No products in the cart.
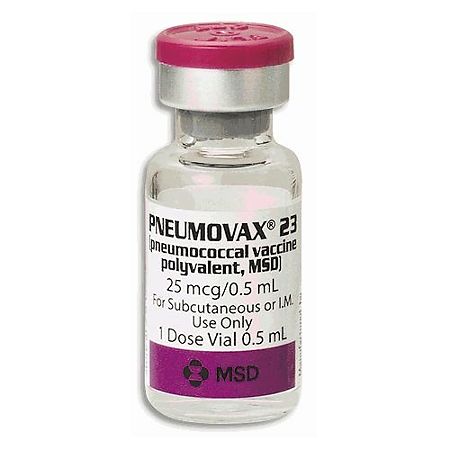
Pneumovax 23.1 dose (0.5 ml) 0.5 ml
€1.00
Out of stock
(E-mail when Stock is available)
Description
Antibacterial vaccines. Antipneumococcal vaccines. Pneumococcal purified polysaccharide antigen
Indications
Indications
– active immunization against pneumococcal infection caused by Streptococcus pneumonia serotypes (1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19F, 19A, 20, 22F, 23F, 33F) for adults and children over 2 years old
scheduled vaccination of persons over 50 years old.br>
Contingent of persons at high risk of morbidity to be vaccinated
scheduled vaccination of persons over 50 years
adults and children over 2 years of age with chronic cardiovascular disease (including congestive heart failure and cardiomyopathy), chronic lung disease (including chronic obstructive pulmonary disease and emphysema), diabetes, chronic liver disease (including cirrhosis) and alcoholism, functional or anatomic asplenia (including sickle cell anemia and splenectomies) and symptoms of liquorrhea*
Adults and children over 2 years of age with reduced immunity (immunodeficiency states in HIV, leukemia, lymphoma, Hodgkin’s disease, multiple myeloma, malignant tumors, chronic renal failure or nephrotic syndrome; caused by immunosuppressive chemotherapy (including corticosteroids); after organ transplantation or bone marrow transplantation)
Vaccination is not carried out due to ineffectiveness:
for the prevention of acute otitis media, sinusitis, and other upper respiratory tract infections
*for the prevention of pneumococcal pneumonia, in patients with spleen caused by congenital injuries, skull fractures, or neurosurgical procedures.
Active ingredient
Active ingredient
Composition
Composition
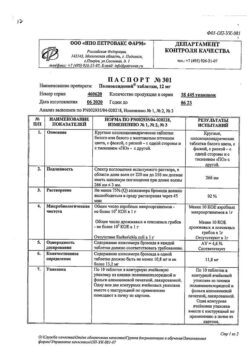
One vial (0.5 ml) of the vaccine contains
the active ingredient – pneumococcal polysaccharide,
consisting of 23 Danish pneumococcal serotypes:
1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19F, 19A, 20, 22F, 23F, 33F 25 µg of each serotype
excipients – sodium chloride,
phenol,
water for injection
How to take, the dosage
How to take, the dosage
Immunization is carried out in the summer and fall period.
Primary vaccination
Adults and children over two years of age – one single dose of 0.5 ml administered intramuscularly or subcutaneously in the deltoid muscle of the shoulder or in the middle third of the anterolateral thigh.
Peculiarities of use in chronic diseases not associated with immunosuppression
The decision on the necessity of vaccination of this category of persons should be taken on the basis of evaluation of the immune status and peculiarities of the underlying disease course.
Peculiarities of use in diseases associated with immunosuppression
It is recommended that pneumococcal vaccine should be administered two weeks (preferably) before the planned splenectomy or the beginning of chemotherapy or other immunosuppressive therapy. Vaccination should be avoided during chemotherapy or radiation therapy.
After completion of chemotherapy and/or radiation therapy due to neoplastic disease, the immune response to vaccination may remain reduced. Vaccination should not be administered earlier than three months after completion of such therapy. A longer delay may be appropriate for patients receiving intensive or prolonged therapy.
Individuals with asymptomatic or symptomatic HIV infection should be vaccinated as soon as possible after confirmation of diagnosis.
Revaccination
One single dose of 0.5 ml is given by intramuscular or subcutaneous injection into the deltoid muscle of the upper arm or lateral mid-thigh.
The schedule and timing of vaccination (revaccination) is determined according to local official recommendations. Immunocompetent patients should not be scheduled for revaccination. Revaccination is decided on an individual basis depending on patients’ antibody levels.
Revaccination may be considered for individuals at increased risk for serious pneumococcal infection who received the pneumococcal vaccine at least five years ago or for individuals with rapidly declining antipneumococcal antibody levels. Those at high risk include patients with functional or anatomic asplenia (e.g., splenectomy or sickle cell disease), HIV, leukemia, lymphoma, Hodgkin’s disease, multiple myeloma, malignant tumors, chronic renal failure, nephrotic syndrome. Persons receiving immunosuppressive chemotherapy or those who have undergone organ or bone marrow transplantation also belong to this group. For patients at high risk of fatal pneumococcal infection, revaccination after three years may be considered.
Revaccination after less than three years is not recommended because of the increased risk of adverse reactions. The incidence of local adverse reactions and, in persons aged â¥65 years, some systemic adverse reactions has been found to be higher after revaccination than after the initial vaccination when the time interval between vaccine administration is three to five years.
Children
Revaccination of children aged 2 to 10 years should be considered only 3 years after vaccination if there is an increased risk of pneumococcal infection (for example, children with nephrotic syndrome, removed spleen, or sickle cell anemia).
For children over 10 years old the recommendations on revaccination for adults are applicable.
For more detailed instructions on vaccine administration see the recommendations of the National Calendar of the Republic of Kazakhstan.
Techniques of vaccine administration
The vaccine should be used as supplied, no dilution or reconstitution is required. It is necessary to carry out visual inspection of the ampoule for integrity, color changes, precipitation. If there are changes, this vaccine should not be administered.
The vaccine is administered intramuscularly (cpm) or subcutaneously (p/k).
Do not administer intravenously or intradermally.
Take precautions to make sure the needle does not get into a blood vessel. Also, the vaccine should not be injected intradermally, as this route of administration carries an increased risk of local reactions.
Any unused product or waste should be disposed of according to local biological waste disposal requirements.
As with any vaccine, adequate medication, including epinephrine (adrenaline), should be available for immediate use if an acute anaphylactic reaction occurs.
Interaction
Interaction
Pneumococcal vaccine can be given at the same time as influenza vaccine, using individual needles and different limbs for injection.
Pneumovax 23 and Zostavax (an antiviral vaccine to prevent shingles) should not be given at the same time because this use in a clinical study resulted in decreased immunogenicity of the Zostavax vaccine. A 4-week interval between the two vaccines is recommended.
There is no experience with concomitant use with other vaccines.
Special Instructions
Special Instructions
Vaccine administration should be postponed in cases of illness accompanied by marked fever, other active infection, unless postponement would entail an even greater risk of pneumococcal infection.
As with any vaccine, adequate medication, including epinephrine (adrenaline), should be available for immediate use if an acute anaphylactic reaction develops.
Patients with immunodeficiencies
As with any vaccine, Pneumovax 23 vaccination may not be effective in all recipients. Patients with immunodeficiencies due to background conditions or treatment (e.g. immunosuppressive therapy, chemotherapy, or radiation therapy for malignancy) may not have the expected serum antibody production after the first or second dose of the vaccine. Consequently, these patients may not have adequate protection against pneumococcal disease.
In individuals receiving immunosuppressive therapy, the time interval for recovery of the immune response varies with disease and treatment. Improved immune response was observed within two years after completion of chemotherapy or other immunosuppressive therapy (with or without radiation therapy) and when the interval between the end of treatment and administration of pneumococcal vaccine was extended.
After administration of pneumococcal vaccine, appropriate antibiotic therapy to prevent pneumococcal infection in patients with immunodeficient conditions should not be stopped. The duration of antibiotic therapy should be determined by the treating physician in each clinical case.
Patients at increased risk of developing a serious pneumococcal infection (e.g., those with a removed spleen or those receiving immunosuppressive therapy for any reason) should be advised of the possible need for early antimicrobial therapy in cases of severe, acute illness accompanied by fever.
Pneumococcal vaccine may not be effective in preventing infection resulting from skull base fracture, neurosurgical procedures, or contact of cerebrospinal fluid with the outside environment.
Contraindications
Contraindications
Hypersensitivity to any component of the vaccine
-Anaphylactic reaction in the history of previous pneumococcal vaccines
-acute infectious disease or exacerbation of moderate or severe chronic disease
-children under 2 years of age
-pregnancy and lactation
Side effects
Side effects
Clinical studies found that the most common general systemic reactions to vaccine administration were: weakness, fatigue, myalgia, and headache. Patients were treated symptomatically to eliminate postvaccination reactions.
Elderly
In clinical studies, the total number of adverse reactions in patients aged 50-64 years at the vaccine injection site was 72.8% at the primary vaccination and 79.6% at the revaccination site. In patients â¥65 years of age the total number of adverse reactions at the vaccine injection site during the primary vaccination was 52.9%, during the revaccination 79.3%.
Local adverse reactions to the vaccine injection occurred on the third day after vaccination and were completely gone by the fifth day.
The total number of systemic adverse reactions at primary vaccination in patients aged 50-64 years was 48.8% and at revaccination 47.4%. In patients â¥65 years of age, the total number of systemic adverse reactions at primary vaccination was 32.1% and at revaccination 39.1%.
The total number of vaccine-related adverse reactions in patients aged 50 to 64 years was 35.5% at primary vaccination and 37.5% at revaccination. In patients ⥠65 years of age, the total number of vaccine-related adverse reactions at primary vaccination was 21.7%, at revaccination 33.1%
Children
No clinical studies have been conducted on the safety and effectiveness of Pneumovax 23 in children younger than two years. Application in this age group is not recommended as the level of produced antibodies may be insufficient.
Side effects are distributed in accordance with their frequency of their occurrence in the course of clinical trials and in the post-marketing period: very common (1/10); common (1/100 to < 1/10); infrequent (1/1,000 to < 1/100); rare (1/10,000 to < 1/1,000); very rare (< 1/10,000), unknown – (frequency cannot be determined from available data).
Very common
-fever (£38.8°C)
– erythema, swelling, pain, soreness, swelling, and local hyperthermia at the injection site
Rarely
– inflammation of subcutaneous fatty tissue that developed at the vaccine injection site in the immediate post-vaccination period
br>
Unknown
-sthenia, chills, restricted mobility and peripheral swelling of the limb where the injection was given, malaise
-hemolytic anemia in patients with other hematologic disorders, leukocytosis, lymphadenitis, lymphadenopathy, thrombocytopenia in patients with idiopathic thrombocytopenic purpura with stable platelet levels
-anaphylactoid reactions, Quincke’s edema, serum disease – febrile seizures, Guillain-Barré syndrome, headache, paresthesia, radiculoneuropathy
– nausea, vomiting
-rash, urticaria, erythema multiforme
-arthralgia, arthritis, myalgia
-increase in C-reactive protein level.
Similarities
Similarities
Additional information
| Manufacturer | Merck Sharp & Home Corp. |
|---|---|
| Medication form | solution |
| Brand | #Н/Д |
Related products
Buy Pneumovax 23.1 dose (0.5 ml) 0.5 ml with delivery to USA, UK, Europe and over 120 other countries.