No products in the cart.
Solian, 400 mg 30 pcs.
€221.70 €192.14
Description
Solian is an antipsychotic (neuroleptic)
Pharmacodynamics
. Amisulpride binds selectively, with high affinity, to D2/D3 subtypes of dopaminergic receptors, whereas it has no affinity for D1 D4 and D5 subtypes.
Unlike classical and atypical neuroleptics, amisulpride has no affinity for serotonin, histamine H1, alpha-adrenergic and cholinergic receptors. In addition, amisulpride does not bind to sigma receptors. When used in high doses, it blocks postsynaptic D2 receptors located in limbic structures, unlike similar receptors in the striatum. It does not cause catalepsy and does not lead to development of hypersensitivity of D2-dopamine receptors after repeated treatment.
In low doses, it predominantly blocks presynaptic D2/D3 receptors, causing the release of dopamine responsible for its disinhibitory effects. This atypical pharmacological profile may explain the antipsychotic effects of amisulpride at high doses resulting from blockade of postsynaptic dopamine receptors and its effectiveness against negative symptoms at low doses resulting from blockade of presynaptic dopamine receptors.
In addition, amisulpride is less likely to cause extrapyramidal side effects, which may be due to its predominant limbic activity.
In schizophrenic patients with acute seizures, Solian acts both on secondary negative symptoms and on affective symptoms such as depressed mood and retardation.
Pharmacokinetics
Amisulpride has two absorption peaks: one is reached rapidly, one hour after administration of the dose, and the second between 3 and 4 hours after administration. Plasma concentrations are 39 ± 3 and 54 ± 4 ng/mL, respectively, after administration of 50 mg.
The volume of distribution is 5.8 l/kg. Since the binding to plasma proteins is low (16%), interaction with other drugs is unlikely.
The absolute bioavailability is 48%. Amisulpride is poorly metabolized: (about 4%, two inactive metabolites have been identified. There is no cumulation of amisulpride and its pharmacokinetics remain unchanged after repeated doses.
The half-life (T1/2) of amisulpride is approximately 12 hours after an oral dose.
Amisulpride is excreted unchanged in the urine. Renal clearance is approximately 20 l/hour or 330 ml/min.
Carbohydrate-rich foods (containing 68% liquid) significantly decrease the AUC (area under the concentration-time curve), time to reach maximum concentration and maximum concentration of amisulpride itself, but no changes in pharmacokinetics were noted after eating fatty foods. However, the significance of these observations in routine clinical practice is unknown.
Hepatic impairment. Due to the fact that the drug is poorly metabolized, there is no need to reduce the dose for patients with hepatic impairment.
Hepatic impairment. The T1/2 in patients with renal impairment is not altered, but systemic clearance is reduced by a factor of 2.5 to 3. The AUC of amisulpride is doubled in mild renal insufficiency and almost tenfold in moderate insufficiency (see section Dosage and administration). Practical experience is limited, however, and there are no results for doses greater than 50 mg.
Amisulpride is poorly tolerated by dialysis.
Limited pharmacokinetic data for elderly (older than 65 years) patients indicate that Cmax, T1/2, and AUC are 10-30% higher after a single oral administration of 50 mg than in younger individuals. There are no data on the pharmacokinetics of the drug during long-term treatment.
Indications
Indications
Acute and chronic schizophrenia, accompanied by severe productive (including delusions, hallucinations, thinking disorders) and/or negative (including affective flatness, lack of emotionality and withdrawal from communication) disorders, incl. in patients with a predominance of negative symptoms.
Pharmacological effect
Pharmacological effect
Solian – antipsychotic drug (neuroleptic)
Pharmacodynamics
Amisulpride selectively binds with high affinity to subtypes D2/D3 of dopaminergic receptors, while it has no affinity for subtypes D1, D4 and D5.
Unlike classical and atypical antipsychotics, amisulpride has no affinity for serotonin, histamine H1, alpha-adrenergic and cholinergic receptors. In addition, amisulpride does not bind to sigma sites. When used in high doses, it blocks postsynaptic D2 receptors localized in limbic structures, in contrast to similar receptors in the striatum. Does not cause catalepsy and does not lead to the development of hypersensitivity of D2-dopamine receptors after repeated treatment.
At low doses, it preferentially blocks presynaptic D2/D3 receptors, causing the release of dopamine, which is responsible for its disinhibitory effects. This atypical pharmacological profile may explain the antipsychotic effect of amisulpride at high doses, resulting from blockade of postsynaptic dopamine receptors, and its effectiveness against negative symptoms at low doses, resulting from blockade of presynaptic dopamine receptors.
In addition, amisulpride causes less extrapyramidal side effects, which may be due to its predominant limbic activity.
In patients with schizophrenia with acute attacks, Solian acts on both secondary negative symptoms and affective symptoms such as depressed mood and retardation.
Pharmacokinetics
Amisulpride has two absorption peaks: one is achieved quickly, one hour after dosing, and the second is reached between 3 and 4 hours after dosing. Plasma concentrations are respectively 39 ± 3 and 54 ± 4 ng/ml, after taking 50 mg.
The volume of distribution is 5.8 l/kg. Since plasma protein binding is low (16%), interaction with other drugs is unlikely.
Absolute bioavailability is 48%. Amisulpride metabolizes weakly: (about 4%, two inactive metabolites have been identified. Amisulpride does not accumulate, and its pharmacokinetics remains unchanged after repeated doses.
The half-life (T1/2) of amisulpride is approximately 12 hours after oral dosing.
Amisulpride is excreted unchanged in the urine. Renal clearance is approximately 20 l/hour or 330 ml/min.
A carbohydrate-rich meal (containing 68% liquid) significantly reduced the AUC (area under the concentration/time curve), time to maximum concentration and maximum concentration of amisulpride, but no changes in pharmacokinetics were noted after ingestion of a fatty meal. However, the significance of these observations in daily clinical practice is unknown.
Liver failure. Due to the fact that the drug is poorly metabolized, there is no need to reduce the dose for patients with liver dysfunction.
Kidney failure. T1/2 in patients with renal failure does not change, but systemic clearance decreases by a factor of 2.5 to 3. The AUC of amisulpride in mild renal failure doubles, and in moderate failure almost tenfold (see section Dosage and Administration). Practical experience, however, is limited and there are no results with doses exceeding 50 mg.
Amisulpride is poorly dialyzable.
Limited pharmacokinetic data for elderly (over 65 years of age) patients indicate that after a single 50 mg oral dose, Cmax, T1/2 and AUC are 10-30% higher than in younger adults. There are no data on the pharmacokinetics of the drug during long-term treatment.
Special instructions
Special instructions
It is possible to develop a malignant neuroleptic syndrome, characterized by hyperthermia, muscle rigidity, dysfunction of the peripheral nervous system, and increased levels of CPK. If hyperthermia develops, especially when used in high doses, all antipsychotic drugs (including Solian) should be discontinued.
Since amisulpride is eliminated by the kidneys, in case of severe renal impairment, the dose of the drug and the treatment regimen should be adjusted. There is no experience with the use of the drug in patients with severely impaired renal function (creatinine clearance less than 10 ml/min).
Since the drug is poorly metabolized, dose reduction is not required in case of liver dysfunction.
Due to the possible decrease in the seizure threshold when using amisulpride, patients with a history of epilepsy require constant monitoring during Solian therapy.
In elderly patients, amisulpride should be used with special precautions due to the possible risk of hypotension or excessive sedation.
In Parkinson’s disease, caution should be exercised when prescribing antidopaminergic drugs and amisulpride due to the possible worsening of the condition. Amisulpride should only be used if antipsychotic therapy cannot be avoided.
Amisulpride causes a dose-dependent prolongation of the QT interval, thereby increasing the risk of developing serious ventricular arrhythmias (such as torsade de pointes). Before prescribing the drug, and, if possible, depending on the patient’s clinical condition, it is recommended to monitor factors contributing to the development of arrhythmia: bradycardia (heart rate less than 55 beats/min), hypokalemia, congenital prolongation of the QT interval.
In patients requiring long-term treatment with antipsychotics, an ECG should be performed as part of the initial assessment of the status.
Due to the lactose content in the tablets, the drug is contraindicated in congenital galactosemia, impaired absorption of glucose or galactose, or lactase deficiency.
Use for liver dysfunction: When prescribing the drug to patients with liver dysfunction, no dose reduction is required.
Use for impaired renal function: The use of the drug is contraindicated in severe renal failure (creatinine clearance less than 10 ml/min).
Effect on the ability to drive vehicles and operate machinery: Amisulpride affects the reaction rate, as a result of which the ability to engage in potentially hazardous activities may be weakened.
Active ingredient
Active ingredient
Amisulpride
Composition
Composition
1 tablet contains
active ingredient: amisulpride – 400 mg;
excipients: sodium carboxymethyl starch (sodium amylopectin glycolate) (type A), lactose monohydrate, microcrystalline cellulose, hypromellose, magnesium stearate.
Shell composition. hypromellose, microcrystalline cellulose, macrogol stearate, titanium dioxide (E 171).
Pregnancy
Pregnancy
The safety of amisulpride during pregnancy has not been established.
Therefore, the use of the drug during pregnancy is not recommended, unless the expected benefit to the mother justifies the potential risk to the fetus.
The use of amisulpride during lactation is contraindicated.
Contraindications
Contraindications
– Concomitant prolactin-dependent tumors (including pituitary prolactinoma, breast cancer).
– Pheochromocytoma.
– Severe renal failure (creatinine clearance less than 10 ml/min).
– Combined use with sultopride.
– Combined use with dopaminergic agonists (including amantadine, apomorphine, bromocriptine, cabergoline, entacapone, lisuride, pergolide, piribedil, pramipexole, quinagolide, ropinirole, selegiline), with the exception of patients with Parkinson’s disease.
– Children up to 14 years old.
– Lactation period (breastfeeding).
– Hypersensitivity to amisulpride and other components of the drug.
The drug should be used with caution when:
– Pregnancy.
– Epilepsy.
– Parkinsonism.
– Kidney failure.
– In elderly patients.
Side Effects
Side Effects
Adverse reactions (HP) are presented in accordance with the following gradations of the frequency of their development: very often (≥10%); often (≥1%, <10%); uncommon (≥0.1%, <1%); rare (≥0.01%, <0.1%); very rare, including isolated reports (<0.01%); frequency is unknown (it is not possible to determine the frequency of HP development based on available data).
Blood and lymphatic system disorders
Uncommon: leukopenia, neutropenia (see section “Special instructions”).
Rarely: agranulocytosis (see section “Special instructions”).
Immune system disorders
Uncommon: allergic reactions.
Endocrine system disorders
Often: amisulpride causes an increase in plasma concentrations of prolactin, which is reversible after discontinuation of the drug. This can lead to galactorrhea, amenorrhea, gynecomastia, breast pain and erectile dysfunction
Rare: benign pituitary tumor, such as prolactinoma. Metabolic and nutritional disorders
Common: weight gain.
Uncommon: hyperglycemia (see sections “With caution” and “Special instructions”), hypertriglyceridemia, hypercholesterolemia.
Rarely: hyponatremia, syndrome of inappropriate secretion of antidiuretic hormone.
Mental disorders
Common: insomnia, anxiety, agitation, impaired orgasm (orgasmic dysfunction).
Uncommon: confusion.
Nervous system disorders
Very common: extrapyramidal symptoms (tremor, rigidity, hypokinesia, hypersalivation, akathisia, dyskinesia). These symptoms are usually mild when taken at optimal doses and are partially reversible with the addition of anticholinergic antiparkinsonian drugs without stopping amisulpride treatment. The incidence of extrapyramidal symptoms depends on the dose. Therefore, in patients with predominantly negative symptoms taking amisulpride at a dose of 50-300 mg per day, the incidence of extrapyramidal disorders is very low. According to clinical studies, a significantly lower incidence of extrapyramidal symptoms was observed with the use of amisulpride than with the use of haloperidol.
Common: acute dystonia (spasmodic torticollis, oculogyric crisis, trismus), reversible with the addition of anticholinergic antiparkinsonian drugs without stopping treatment with amisulpride; drowsiness.
Uncommon: tardive dyskinesia, characterized by rhythmic, involuntary movements, mainly of the tongue and/or facial muscles, and usually occurs after long-term use of the drug (anticholinergic antiparkinsonian drugs in these cases are ineffective or may increase symptoms); convulsions.
Rare: neuroleptic malignant syndrome (see section “Special Instructions”), which is a potentially fatal complication.
Frequency unknown: restless legs syndrome with or without akathisia.
Visual disorders
Common: blurred vision.
Cardiac disorders
Uncommon: bradycardia.
Rarely: prolongation of the QT interval; ventricular arrhythmias, such as torsades de pointes, ventricular tachycardia, ventricular fibrillation, cardiac arrest and sudden death (see section “Special Instructions”).
Vascular disorders
Frequently: decrease in blood pressure.
Uncommon: increased blood pressure.
Rare: venous thromboembolic complications, including pulmonary embolism, sometimes fatal, and deep vein thrombosis (see section “Special Instructions”).
Respiratory, thoracic and mediastinal disorders
Uncommon: nasal congestion; aspiration pneumonia (mainly when used concomitantly with other antipsychotics and CNS depressants).
Gastrointestinal disorders
Common: constipation, nausea, vomiting, dry mouth. .
Disorders of the liver and biliary tract
Uncommon: hepatocellular lesions.
Skin and subcutaneous tissue disorders
Rarely: angioedema, urticaria.
Frequency unknown: photosensitivity.
Musculoskeletal and connective tissue disorders
Uncommon: osteopenia, osteoporosis.
Renal and urinary tract disorders
Uncommon: urinary retention.
Injuries, complications and complications caused by manipulations
Not known: falls (sometimes resulting in fractures) as a consequence of adverse reactions associated with possible imbalance.
Pregnancy, postpartum and perinatal conditions
Frequency unknown: withdrawal syndrome in newborns (see section “Use during pregnancy and breastfeeding”).
Laboratory abnormalities
Uncommon: increased activity of liver enzymes in the blood, mainly transaminases.
Interaction
Interaction
Combinations that are contraindicated: With dopaminergic agonists (including amantadine, apomorphine, bromocriptine, cabergoline, entacapone, lisuride, pergolide, piribedil, pramipexole, quinagolide, ropinirole, selegiline), with the exception of patients with Parkinson’s disease. Dopaminergic agonists and antipsychotics exhibit mutual antagonism.
For extrapyramidal syndrome caused by antipsychotics, anticholinergic drugs should be used instead of dopaminergic agonists. When Solian is used simultaneously with sultopride, the risk of ventricular arrhythmias, especially atrial fibrillation, increases.
Combinations that are not recommended: With drugs that can cause pirouette-type arrhythmias: class Ia (including quinidine, hydroquinidine, disopyramide) and class III antiarrhythmic drugs (including amiodarone, sotalol, dofetilide, ibutilide), some neuroleptics (including thioridazine, chlorpromazine, levomepromazine, trifluoperazine, cyamemazine, sulpiride, tiapride, pimozide, haloperidol, droperidol) and other drugs (including bepridil, cisapride, difemanil, IV erythromycin, mizolastine, IV vincamine, halofantrine, sparfloxacin, gatifloxacin, moxifloxacin, pentamidine, iv spiramycin).
The risk of ventricular arrhythmias increases, especially the development of pirouette-type arrhythmias. If a combination of drugs cannot be avoided, monitor the QT interval and begin ECG monitoring before prescribing. Ethanol enhances the sedative effects of neuroleptics. The consumption of alcoholic beverages and the use of medications containing alcohol should be avoided. The mutual antagonism of the effects of levodopa and antipsychotics should be taken into account when prescribing these drugs. In patients with Parkinson’s disease, it is recommended to use the minimum effective doses of both drugs.
Combinations requiring special caution: With drugs that cause bradycardia (including beta-blockers / except sotalol / calcium channel blockers that cause bradycardia – diltiazem and verapamil), clonidine, guanfacine, digitalis preparations, cholinesterase inhibitors (including donepezil, rivastigmine, tacrine, ambenonium, galantamine, pyridostigmine, neostigmine).
With drugs that can cause hypokalemia (including potassium-sparing diuretics, laxatives, IV amphotericin B, glucocorticoids, tetracosactides). With the above combinations of drugs, the risk of ventricular arrhythmias remains, especially the development of pirouette-type arrhythmias.
Combinations that should be taken into account: With antihypertensive drugs and beta-blockers for heart failure (including bisoprolol, carvedilol, metoprolol) has a vasodilatory effect, increasing the risk of orthostatic hypotension (additive effect).
With morphine derivatives (including analgesics, antitussives), barbiturates, benzodiazepines and other anxiolytics, hypnotics, sedative antidepressants (including amitriptyline, doxepin, mianserin, mirtazapine, trimipramine), sedative antihistamines, centrally acting antihypertensives, neuroleptics and other drugs (including baclofen, thalidomide, pizotifen) leads to a pronounced increase in the inhibitory effect on the central nervous system (concentration decreases and poses a danger to vehicle drivers and machine operators).
Overdose
Overdose
Symptoms: Experience with amisulpride overdose is very limited. A significant increase in the known pharmacological effects of the drug has been reported, namely the development of drowsiness, sedation, coma, arterial hypotension and extrapyramidal symptoms.
It should be borne in mind that overdose phenomena can occur in cases of erroneous administration of additional doses of the drug or simultaneous use of other drugs.
Treatment: There is no specific antidote for amisulpride.
In case of overdose, the basic vital functions of the body should be monitored and maintained until the patient completely recovers from the overdose. In case of overdose, ECG monitoring is mandatory, because there is a risk of prolongation of the QT interval and the development of life-threatening arrhythmias (see “Side effects”).
If severe extrapyramidal symptoms occur, anticholinergic drugs should be used.
Because Since the elimination of amisulpride by hemodialysis is insignificant, the use of hemodialysis for its removal in case of overdose is inappropriate.
Storage conditions
Storage conditions
In a dry place, at a temperature not exceeding 25 °C
Shelf life
Shelf life
3 years
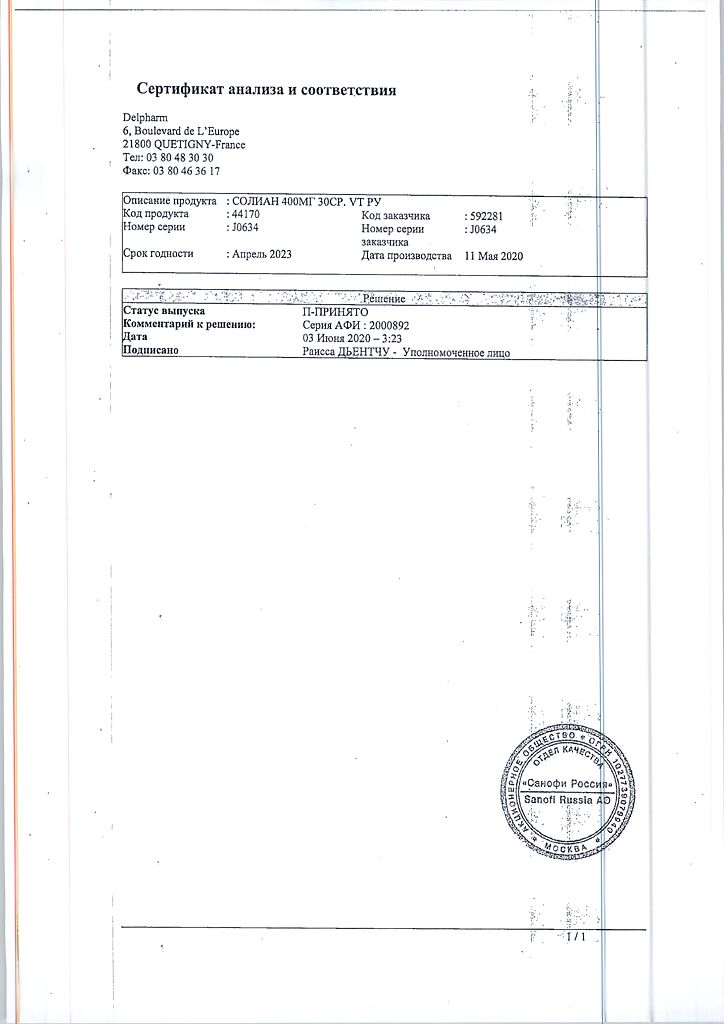
Manufacturer
Manufacturer
Delpharm Dijon, France
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a dry place, at a temperature not exceeding 25 °C |
| Manufacturer | Delpharm Dijon, France |
| Medication form | pills |
| Brand | Delpharm Dijon |
Related products
Buy Solian, 400 mg 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.