentration and AUC. The clinical significance of these data is unclear. When patients use Topiramate-ALSI and pioglitazone simultaneously, the patient’s condition should be carefully monitored to assess the course of diabetes mellitus.
Glibenclamide: A drug interaction study was conducted to examine the pharmacokinetics of glibenclamide (5 mg daily) at steady state, administered alone or concomitantly with topiramate (150 mg daily) in patients with type 2 diabetes mellitus. When topiramate was used, the AUC of glibenclamide decreased by 25%. Systemic exposure to 4-trans-hydroxy-glibenclamide and 3-cis-hydroxy-glibenclamide was also reduced (by 13% and 15%, respectively). Glibenclamide did not affect the pharmacokinetics of topiramate at steady state. A statistically insignificant decrease in the AUC of pioglitazone by 15% was detected with no change in Cmax. When prescribing topiramate to patients receiving glibenclamide (or prescribing glibenclamide to patients receiving topiramate), the patient’s condition should be carefully monitored to assess the course of diabetes mellitus.
Other drugs: simultaneous use of Topiramate-ALSI with drugs that predispose to nephrolithiasis may increase the risk of kidney stones. During treatment with Topiramate-ALSI, the use of drugs that predispose to nephrolithiasis should be avoided, as they may cause physiological changes that contribute to nephrolithiasis.
Valproic acid: the combined use of topiramate and valproic acid in patients who tolerate each drug separately is accompanied by hyperammonemia with or without encephalopathy. In most cases, symptoms and signs disappear after discontinuation of one of the drugs (see section “Special instructions” and “Side effects”). This adverse reaction is not due to a pharmacokinetic interaction.
When topiramate and valproic acid are taken together, hypothermia (an unintentional decrease in body temperature below 35°C) may occur in combination with hyperammonemia or independently. This phenomenon can occur both after the start of joint use of valproic acid and topiramate, and with an increase in the daily dose of topiramate.
Additional drug interaction studies: A number of clinical studies have been conducted to evaluate potential drug interactions between topiramate and other drugs.
The results of these interactions are summarized in the following table:
Added drug
Concentration of added drug
Concentration of topiramatea
Amitriptyline
increase in maximum concentration and AUC of nortriptyline metabolite by 20%
not studied
Dihydroergotamine
(oral and subcutaneous)
↔
↔
Haloperidol
increase in metabolite AUC by 31%
not studied
Propranolol
increase in maximum concentration for 4-OH propranolol by 17% (topiramate 50 mg)
increase in maximum concentration by 9% and 16%, increase in AUC by 9% and 17%, respectively (for propranolol 40 mg and 80 mg every 12 hours)
Sumatriptan
(oral and subcutaneous)
↔
not studied
Pizotifen
↔
↔
Diltiazem
decrease in AUC of diltiazem by 25% and decrease in desacetyldiltiazem by 18%, and ↔ for N-demethyldiltiazem
AUC increase by 20%
Venlafaxine
↔
↔
Flunarizine
16% increase in AUC
(50 mg every 12 hours)b
↔
a = expressed as % of the values of maximum plasma concentration and AUC during monotherapy;
↔ = no change in maximum plasma concentration and AUC (≤ 15% of baseline);
b = with repeated administration of flunarizine alone, an increase in AUC of 14% was observed, which may be due to accumulation of the drug during the process of reaching an equilibrium state.
Overdose
Symptoms
Signs and symptoms of topiramate overdose: convulsions, drowsiness, speech and vision disturbances, diplopia, impaired thinking, impaired motor coordination, lethargy, stupor, hypotension, abdominal pain, dizziness, agitation and depression. In most cases, the clinical consequences were not severe, but deaths have been reported after overdose using a mixture of several drugs, including topiramate. An overdose of topiramate can cause severe metabolic acidosis (see section “Special Instructions”).
There is a known case of overdose when the patient took a dose of topiramate from 96 to 110 g, which resulted in a coma that lasted 20-24 hours. After 3-4 days, the patient’s condition returned to normal.
Treatment
In case of acute overdose of topiramate, if the patient has eaten shortly before, it is necessary to immediately rinse the stomach or induce vomiting. Activated carbon has been shown to adsorb topiramate in in vitro studies. If necessary, symptomatic therapy should be carried out. An effective way to remove topiramate from the body is hemodialysis. Patients are advised to adequately increase their fluid intake.
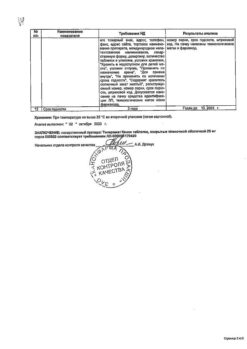
Storage conditions
At a temperature not exceeding 25ºС in original packaging.
Keep out of the reach of children.
Shelf life
3 years. Do not use after the expiration date stated on the package.
Manufacturer
ALSI Pharma, Russia
| Shelf life | 3 years. Do not use after the expiration date stated on the package. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25ºC in the original package. Keep out of reach of children. |
| Manufacturer | ALSI Pharma, Russia |
| Medication form | pills |
| Brand | ALSI Pharma |
Other forms…
Related products
Buy Topiramate-ALSI, 100 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.