No products in the cart.
Tebantin, 300 mg capsules 100 pcs
€62.94 €52.45
Description
Gabapentin has a structure similar to the neurotransmitter gamma-aminobutyric acid (GABA). It is a lipophilic substance. Only the mechanism of action is different from that of some other similar drugs which interact with GABA receptors, including valproic acid preparations, barbiturates, benzodiazepines, GABA transferase inhibitors, GABA capture inhibitors, GABA agonists and prodrug forms of GABA: it does not have GABA-ergic properties and does not affect GABA capture and metabolism.
The results of preliminary studies suggest that gabapentin binds to the α2-δ subunit of potential-dependent calcium channels and suppresses calcium ion flux, which plays an important role in causing neuropathic pain.
There are also other mechanisms that are involved in the action of gabapentin in neuropathic pain: reduction of glutamate-dependent neuronal death, increased synthesis of GABA, suppression of monoamine group neurotransmitter release.
Gabapentin in clinically relevant concentrations does not bind to receptors for other common drugs or transmitters, including GABAA and GABAB, benzodiazepine receptors, glutamate, glycine or NMDA.
Unlike phenytoin and carbamazepine, gabapentin does not interact with sodium channels in vitro. Gabapentin partially attenuated the effects of glutamate NMDA receptor agonist in some in vitro tests, but only at concentrations greater than 100 μmol, which are not achieved in vivo.
Gabapentin slightly reduces the release of monoamine neurotransmitters and modifies the activity of GABA synthetase and glutamate synthetase enzymes in vitro.
In a study of gabapetin in rats, it was found to increase GABA metabolism in some parts of the brain; this effect was similar to that of valproic acid, although it was observed in other parts of the brain.
The significance of these effects of gabapentin for its anticonvulsant activity has not been established. In animals, gabapentin readily penetrates brain tissue and prevents seizures induced by maximal electroshock, chemicals including GABA synthesis inhibitors, and genetic factors.
Indications
Indications
Partial seizures with or without secondary generalization in adults and children over 12 years of age as monotherapy or adjunctive therapy;
partial seizures with or without secondary generalization in children from 3 to 12 years old as additional therapy;
neuropathic pain in patients over 18 years of age (efficacy and safety in patients under 18 years of age have not been established).
Pharmacological effect
Pharmacological effect
Gabapentin is structurally similar to the neurotransmitter gamma-aminobutyric acid (GABA). It is a lipophilic substance. Only its mechanism of action differs from that of some other similar drugs that interact with GABA receptors, including valproic acid drugs, barbiturates, benzodiazepines, GABA transferase inhibitors, GABA uptake inhibitors, GABA agonists and GABA prodrugs: it does not have GABAergic properties and does not affect the uptake and metabolism of GABA.
Preliminary studies suggest that gabapentin binds to the α2-δ subunit of voltage-gated calcium channels and inhibits the flow of calcium ions, which plays an important role in neuropathic pain.
There are also other mechanisms that are involved in the action of gabapentin in neuropathic pain: a decrease in glutamate-dependent neuronal death, an increase in GABA synthesis, and suppression of the release of monoamine group neurotransmitters.
Gabapentin at clinically relevant concentrations does not bind to the receptors of other common drugs or transmitters, including the GABAA and GABAB, benzodiazepine, glutamate, glycine, or NMDA receptors.
Unlike phenytoin and carbamazepine, gabapentin does not interact with sodium channels in vitro. Gabapentin partially attenuated the effects of the NMDA glutamate receptor agonist in some in vitro tests, but only at concentrations greater than 100 μM, which is not achieved in vivo.
Gabapentin slightly reduces the release of monoamine neurotransmitters and modifies the activity of the enzymes GABA synthetase and glutamate synthetase in vitro.
A study of gabapetin in rats found an increase in GABA metabolism in some areas of the brain; this effect was similar to that of valproic acid, although it was observed in other areas of the brain.
The significance of these effects of gabapentin for its anticonvulsant activity has not been established. In animals, gabapentin easily penetrates brain tissue and prevents seizures caused by maximum electric shock, chemicals, including GABA synthesis inhibitors, and those caused by genetic factors.
Special instructions
Special instructions
In the process of selecting the optimal therapeutic dose, there is no need to measure the concentration of the drug in plasma.
The drug is ineffective for absence seizures.
When using gabapentin, monitoring blood glucose levels in patients with diabetes mellitus is necessary; Sometimes it becomes necessary to change the dose of a hypoglycemic drug.
When the first signs of acute pancreatitis appear (prolonged abdominal pain, nausea, repeated vomiting), treatment with gabapentin should be stopped. A thorough examination of the patient (clinical and laboratory tests) should be carried out for the purpose of early diagnosis of acute pancreatitis.
If you are lactose intolerant, please note that 1 caps. (100 mg) contains 22.14 mg of lactose, 1 cap. (300 mg) – 66.42 mg of lactose, and 1 cap. (400 mg) – 88.56 mg lactose.
The dose should be reduced, discontinued, or replaced with another alternative agent gradually over a period of at least 1 week. Abrupt cessation of therapy may provoke status epilepticus.
If drowsiness, ataxia, dizziness, increased fatigue, nausea and/or vomiting, weight gain occur in adults, and drowsiness, hyperkinesia and hostility in children, you should stop taking the drug and consult your doctor.
Use in pediatrics
The safety and effectiveness of gabapentin in children under 3 years of age as adjunctive therapy for epilepsy and in children under 12 years of age as monotherapy have not been established.
The safety and effectiveness of treatment for neuropathic pain in patients under 18 years of age have not been established.
Impact on the ability to drive vehicles and operate machinery
During the treatment period, patients must refrain from driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Gabapentin
Composition
Composition
1 capsule contains:
Pregnancy
Pregnancy
There are no data on the use of the drug during pregnancy, therefore Tebantin® should be used in pregnant women only if the expected benefit to the mother outweighs the possible risk to the fetus.
Gabapentin is excreted in breast milk. The effect of gabapentin on breastfed children is unknown, therefore, if it is necessary to use the drug during lactation, breastfeeding should be discontinued
Use in children
Contraindicated in children under 3 years of age.
The use of Tebantin® as monotherapy is contraindicated in children aged 3 to 12 years.
Contraindications
Contraindications
Acute pancreatitis;
monotherapy in children aged 3 to 12 years;
children under 3 years of age;
lactation period (breastfeeding);
lactase deficiency, lactose intolerance, glucose/galactose malabsorption (the dosage form of the drug contains lactose);
hypersensitivity to the components of the drug.
The drug should be prescribed with caution to patients with renal failure.
Use for renal impairment
The drug should be prescribed with caution to patients with renal failure.
Recommended doses of gabapentin for renal impairment
Creatinine clearance (ml/min)
Daily dose of gabapentin for 3 doses (mg/day)
≥80 ml/min
900-2400
50-79
600-1800
30-49
300-900
15-29
150*-600
150*-300
*- take 100 mg of the drug 3 times a day every other day.
For patients on hemodialysis who have not previously taken gabapentin, it is recommended to prescribe a loading dose of 300-400 mg, then prescribe 200-300 mg of the drug every 4 hours of hemodialysis. Gabapentin should not be taken on dialysis-free days.
Use in elderly patients
In elderly patients, in accordance with the age-related decrease in CC, the dose should be selected individually.
Side Effects
Side Effects
In the treatment of partial seizures
From the central nervous system and peripheral nervous system: drowsiness, dizziness, headache, amnesia, ataxia, depression, emotional lability, increased nervous excitability, nystagmus (dose-dependent), tremor, muscle twitching, hyperkinesis, dysarthria, incoordination, hallucinations, movement disorders (choreoathetosis, dyskinesia, dystonia), impaired thinking, confusion, tics, paresthesia (dose-dependent), hyperkinesia, increased, weakened or absent reflexes, anxiety, restlessness, hostility, insomnia. In addition, hostility and hyperkinesia were noted in children under 12 years of age.
From the digestive system: nausea, vomiting, abdominal pain, dyspepsia, increased appetite, dry mouth or pharynx, constipation, diarrhea, dental lesions, pancreatitis, hepatitis, jaundice, increased activity of liver transaminases, flatulence, anorexia, gingivitis, discoloration of tooth enamel.
From the cardiovascular system: palpitations, symptoms of vasodilation. When prescribed with other drugs – increased blood pressure.
From the hematopoietic system: leukopenia, thrombocytopenia.
From the musculoskeletal system: arthralgia, myalgia, fractures.
From the respiratory system: pharyngitis, rhinitis, when prescribed with other antiepileptic drugs – cough, pneumonia.
From the senses: visual impairment (amblyopia, diplopia), tinnitus.
From the urinary system: urinary incontinence, acute renal failure, when prescribed with other antiepileptic drugs – urinary tract infection.
From the reproductive system: impotence, enlargement of the mammary glands, gynecomastia.
From the metabolic side: weight gain, facial swelling, peripheral edema, generalized edema, fluctuations in blood glucose concentration in patients with diabetes.
Allergic reactions: skin rash, itching, urticaria, fever, angioedema, erythema multiforme (including Stevens-Johnson syndrome).
Dermatological reactions: purpura, acne, alopecia.
Other: back pain, chest pain, fever, fatigue, flu-like syndrome, asthenia, malaise.
In the treatment of neuropathic pain
From the digestive system: constipation, diarrhea, dyspepsia, dry mouth, flatulence, nausea, vomiting, abdominal pain.
From the central nervous system and peripheral nervous system: gait disturbance, disorientation, paresthesia, drowsiness, impaired thinking, tremor, headache.
From the respiratory system: shortness of breath, pharyngitis.
Dermatological reactions: skin rash.
From the senses: amblyopia.
Metabolism: peripheral edema, weight gain.
Other: accidental injuries, asthenia, back pain, flu-like syndrome, headache, infections, pain of various localizations.
After abrupt discontinuation of gabapentin therapy, the most frequently reported symptoms were anxiety, insomnia, nausea, pain of various localizations, and increased sweating.
Interaction
Interaction
No interactions were observed between gabapentin and phenytoin, carbamazepine, valproic acid and phenobarbital. The pharmacokinetics of gabapentin at steady state are similar in healthy subjects and patients receiving other antiepileptic drugs.
Gabapentin does not affect the pharmacokinetics and effectiveness of oral contraceptives containing norethisterone and/or ethinyl estradiol. However, a reduction/cessation of the contraceptive effect of these drugs is possible when combining Tebantin® with other antiepileptic drugs that reduce the effectiveness of oral contraceptives.
Gastric acid neutralizers containing magnesium or aluminum reduce the bioavailability of gabapentin by 24%. Tebantin® capsules should be taken 2 hours after taking antacids.
When cimetidine is combined with gabapentin, the excretion of the latter by the kidneys is slightly reduced, which probably has no clinical significance.
Other drugs that affect the central nervous system, as well as ethanol, can enhance the side effects of gabapentin on the central nervous system (for example, drowsiness, ataxia).
Probenecid does not affect the renal excretion of gabapentin.
When gabapentin and morphine were taken together, when morphine in the form of controlled-release capsules of 60 mg was taken 2 hours before taking gabapentin, an increase in AUC of gabapentin by 44% was observed compared with gabapentin monotherapy, which was accompanied by an increase in the pain threshold (cold pressor test).
The clinical significance of these changes has not been established. When gabapentin was administered 2 hours after morphine administration, no changes in the pharmacokinetic parameters of morphine were observed. The side effects of morphine when coadministered with gabapentin were no different from those observed when morphine was taken with placebo.
False-positive results have been reported when gabapentin is added to other anticonvulsants when urinary total protein is determined using semiquantitative tests. If positive results are obtained with such tests, it is recommended to use the more specific precipitation method of sulfosalicylic acid or biuret test.
Overdose
Overdose
Symptoms: dizziness, double vision, drowsiness, dysarthria, lethargy and diarrhea. Symptoms of acute, life-threatening poisoning were not observed even after daily intake of 49 g of the drug.
Treatment: carrying out symptomatic therapy. Hemodialysis may be indicated for patients with severe renal failure.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C
Shelf life
Shelf life
5 years
Manufacturer
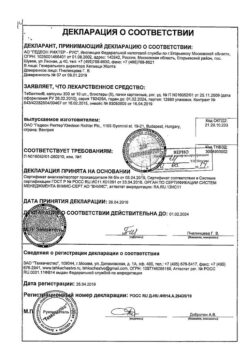
Manufacturer
Gedeon Richter, Hungary
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | Gedeon Richter, Hungary |
| Medication form | capsules |
| Brand | Gedeon Richter |
Other forms…
Related products
Buy Tebantin, 300 mg capsules 100 pcs with delivery to USA, UK, Europe and over 120 other countries.