No products in the cart.
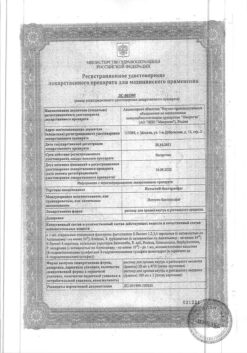
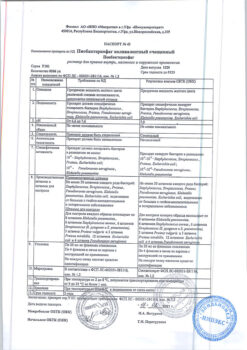
Simponi 50 mg/0.5 ml syringe pen
€1.00
Out of stock
(E-mail when Stock is available)
Description
Golimumab is a human IgG1k monoclonal antibody produced by a mouse hybridoma cell line derived from recombinant DNA technology.
The mechanism of action
Golimumab is a human monoclonal antibody that forms high-affinity stable antigen-antibody complexes with both soluble and transmembrane bioactive forms of human tumor necrosis factor alpha (TNF-α), preventing TNF-α binding to its receptors. Increased expression of TNF-α is seen in chronic inflammatory diseases such as rheumatoid arthritis (RA), as well as in snopdyloarthritis, including psoriatic arthritis (PsA) and axial spondyloarthritis (ankylosing spondylitis (AS) and neurogenic axial spondyloarthritis). TNF-α plays an important role in the development of inflammation and joint destruction that are characteristic of these diseases.
Pharmacodynamic properties
The binding of human TNF-α by golimumab results in the inhibition (or suppression) of the expression of adhesion molecules, including E-selectin, vascular cell adhesion molecules (VCAM-1) and intercellular adhesion molecules (ICAM-1), on endothelial cell surfaces. In addition, golimumab inhibits TNF-α-induced secretion of interleukin IL-6, IL-8 and granulocyte-macrophage colony-stimulating factor (GM-CSF) by human endothelial cells. In vivo golimumab treatment significantly delayed the onset of clinical symptoms in mice with induced arthritis and significantly suppressed the activity of pathological processes in the joints.
Simponi® had an effective modulatory effect on the levels of inflammatory markers and bone metabolism parameters in patients with various diseases. In particular, there was a decrease in the levels of C-reactive protein (CRP) compared to the placebo group.
The drug Simponi® caused significant reductions in serum levels of IL-6, ICAM-1, matrix metalloproteinase-3 (MMP-3) and vascular endothelial growth factor (VEGF) compared to controls. In addition, there were decreases in TNF-α levels in patients with RA and AS and in IL-8 concentrations in patients with PsA. These changes were observed at the first examination (4th week) after the first dose of Simponi® and persisted till the 24th week.
The use of Simponi® with or without methotrexate (MT) resulted in significant changes in serum levels of several markers of bone metabolism (increased levels of osteocalcin and N-terminal procollagen type I propeptide and decreased levels of deoxypyridinoline) at week 4. These biomarker changes are consistent with an improvement in the clinical course of the disease in the form of reduced inflammation, increased bone growth and suppression of bone resorption.
Indications
Indications
Rheumatoid arthritis (in combination with methotrexate):
Psoriatic arthritis (as monotherapy or in combination with methotrexate):
Ankylosing spondylitis: for the treatment of severe, active ankylosing spondylitis in adult patients in whom the response to standard therapy has been inadequate.
Active ingredient
Active ingredient
Composition
Composition
The 0.5 ml solution contains:
the active substance:
golimumab 50 mg;
excipients:
sorbitol 20.5 mg,
histidine 0.44 mg,
polysorbate-80 0.075 mg,
water for injection 0.5 ml.
How to take, the dosage
How to take, the dosage
Treatment with Simponi should be initiated and administered under the supervision of qualified physicians experienced in the diagnosis and treatment of rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis.
After training in injection technique, patients may inject Simponi themselves if the physician considers it possible, and the physician should continue to monitor the patient.
Adults (â¥18 years)
Rheumatoid arthritis
Simponi 50 mg is given by injection monthly on the same day of the month. Simponi is used in combination with methotrexate.
Psoriatic arthritis
Simponi 50 mg is administered p/monthly on the same day of the month.
Ankylosing spondylitis
The drug Simponi 50 mg is administered by the oral route monthly on the same day of the month.
The current data shows the development of a clinical response between 12-14 weeks of therapy (3-4 injections). If there is no effect during this period of time, the appropriateness of further use of the drug should be evaluated.
In patients with a body weight greater than 100 kg, in the absence of an adequate response on 3-4 injections, an increase in the dose of golimumab to 100 mg monthly may be considered, taking into account the possible increased risk of serious adverse reactions associated with increasing the dose. If there is no effect of golimumab therapy at a dose of 100 mg for 12-14 weeks, the feasibility of further use should be reassessed.
Dose adjustment in elderly patients (⥠65 years) is not required.
The effect of Simponi drug has not been studied in patients with impaired renal and/or hepatic function. No dosing recommendations can be given.
Missing an injection
If the injection is not given on the scheduled date, the next injection of the drug should be given as soon as possible. If the patient self-administers Simponi, the dose should not be increased to compensate for the missed injection.
If less than 2 weeks have elapsed since the scheduled injection date, the next injection should be given at the same dose as usual and the therapy should be continued according to the previous regimen.
If more than 2 weeks have elapsed since the scheduled injection date, the next injection should be given at the same dose as usual and then the therapy should be continued according to the new regimen (the next injection is again given one month after this injection).
Interaction
Interaction
No interaction studies have been performed.
Combination therapy with Simponi and anakinra or abatacept is not recommended.
Live vaccines should not be administered during treatment with Simponi.
Although co-administration of methotrexate results in increased minimum Css of Simponi in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis, the data suggest that no dose adjustment of Simponi or methotrexate is necessary.
Special Instructions
Special Instructions
Infections
Patients should be closely monitored for infections before the prescription of Simponi, during therapy and for 5 months thereafter. If severe infections or sepsis develop, therapy should be discontinued.
The drug Simponi should not be administered to patients with clinically significant active infection. Caution should be exercised when using Simponi in patients with a history of chronic infection or recurrent infection. Patients are advised to avoid exposure to potential risk factors for infection if possible.
Patients treated with TNF inhibitors are at greater risk of developing an infection. There have been reports of bacterial (including sepsis and pneumonia), mycobacterial (tuberculosis), invasive fungal and opportunistic infections, including death, in patients receiving TNF inhibitors, including Simponi. In some cases serious infections developed in patients receiving concomitant therapy with immunosuppressants, which, like the disease itself, predisposes to the development of infections. Patients with new cases of infectious diseases should be carefully examined. The use of Simponi should be discontinued in cases of severe infections or sepsis and an appropriate antibacterial or antifungal therapy should be prescribed until the infectious process is controlled.
People who have lived in or visited regions endemic for invasive mycoses such as histoplasmosis, coccidiomycosis, or blastomycosis should carefully weigh the possible benefits and risks of treatment with Simponi before initiating treatment with Simponi.
Tuberculosis
Tuberculosis has been reported in patients treated with Cimponi. In most cases these were extrapulmonary or disseminated forms of TB.
Before treatment with Simponi it is necessary to assess risk factors for tuberculosis (including close contact with patients with active tuberculosis) and to rule out the presence of latent or active tuberculosis. Treatment of latent tuberculosis should be carried out before the use of Simponi. Therapy with Simponi is contraindicated in case of active tuberculosis.
In patients with a history of latent tuberculosis or active tuberculosis for which adequate treatment cannot be confirmed, antituberculosis therapy should be given before starting Simponi.
Tests for latent tuberculosis may be falsely negative, especially in patients with immunodeficiency or severe disease. Before prescribing Cimponi, treatment of latent tuberculosis should be considered if patients have appropriate risk factors, despite a negative latent tuberculosis test result. The decision to prescribe antituberculosis therapy in such patients should be made only after consultation with a phthisiatrician, comparing the risk of latent tuberculosis with the risk of antituberculosis therapy.
In patients receiving Simponi, signs and symptoms of active tuberculosis should be monitored during and after treatment, including in patients who test negative for latent tuberculosis.
All patients should be informed about symptoms suspected of TB (prolonged cough, weight loss, subfebrile fever) and the need to seek medical attention if they occur. If tuberculosis infection develops during therapy with Simponi the drug should be discontinued and anti-tuberculosis therapy should be prescribed
Hepatitis B virus reactivation
. As with treatment with other immunosuppressants, therapy with TNFα inhibitors was accompanied by reactivation of hepatitis B virus in chronic carriers of the virus (when positive for surface antigen test), including with development of fatal outcome. All patients should be examined before the start of therapy to exclude viral hepatitis B. Chronic hepatitis B carriers should be monitored closely prior to initiation of therapy, during treatment and for several months after discontinuation of therapy with Cimponi.
There are no data available on the efficacy of combined use of antiviral therapy and TNFα inhibitors in patients who are chronic carriers.
In case of reactivation of viral infection, treatment with Simponi should be discontinued and appropriate antiviral therapy should be prescribed.
Malignant tumors
The possible role of TNFα inhibitor therapy in the development of malignancies has not been established, but based on current data, the risk of lymphoma, leukemia, and other malignancies on anti-NFα therapy cannot be excluded. Caution should be exercised when prescribing TNF inhibitors to patients with a history of malignancies or when continuing therapy if malignancy develops.
Malignant tumors in children
Postmarketing studies have reported cases of malignancy, some fatal, in children, adolescents, and young adults (under age 22) who received TNF inhibitors (initiation of therapy at age â¤18 years). Approximately half of the cases reported were lymphomas. Other cases represented a number of different malignancies, including malignancies not usually seen in children and adolescents. Most patients received concomitant therapy with immunosuppressants such as methotrexate, azathioprine, or 6-mercaptopurine. The role of TNF inhibitors in the development of malignancies in children and adolescents remains unclear.
Lymphoma
In controlled clinical trials of treatment with all TNF inhibitors, including Simponi, cases of lymphoma were reported more frequently in patients treated with TNF inhibitors than in controls. In Phase 2 and 3 clinical trials of Simponi, the incidence of lymphoma in patients treated with Simponi was higher than expected in the general population. In patients with rheumatoid arthritis and other chronic inflammatory diseases, especially in patients with high disease activity and/or patients undergoing long-term immunosuppressant therapy, the risk of lymphoma is higher (several times higher) than in the general population, even without treatment with TNF inhibitors.
Leukemia
In the postmarketing use of TNF inhibitors to treat rheumatoid arthritis and other diseases, cases of acute and chronic leukemia have been reported. Even in the absence of TNF inhibitor therapy, patients with rheumatoid arthritis may have an increased risk (approximately 2-fold) of developing leukemia compared to the general population.
Other malignancies
In controlled clinical trials of Simponi’s phase II and III drugs in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis, the rates of other malignancies (excluding nonmelanoma skin cancer) were similar in the Simponi group and the control group.
In a clinical study evaluating the use of Simponi in patients with severe persistent asthma, malignancies were more common in patients treated with Simponi than in the control group. The significance of this finding has not been established.
In a clinical trial with another TNFα inhibitor, infliximab, a higher incidence of lung, head and neck tumors was reported in patients with moderate to severe COPD in the TNF inhibitor group compared to controls. Therefore, caution should be exercised when prescribing TNF inhibitors to patients with COPD as well as to high-risk patients such as chronic smokers.
Congestive heart failure
In treatment with TNF inhibitors, there have been cases of an increase or development of congestive heart failure, including during therapy with Simponi. In clinical trials with the use of other TNF inhibitors, progression of heart failure and increased mortality due to CHF were observed. The effect of Simponi has not been studied in patients with congestive heart failure. Simponi should be used with caution in patients with mild heart failure (NYHA class I-II). Patients should be monitored and in case of new or worsening of existing signs of heart failure, therapy with Simponi should be discontinued.
Neurological disorders
The use of TNF inhibitors, including Simponi, in rare cases was accompanied by the appearance or increase in clinical and/or radiological signs of demyelinating diseases of the CNS (including multiple sclerosis) and the peripheral nervous system. In patients with existing or newly emerging demyelinating diseases, the benefits and risks of treatment with TNF inhibitors should be carefully weighed before prescribing Simponi. If such diseases develop, therapy with Simponi should be discontinued.
Surgical treatment
The data on the safety of Simponi in patients receiving surgical treatment, including arthroplasty, are limited. A long T1/2 must be considered when planning surgeries. When performing surgery in patients treated with Simponi, close monitoring of infections is required and timely therapy if they occur.
Immunosuppression
There is potential for TNF inhibitors, including Simponi®, to affect immunity against infections and tumors due to blockade of inflammation and modulation of cellular response mediated through TNFα.
Autoimmune processes
A relative TNFα deficiency against the background of TNF inhibitor therapy may lead to the development of autoimmune processes. When clinical symptoms of lupus-like syndrome occur and when antibodies to double-stranded DNA test positive, therapy with Simponi should be discontinued.
The concomitant use of Simponi and anakinra
The concomitant use of anakinra and another TNF inhibitor, etanercept, in clinical trials has resulted in serious infections and neutropenia and no additional clinical benefit. Because of the nature of adverse reactions seen with this combination therapy, similar types of toxicity may occur with combination therapy with anakinra and other TNF inhibitors. Therefore, combined use of Simponi® and anakinra is not recommended.
The combined use of Simponi and abatacept
In clinical trials, the combined use of TNF inhibitors and abatacept has been associated with an increased risk of infections, including serious infections, compared to the use of TNF inhibitors alone, without enhancing the clinical effect. Because of the nature of adverse reactions seen with combination therapy with TNF inhibitors and abatacept, the combination of Simponi and abatacept is not recommended.
Changing biologic basal anti-inflammatory drugs
When transferring from one biologic drug to another, patients should continue to be monitored for signs of infection.
Hematologic reactions
In a post-marketing study, there have been reports of pancytopenia, leukopenia, neutropenia and thrombocytopenia in patients receiving TNF inhibitors, including Simponi. Caution should be exercised when treating patients with cytopenia or a history of serious cytopenias with Simponi.
Patients with the development of signs of hematological disorders (persistent fever, bruising, bleeding, pallor) should be immediately examined. In case of marked hematological disorders, Simponi therapy should be discontinued.
Allergic reactions
The post-marketing study of Simponi described serious systemic hypersensitivity reactions, including anaphylactic reactions. Some cases have been described after the first administration of the drug. In cases of anaphylactic reactions or other serious allergic reactions, the use of Simponi should be discontinued and appropriate therapy administered.
Vaccination
Patients receiving Simponi may receive a concomitant vaccination, but not live vaccines. There are no data on response to vaccination, risk of infection, or possibility of transmission with live vaccines in patients receiving Simponi. In patients with psoriatic arthritis who received Simponi in one phase 3 study, an effective B-cell immune response to the pneumococcal polysaccharide vaccine was observed. A comparable number of patients with psoriatic arthritis who received and did not receive Simponi showed at least a twofold increase in antibody titers. The percentage of patients who responded to the pneumococcal vaccine was lower in the Simponi group and in the control group of patients receiving methotrexate than in patients not receiving methotrexate. Overall, the data suggest that Simponi did not suppress the humoral immune response to this vaccine.
Latex sensitivity
The needle protection cap on the prefilled syringe is made of dry natural rubber containing latex, which can cause allergic reactions in latex-sensitive patients.
Patients in the elderly
Patients. In phase III studies in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis, the incidence of adverse events, serious adverse events and serious infections during treatment with Simponi did not differ between patients aged 65 years or older (n=155) and younger patients. In general, older patients had a higher incidence of infections, so caution should be exercised when treating older patients.
Hepatic and renal impairment
Special studies of Simponi in patients with impaired renal and hepatic function have not been performed. Caution should be exercised when treating patients with hepatic impairment.
The clinical effectiveness in the treatment of rheumatoid arthritis
The efficacy and safety of Simponi was studied in three multicenter, randomized, double-blind, placebo-controlled trials in more than 1,500 patients aged â¥18 years with moderate-to-severe to severe active rheumatoid arthritis diagnosed according to American College of Rheumatologists (ACR) criteria at least 3 months before screening. Simponi was administered subcutaneously at doses of 50 mg or 100 mg (with or without MT) every 4 weeks. The duration of the placebo-controlled phase was 24 weeks.
The overall clinical efficacy of Simponi at doses of 50 mg and 100 mg was not significantly different.
In all phase 3 studies, the proportion of patients responding adequately to treatment after 14 and 24 weeks was higher in the Simponi groups than in the control groups. Response was observed 4 weeks after initiation of Simponi treatment (when results were first evaluated) and persisted for 24 weeks.
The treatment with Cimponi compared to placebo showed clinically and statistically significant improvement in quality of life. There was a statistically significant improvement in ability to work and a decrease in fatigue.
Clinical efficacy in the treatment of psoriatic arthritis
The safety and efficacy of Simponi was studied in a multicenter, randomized, double-blind, placebo-controlled study in 405 adult patients with active psoriatic arthritis who had not responded to NSAID or basic anti-inflammatory medication therapy. In this study, the time from the diagnosis of psoriatic arthritis was at least 6 months before inclusion in the study, with a plaque skin lesion diameter of at least 2 cm. Patients with various subtypes of psoriatic arthritis, including polyarthritis without rheumatoid nodules (43%), asymmetric peripheral arthritis (30%), arthritis of the distal interphalangeal joints (15%), spondylitis with peripheral arthritis (11%) and mutilitating arthritis (1%) were included in the study. Previous therapy with a TNF antagonist was an exclusion criterion. Simponi was administered p/c in doses of 50 mg or 100 mg every 4 weeks with or without methotrexate. Randomized patients received placebo (n=113), Simponi 50 mg (n=146), and Simponi 100 mg (n=146). The primary endpoint was the proportion of patients achieving 20% improvement according to ACR 20 criteria after 14 weeks. Treatment results were compared with placebo at 24 weeks.
The overall clinical efficacy of Simponi at doses of 50 mg and 100 mg was not significantly different.
Emprovement in the main parameters characterizing disease activity was already noted at the first examination (4 weeks) after the start of treatment and was maintained for 24 weeks. The response rate after 14 weeks was similar in patients with different subtypes of psoriatic arthritis, including polyarthritis without rheumatoid nodules, asymmetric peripheral arthritis, arthritis of the distal interphalangeal joints and spondylitis with peripheral arthritis. The number of patients with mutilating arthritis was insufficient to assess efficacy. The response rate to Simponi treatment was comparable in patients receiving and not receiving methotrexate.
Treatment with Simponi showed improvement in psoriatic arthritis activity, including the number of swollen joints, number of painful joints, dactylitis, and enthesitis. In addition, patients treated with Simponi showed significant improvement in psoriasis of the skin and nails.
The treatment with Simponi resulted in a significant improvement in physical function as well as quality of life. Ability to work significantly increased, and time spent with the patient by caregivers or treatment providers decreased.
The clinical effectiveness in the treatment of ankylosing spondylitis
The safety and efficacy of Simponi was studied in a multicenter, randomized, placebo-controlled trial in 356 adult patients with active ankylosing spondylitis. The study included patients who had persistent signs of active ankylosing spondylitis despite treatment with NSAIDs or basal anti-inflammatory drugs. They had not previously received TNF antagonists. Patients with complete ankylosis of the spine were excluded from the study. Simponi was administered p/c every 4 weeks. Randomized patients received placebo (n=78), Simponi 50 mg (n=138), and Simponi 100 mg (n=140). The primary endpoint was the proportion of patients achieving ASAS 20 improvement after 14 weeks. Efficacy was compared with placebo at 24 weeks.
The overall clinical efficacy of Simponi at doses of 50 mg and 100 mg was not significantly different.
In comparison to placebo, treatment with Simponi resulted in a significant reduction of symptoms after 14 and 24 weeks. Improvement in the key indicators of ankylosing spondylitis activity was noted at the first evaluation of treatment (4 weeks) and was sustained for 24 weeks.
Treatment with Simponi caused a significant increase in physical function, which was assessed at 14 and 24 weeks. In patients treated with Simponi®, the improvement in physical function was maintained at 24 weeks. Quality of life was also significantly improved after 14 and 24 weeks. In addition, significant improvements in sleep and work ability were found.
Immunogenicity
Antibodies to golimumab were detected in 5% (105/2115) of patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis who received Simponi for 52 weeks in phase 3 studies. The frequency of antibody formation was comparable in patients with different rheumatic diseases. Patients who received concomitant methotrexate therapy had lower antibody rates than patients who received Simponi without methotrexate (3% (41/1262) and 8% (64/853), respectively).
The presence of antibodies to golimumab may increase the risk of injection site reactions. The low incidence of antibodies to golimumab does not allow definite judgments about the relationship between immunogenicity and clinical efficacy or safety.
Because the immunogenicity assay is product-specific and specific to each individual reagent kit, a comparison of antibody levels to different products is not valid.
Pediatric use
There have been no specific studies of Simponi in children. The drug is contraindicated in children and adolescents under 18 years of age, because the safety and effectiveness in this patient population has not been studied.
Impact on ability to drive vehicles and other mechanisms
The drug Simponi may have slight effect on the ability to drive vehicles and operate machinery due to possible development of adverse reactions from the nervous system and eyes.
Contraindications
Contraindications
Side effects
Side effects
Infections of the upper respiratory tract were the most frequently reported adverse effects in controlled phase III studies (at up to 16 weeks, the incidence in golimumab therapy groups was 7.2% compared to 5.8% in control groups). Serious adverse reactions included severe infections (including sepsis, pneumonia, tuberculosis, invasive fungal and opportunistic infections), demyelinating disease, lymphoma, reactivation of viral hepatitis B, chronic heart failure, autoimmune disease (lupus-like syndrome) and hematological disorders.
Simponi safety data were obtained in phase 2 and 3 clinical trials in 2,578 patients, including 1,600 patients with rheumatoid arthritis, 394 patients with psoriatic arthritis, 353 patients with ankylosing spondylitis and 231 patients with severe persistent asthma, and in post-registration use.
The adverse reactions that have been observed in clinical trials of Simponi are listed in the table. They are categorized by systemic organ class and frequency of occurrence based on the following criteria: very common (>10%), common (>1% and < 10%); infrequent (>0.1% and <1%); rare (>0.01% and <0.1%); very rare (less than 0.01%, including individual cases), unknown (cannot be estimated based on available data).
Table. Adverse reactions.
IncidenceInfectious and parasitic diseasesVery commonInfections of the upper respiratory tract (rhinitis, nasopharyngitis, pharyngitis, laryngitis)FrequentBacterial infections (phlegmon), viral infections (influenza and herpes), Bronchitis, sinusitis, superficial fungal infections InfrequentSeptic shock, sepsis, tuberculosis, lower respiratory tract infections (pneumonia), opportunistic infections (invasive fungal infections (histoplasmosis, coccidioidomycosis, pneumocystis), bacterial, atypical mycobacterial and protozoal), pyelonephritis, abscess, bacterial arthritis, infectious bursitisRarelyReactivation of hepatitis BDoblastic, Malignant tumors and unspecified neoplasmsInfrequentTumors (skin cancer, squamous cell carcinoma, and myelocytic nevus)RarelyLymphoma, leukemiaHematopoietic system:FrequentAnemiaFrequentLeukopenia, thrombocytopeniaRarelyPancytopeniaNot knownAplastic anemia* Immune system sideFrequentAllergic reactions (bronchospasm, hypersensitivity, urticaria), RarelySystemic allergic reactions (anaphylactic reactions), systemic vasculitis, sarcoidosisEndocrine system InfrequentThyroid disorders (hypothyroiditis, Mental disordersFrequentDepression, insomniaNervous system disordersFrequentDizziness, paresthesia, headacheFrequentDemyelinating diseases (central and peripheral forms), Visual disordersInfrequent Visual disturbances (clouding), conjunctivitis, allergic reactions (redness, irritation)Cardiovascular system:FrequentArterial hypertensionInfrequentSerious heart failure (newly detected or worsening of existing), arrhythmias, angina pectoris, thrombosis (including deep vein and artery thrombosis), Raynaud’s disease, hyperemiaInfrequentBronchial asthma and associated symptoms (shortness of breath, overactive bronchi)RarelyInterstitial lung diseaseDigestive system side:FrequentEstipation, dyspepsia, GI pain, nauseaInfrequentInflammatory GI disease (gastritis, colitis), reflux, stomatitisFrequentLiver and biliary tract activity Increased ALT, ASTFrequentCholletitiasis, liver dysfunctionFrequentSkin and subcutaneous tissue sideFrequentAlopecia, Dermatitis, itching, rash InfrequentPsoriasis (first detected or worsening of existing disease, palpebral, pustular), urticaria, systemic vasculitisMuscular system and connective tissueRarelySolenoid-like syndromeSystem urinary tract disorders:InfrequentBladder diseaseRarelyKidney diseaseCurrentlyGenital and mammary gland involvementFrequentMammary gland disease, menstrual disordersGeneral disorders:FrequentHyperthermia, asthenia, chest discomfortGeneral reactions:FrequentErythema, urticaria, thickening, pain, bruising, itching, irritation, paresthesia at injection site, slow healing at injection siteInjuries, poisoning, injection-related complicationsInfrequentBone fractures*Were seen with other TNF inhibitors, but not observed in clinical trials of golimumab
Infections
The most common adverse reaction reported in phase 3 combination studies over 16 weeks in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis was upper respiratory infection. It occurred in 7.2% of patients taking Simponi (per 100 patient-years: 26.3; 95% CI: 22.1, 31.2) and 5.8% of patients in the control group (per 100 patient-years: 22.9; 95% CI: 0.17, 0.31). At 3-year follow-up (median), the event rate per 100 patient-years for upper respiratory tract infections was 17.4 (95% CI: 16.4, 18.6 in the Simponi group).
In controlled phase 3 studies over 16 weeks in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis, infections were seen in 28.3% of patients treated with Simponi (incidence per 100 patient-years: 128; 95% CI: 118.3, 138.2) and 24.7% of control group patients (incidence per 100 patient-years: 116.6; 95% CI: 101.8, 132.9). At 3-year follow-up (median), the event rate per 100 patient-years (95% CI) of infections was 96.0 (93.5, 98.6) in the Simponi drug group.
In controlled phase 3 studies over 16 weeks in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis, serious infections were seen in 1.4% of patients treated with Simponi (incidence per 100 patient-years: 7.4 in the golimumab 100 mg group; 95% CI: 4.6, 11.1; 3.3 in the golimumab 50 mg group; 95% CI: 1.3, 6.9), and 1.3% of control group patients (incidence per 100 patient-years: 4.2; 95% CI: 1.8, 8.2). Serious infections observed with Simponi treatment included: tuberculosis, bacterial infections, including sepsis, pneumonia, invasive fungal and other opportunistic infections. Some cases were fatal. At 3-year follow-up (median), the incidence of serious infections was higher in the golimumab 100 mg group compared with the golimumab 50 mg group and was 5.1 (4.4, 5.9) and 3.0 (2.4, 3.8) serious infections per 100 patient-years (95% CI), respectively, in phase 2 and phase 3 clinical trials.
Malignant tumors
Lymphoma. The incidence of lymphoma in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis who received Simponi in controlled phase 2 and 3 clinical trials and over 3 years of follow-up was higher than the expected incidence in the general population. In controlled and uncontrolled clinical trials at a median follow-up of 3 years, the incidence of lymphoma was higher in the golimumab 100 mg group (6 patients) compared to the golimumab 50 mg group (1 patient) and placebo group and was 0.04 (0.00, 0.24), 0.18 (0.06, 0.38) and 0.00 (0.00, 0.84) per 100 patient-years (95% CI), respectively. Most cases were reported in a study involving patients transferred from other TNF inhibitors who had a longer duration of disease and refractoriness of prior therapy.
Other malignancies. In controlled phase 2 and 3 clinical trials in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis and at approximately 3-year follow-up, the incidence of other malignancies (excluding nonmelanoma skin cancer) was comparable in the Simponi drug group and the control group.
Nemelanoma skin cancer was diagnosed in 33 patients during the 3-year follow-up (5 in the placebo group, 10 in the golimumab 50 mg group, and 18 in the golimumab 100 mg group) with an event rate per 100 patient-years of 0.49 (95% CI: 0.33, 0.71) in the golimumab groups (pooled data) and 1.40 (95% CI: 0.46, 3.28) in the placebo group.
Other tumors (excluding lymphoma and nonmelanoma skin cancer) were diagnosed in 34 patients during the 3-year follow-up (2 in the placebo group, 18 in the golimumab 50 mg group and 14 in the golimumab 100 mg group) with an event rate per 100 patient-years of 0.56 (95% CI: 0.38, 0.79) in the golimumab groups (pooled data) and 0.56 (95% CI: 0.07, 2.02) in the placebo group.
Golimumab was administered p/k at a higher dose (150%) than recommended for rheumatic indications at week 0, followed by golimumab injections of 200 mg, 100 mg, and 50 mg every 4 weeks until week 52. There were 8 tumor cases diagnosed in the golimumab group (n=230) and no cases in the placebo group (n=79): 1 patient with lymphoma, 2 patients with nonmelanoma skin cancer, and 5 other tumors.
For the placebo-controlled portion of the study, the event rate for all tumors per 100 patient-years was 3.19 (95% CI: 1.38, 6.28) in the golimumab group, including: lymphoma 0.40 (0.01, 2.20), nonmelanoma skin cancer 0.79 (0.10, 2.86) and 1.99 (0.64, 4.63) for other tumors. In the placebo group, the event rate was 0.00 (0.00, 2.94), respectively.
The significance of this finding in the asthma patient population has not been established.
The potential role of TNF antagonists in the development of malignancies is not known.
Neurologic disorders
In controlled phase 2 and 3 clinical trials in patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis with a median follow-up of 3 years, a higher incidence of demyelinating disease was observed in the golimumab 100 mg group compared with the golimumab 50 mg group.
Elevated liver enzyme activity
In controlled phase 3 studies, a mild increase in ALT activity (>1 and <3-fold of GHN) was observed over 16 weeks in a comparable percentage of patients with rheumatoid arthritis and psoriatic arthritis in the Simponi® drug group and the control group (22.1-27.4% of patients); in a study of patients with ankylosing spondylitis, the incidence of moderate ALT elevation was higher in the Simponi® drug group (25.6%) than in the control group (3.9%). At 3-year follow-up, the incidence of mild ALT elevation in patients with rheumatoid arthritis and psoriatic arthritis was comparable in the Simponi group and the control group. In a study in patients with ankylosing spondylitis, the incidence of mild elevation of ALT activity was higher in the Simponi group than in the control group.
In a 16-week study in patients with rheumatoid arthritis and ankylosing spondylitis, increases in ALT activity â¥5 times the upper limit of normal were infrequent. The frequency of ALT elevation in the Simponi drug group was higher (0.4-0.9%) than in the control group (0.0%). This trend was not observed in patients with psoriatic arthritis. At physician follow-up for 3 years, the incidence of an ALT increase â¥5 times of VGN was comparable in the Simponi drug group and the control group in phase 3 studies in patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. In most cases, this increase was asymptomatic and decreased/decreased after discontinuation of golimumab therapy or correction of concomitant treatment.
In phase 2 and 3 clinical trials of patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis, 1 patient with prior liver dysfunction developed noninfectious hepatitis with jaundice, ending in death. The role of golimumab as a factor potentially provoking or aggravating the manifestations of the disease cannot be completely excluded.
Injection site reactions
In controlled phase 3 studies over 16 weeks in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis, injection site reactions were observed in 5.8% of patients treated with Simponi and 2.2% of control group patients. The presence of antibodies to golimumab may increase the risk of injection site reactions. Most reactions at the injection site were mild to moderate. Erythema at the injection site was the most common.
In controlled phase 2 and 3 studies in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis and severe persistent asthma, no anaphylactic reactions were reported when treated with Simponi.
Antinuclear antibodies (ANA)/ double-stranded DNA (dsDNA) antibodies
The use of TNF blockers has been associated with the formation of autoantibodies and rarely the development of lupus-like syndrome.
In phase 3 studies in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis, 4.0% of patients treated with Simponi and 2.6% of control group patients were again positive for ANA (titers 1:160 or higher) at 1-year follow-up compared with baseline data obtained before study inclusion. At 1-year follow-up, the formation of dsDNA antibodies in patients with baseline negative tests for dsDNA antibodies was rare.
Overdose
Overdose
Single intravenous administration at a dose up to 10 mg/kg in a clinical study was not associated with dose-limiting toxicity.
Treatment: In case of overdose in a patient it is recommended to control the symptoms of side effects and immediately prescribe symptomatic treatment.
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In the dark place at 2-8 °C (do not freeze) |
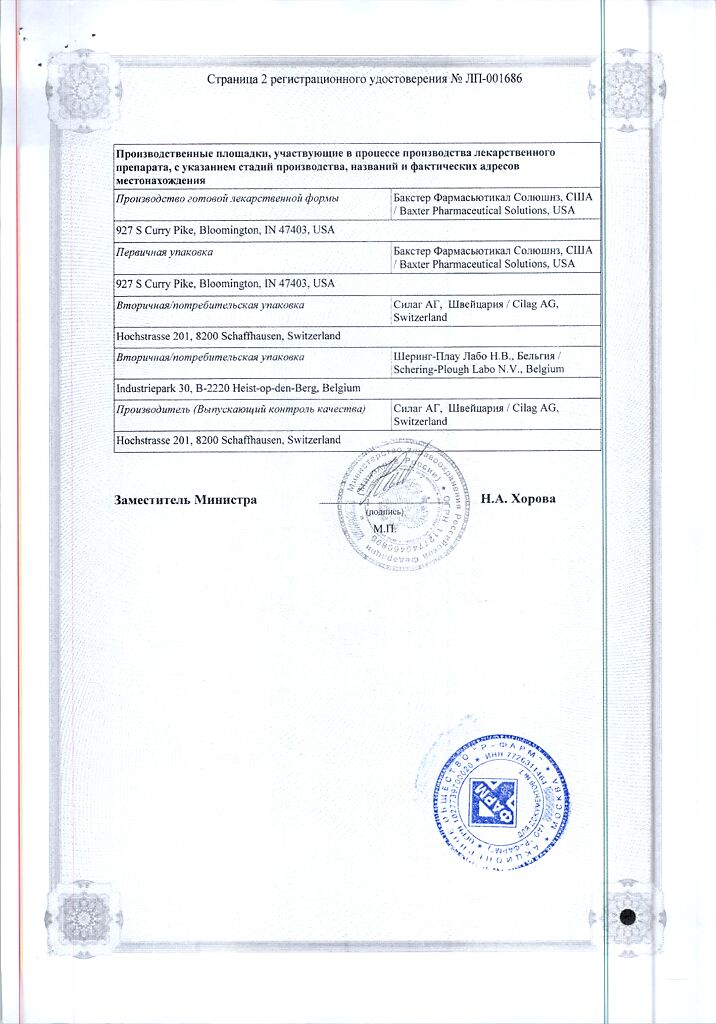
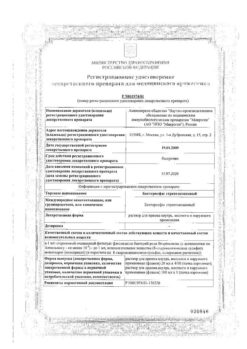
| Manufacturer | Baxter Pharmaceutical Solutions LLC, USA |
| Medication form | solution for injection |
| Brand | Baxter Pharmaceutical Solutions LLC |
Related products
Buy Simponi 50 mg/0.5 ml syringe pen with delivery to USA, UK, Europe and over 120 other countries.