No products in the cart.
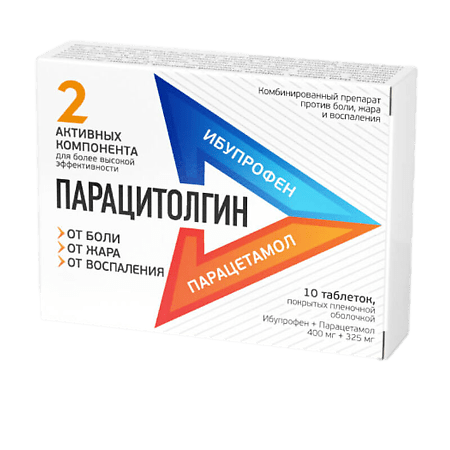
Paracytolgin, 400 mg+325 mg 10 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group Anallergic agent, combined (NSAID + non-narcotic analgesic).
ATX code: M01AE51
Pharmacological properties
Pharmacodynamics.
A combination drug, the action of which is due to its constituent components. It has a directed effect against pain (analgesic), antipyretic and anti-inflammatory effects.
Ibuprofen and paracetamol differ in mechanism and site of action. Their mutually reinforcing action results in a more pronounced decrease in pain sensitivity and an increase in antipyretic effect than separately.
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) with analgesic, anti-inflammatory, antipyretic effects. Inhibiting cyclooxygenase (COX) 1 and 2, disrupts metabolism of arachidonic acid, reduces the number of prostaglandins (mediators of pain, inflammation and hyperthermia), both in the focus of inflammation and in healthy tissues, inhibits the exudative and proliferative phases of inflammation. Ibuprofen inhibits the migration of leukocytes to the center of inflammation.
The analgesic effect of ibuprofen is provided by its inhibitory action at the peripheral level. Antipyretic effect of ibuprofen is associated with central inhibition of prostaglandin synthesis in hypothalamus.
Paracetamol is an analgesic non-narcotic agent and has analgesic, antipyretic and mild anti-inflammatory effects. Paracetamol indiscriminately blocks COX, mainly in the central nervous system, has little effect on water-salt metabolism and the mucosa of the gastrointestinal tract (GIT). It has analgesic and antipyretic effects. Paracetamol can also stimulate the activity of descending serotonin pathways, which leads to knocking out the transmission of the pain impulse in the spinal cord. At the peripheral level, paracetamol has a weak effect on COX-1 and COX-2.
It relieves arthralgia at rest and on movement, reduces morning stiffness and joint swelling, and promotes increased range of motion.
Pharmacokinetics
Ibuprofen<
Absorption is high, rapidly and almost completely absorbed from the gastrointestinal tract. Detected in blood plasma 5 minutes after the drug is taken on an empty stomach, time to reach maximum concentration (TCmah) after oral administration – about 1-2 hours. Binding to plasma proteins is more than 90%. The elimination half-life (T1/2) is about 2 hours. Slowly penetrates into the joint cavity, accumulates in synovial fluid, creating higher concentrations in it than in blood plasma. After absorption, about 60% of the pharmacologically inactive R-form is slowly transformed into the active S-form. It is metabolized in the liver. More than 90% is excreted by the kidneys (not more than 1% unchanged) and to a lesser extent in the bile as metabolites and their conjugates.
Paracetamol
Absorption is high, quickly absorbed from the gastrointestinal tract. Binding to plasma proteins is less than 10% and increases slightly in overdose. Sulfate and glucuronide metabolites do not bind to plasma proteins even in relatively high concentrations. Cmax value is 5-20 µg/ml, Tcmax is 0.5-2 hours.
It is quite evenly distributed in the fluid medium of the body. It penetrates through the blood-brain barrier.
It is detected in plasma 5 minutes after the drug intake on an empty stomach, Cmax in plasma is reached 30-40 minutes after intake. The degree of absorption of paracetamol is independent of food intake. About 90-95% of paracetamol is metabolized in the liver to form inactive conjugates with glucuronic acid (60%), taurine (35%) and cysteine (3%), and a small amount of hydroxylated and deacetylated metabolites. A small part of the drug is hydroxylated by microsomal enzymes to form highly active N-acetyl-n-benzoquinonimine, which binds to sulfhydryl groups of glutathione. When glutathione stores in the liver are depleted (in overdose) the enzyme systems of hepatocytes can be blocked, leading to the development of their necrosis.
The elimination half-life (T1/2) is 2-3 hours. In patients with cirrhosis the T1/2 increases slightly. The drug clearance is decreased and the elimination half-life is increased in elderly patients. It is excreted by the kidneys mainly as glucuronide and sulfate conjugates (less than 5% unchanged). Less than 1% of the administered dose of paracetamol penetrates into breast milk. In children the ability to form conjugates with glucuronic acid is lower than in adults.
Indications
Indications
– headache (including migraine);
– toothache;
– back pain;
– myalgia;
– algodismenorrhea (painful menstruation);
– neuralgia;
– joint pain, pain syndrome in inflammatory and degenerative diseases of the joints and spine;
– pain from bruises, sprains, dislocations, fractures;
– post-traumatic and postoperative pain syndrome.
– febrile conditions (including flu and colds), accompanied by fever, chills, headache, muscle and joint pain, sore throat.
The drug is intended for symptomatic therapy, reducing pain and inflammation at the time of use. The drug does not affect the progression of the disease.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Analgesic drug, combined (NSAID + analgesic non-narcotic drug).
ATX code: M01AE51
Pharmacological properties
Pharmacodynamics
A combined drug whose effect is determined by its constituent components. It has a targeted effect against pain (analgesic), antipyretic and anti-inflammatory effect.
Ibuprofen and paracetamol differ in their mechanism and site of action. As a result of their mutually reinforcing action, a more pronounced decrease in pain sensitivity and an increase in antipyretic effect is achieved than individually.
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that has analgesic, anti-inflammatory, and antipyretic effects. By inhibiting cyclooxygenase (COX) 1 and 2, it disrupts the metabolism of arachidonic acid, reduces the amount of prostaglandins (mediators of pain, inflammation and hyperthermic reaction), both in the site of inflammation and in healthy tissues, suppresses the exudative and proliferative phases of inflammation. Ibuprofen inhibits the migration of leukocytes to the site of inflammation.
The analgesic effect of ibuprofen is provided by its inhibitory effect at the peripheral level. The antipyretic effect of ibuprofen is associated with central inhibition of prostaglandin synthesis in the hypothalamus.
Paracetamol is an analgesic non-narcotic drug that has analgesic, antipyretic and weak anti-inflammatory effects. Paracetamol indiscriminately blocks COX, mainly in the central nervous system, and has little effect on water-salt metabolism and the mucous membrane of the gastrointestinal tract (GIT). Has an analgesic and antipyretic effect. Paracetamol can also stimulate the activity of the descending serotonin pathways, which leads to the inhibition of the transmission of pain impulses in the spinal cord. At the peripheral level, paracetamol has a weak effect on COX-1 and COX-2.
Relieves arthralgia at rest and during movement, reduces morning stiffness and swelling of joints, and helps increase range of motion.
Pharmacokinetics
Ibuprofen
Absorption is high, quickly and almost completely absorbed from the gastrointestinal tract. Detected in the blood plasma 5 minutes after taking the drug on an empty stomach, the time to reach the maximum concentration (TCmax) after oral administration is about 1-2 hours. The connection with blood plasma proteins is more than 90%. The half-life (T1/2) is about 2 hours. It slowly penetrates into the joint cavity, accumulates in the synovial fluid, creating higher concentrations in it than in the blood plasma. After absorption, about 60% of the pharmacologically inactive R-form is slowly transformed into the active S-form. Metabolized in the liver. More than 90% is excreted by the kidneys (no more than 1% unchanged) and to a lesser extent with bile in the form of metabolites and their conjugates.
Paracetamol
Absorption is high, quickly absorbed from the gastrointestinal tract. Plasma protein binding is less than 10% and increases slightly with overdose. Sulfate and glucuronide metabolites do not bind to plasma proteins even at relatively high concentrations. The Cmax value is 5-20 μg/ml, Tcmax is 0.5-2 hours.
Distributed fairly evenly in body fluids. Penetrates the blood-brain barrier.
Detected in the blood plasma 5 minutes after taking the drug on an empty stomach, Cmax in the blood plasma is achieved 30-40 minutes after administration. The degree of absorption of paracetamol does not depend on food intake. About 90-95% of paracetamol is metabolized in the liver to form inactive conjugates with glucuronic acid (60%), taurine (35%) and cysteine (3%), as well as a small amount of hydroxylated and deacetylated metabolites. A small portion of the drug is hydroxylated by microsomal enzymes to form highly active N-acetyl-n-benzoquinone imine, which binds to the sulfhydryl groups of glutathione. When glutathione reserves in the liver are depleted (in case of overdose), the enzyme systems of hepatocytes can be blocked, leading to the development of their necrosis.
The half-life (T1/2) is 2-3 hours. In patients with liver cirrhosis, T1/2 increases slightly. In elderly patients, drug clearance decreases and the half-life increases. It is excreted by the kidneys mainly in the form of glucuronide and sulfate conjugates (less than 5% unchanged). Less than 1% of the administered dose of paracetamol passes into breast milk. In children, the ability to form conjugates with glucuronic acid is lower than in adults.
Special instructions
Special instructions
It is recommended to take the drug in the shortest possible short course and in the minimum effective dose necessary to eliminate symptoms.
In patients with bronchial asthma or allergic diseases in the acute stage, as well as in patients with a history of bronchial asthma/allergic diseases, the drug may provoke bronchospasm.
Use of the drug in patients with systemic lupus erythematosus or mixed connective tissue disease is associated with an increased risk of developing aseptic meningitis.
Patients with hypertension, including a history of hypertension and/or chronic heart failure, should consult a physician before using the drug, as the drug may cause fluid retention, increased blood pressure, and edema. In patients with uncontrolled hypertension, NYHA class II-III congestive heart failure, coronary artery disease, peripheral arterial disease and/or cerebrovascular disease, ibuprofen should be prescribed only after a careful benefit-risk assessment, and high doses of ibuprofen (≥2400 mg/day) should be avoided.
The use of NSAIDs in patients with chickenpox may be associated with an increased risk of developing severe purulent complications of infectious and inflammatory diseases of the skin and subcutaneous fat (for example, necrotizing fasciitis). In this regard, it is recommended to avoid using the drug for chickenpox.
Information for women planning pregnancy: the drug suppresses COX and prostaglandin synthesis, affects ovulation, disrupting female reproductive function (reversible after discontinuation of the drug).
The simultaneous use of the drug with other drugs containing paracetamol and/or non-steroidal anti-inflammatory drugs should be avoided. When using the drug for more than 5-7 days as prescribed by a doctor, peripheral blood counts and the functional state of the liver should be monitored.
With the simultaneous use of indirect anticoagulants, it is necessary to monitor the indicators of the blood coagulation system.
To avoid possible damaging effects on the liver, you should not drink alcohol while taking the drug.
The drug may distort the results of laboratory tests when quantitatively determining glucose, uric acid in blood serum, and 17-ketosteroids (the drug must be discontinued 48 hours before the test).
Impact on the ability to drive vehicles and machinery
During the treatment period, the patient should refrain from engaging in potentially hazardous activities that require increased attention and speed of psychomotor reactions.
Active ingredient
Active ingredient
Ibuprofen, Paracetamol
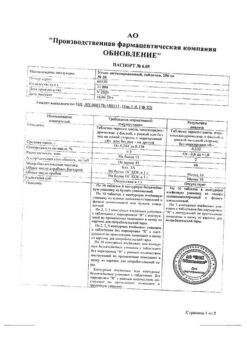
Composition
Composition
One film-coated tablet contains:
Active ingredients:
Ibuprofen 400.00 mg
Paracetamol 325.00 mg
Kernel excipients:
Microcrystalline cellulose M 102 76.00 mg
Corn starch 65.25 mg
Glycerol (glycerin) 3.00 mg
Sodium carboxymethyl starch (sodium starch glycolate (type A), Primogel) 14.25 mg
Colloidal silicon dioxide 38.00 mg
Talc 19.00 mg
Magnesium stearate 9.50 mg
Shell composition:
Hypromellose 12.90 mg
Macrogol-4000 3.20 mg
Titanium dioxide 2.30 mg
Propylene glycol 1.60 mg
Pregnancy
Pregnancy
In the first and second trimesters of pregnancy, the use of the drug is possible only as prescribed by a doctor in cases where the potential benefit outweighs the possible risk to the mother and the potential risk to the fetus. The use of the drug in the third trimester of pregnancy is contraindicated.
If it is necessary to use the drug during breastfeeding, breastfeeding should be stopped.
Experimental studies have not established the embryotoxic, teratogenic and mutagenic effects of the drug components.
Before using the drug, if you are pregnant or think you might be pregnant, or are planning a pregnancy, you should consult your doctor.
Contraindications
Contraindications
Increased individual sensitivity to the components of the drug (including other NSAIDs).
Erosive and ulcerative diseases of the gastrointestinal tract (including gastric and duodenal ulcers, Crohn’s disease, ulcerative colitis) or ulcerative bleeding in the active phase or in history (two or more confirmed episodes of peptic ulcer or ulcerative bleeding).
Cerebrovascular or other bleeding.
Hemophilia or other bleeding disorders (including hypocoagulation), hemorrhagic diathesis, intracranial hemorrhage.
Severe renal failure (creatinine clearance (CC) less than 30 ml/min).
Complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses, and intolerance to acetylsalicylic acid or other NSAIDs (including a history).
Severe heart failure (class IV according to the New York Heart Association NYHA classification).
Decompensated heart failure.
Optic nerve damage.
Genetic absence of glucose-6-phosphate dehydrogenase.
Diseases of the blood system.
The period after coronary artery bypass surgery.
Progressive kidney diseases.
Severe liver failure or active liver disease.
Confirmed hyperkalemia.
Pregnancy (III trimester).
Children under 18 years of age.
With caution
Coronary heart disease, chronic heart failure, peripheral arterial disease, arterial hypertension, blood diseases of unknown etiology (leukopenia and anemia), cerebrovascular diseases, dyslipidemia/hyperlipidemia.
A history of a single episode of gastric and duodenal ulcers or ulcerative bleeding of the gastrointestinal tract, a history of Helicobacter pylori infection, gastritis, enteritis, colitis, ulcerative colitis.
Viral hepatitis, moderate and mild liver failure, benign hyperbilirubinemia (Gilbert, Dubin-Johnson and Rotor syndrome), liver cirrhosis with portal hypertension.
Renal failure, including dehydration (creatinine clearance less than 30-60 ml/min), nephrotic syndrome.
Bronchial asthma or allergic diseases in the acute stage or in the anamnesis may develop bronchospasm.
Systemic lupus erythematosus or mixed connective tissue disease (Sharp’s syndrome) – increased risk of aseptic meningitis.
Chickenpox, severe somatic diseases, diabetes mellitus.
Concomitant use of other NSAIDs, oral glucocorticosteroids (including prednisolone), anticoagulants (including warfarin), antiplatelet agents (including acetylsalicylic acid, clopidogrel), selective serotonin reuptake inhibitors (including citalopram, fluoxetine, paroxetine, sertraline).
Old age, smoking, alcoholism.
Pregnancy I-II trimester, breastfeeding period.
Side Effects
Side Effects
To determine the frequency of side effects of the drug, the following classification is used: very often (≥1/10), often (≥1/100 and <1/10), infrequently (≥1/1000 and <1/100), rarely (≥1/10,000 and <1/1000), very rarely (≥1/10,000).
Gastrointestinal disorders
NSAID gastropathy – nausea, vomiting, heartburn, anorexia, discomfort or pain in the epigastrium, diarrhea, flatulence; rarely – erosive and ulcerative lesions, bleeding; liver dysfunction, hepatitis, pancreatitis: irritation or dryness in the mouth, pain in the mouth, ulceration of the gum mucosa, aphthous stomatitis; constipation. Peptic ulcer, melena, hematemesis, in some cases fatal, especially in elderly patients, gastritis, exacerbation of colitis and Crohn’s disease, increased activity of liver transaminases, jaundice.
Disorders of the nervous system and sensory organs
Headache, dizziness, insomnia, anxiety, nervousness, irritability, agitation, drowsiness, depression, confusion, hallucinations; rarely – aseptic meningitis (more often in patients with autoimmune diseases); hearing loss, tinnitus, visual impairment, toxic damage to the optic nerve, blurred vision or double vision, scotoma, amblyopia.
Cardiovascular disorders
Heart failure, peripheral edema, with long-term use there is an increased risk of thrombotic complications (for example, myocardial infarction), increased blood pressure, tachycardia.
Blood and lymphatic system disorders
Anemia (including hemolytic and aplastic), thrombocytopenia, thrombocytopenic purpura, agranulocytosis, leukopenia, pancytopenia.
Disorders of the respiratory system and mediastinal organs
Shortness of breath, bronchospasm, bronchial asthma.
Renal and urinary tract disorders
Allergic nephritis, acute renal failure, nephrotic syndrome, edema, polyuria, cystitis, hematuria, proteinuria, nephritic syndrome, papillary necrosis, interstitial nephritis.
Allergic reactions
Skin rash, itching, urticaria, Quincke’s edema, bronchospasm, dyspnea, allergic rhinitis, dry and irritated eyes, swelling of the conjunctiva and eyelids, eosinophilia, fever, anaphylactic shock, erythema multiforme exudative (Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell’s syndrome).
Laboratory indicators
Decreased serum glucose concentration, decreased hematocrit and hemoglobin, increased bleeding time, increased serum creatinine concentration.
Others
Increased sweating.
With long-term use in high doses: ulceration of the mucous membrane of the gastrointestinal tract, bleeding (gastrointestinal, gingival, uterine, hemorrhoidal), visual impairment (impaired color vision, scotoma, amblyopia).
If you experience the side effects listed in the instructions, or they get worse, or you notice any other side effects not listed in the instructions, tell your doctor.
Interaction
Interaction
With the simultaneous use of the drug Paracitolgin with drugs, various interaction effects may develop:
antiemetics: decreased rate of absorption of paracetamol when used simultaneously with metoclopramide or domperidone;
anticoagulants: long-term use of drugs containing paracetamol may enhance the effect of anticoagulants, in particular warfarin, and increase the risk of bleeding;
antacids, cholestyramine: decreased rate of absorption of paracetamol;
with simultaneous use, ibuprofen reduces the anti-inflammatory and antiplatelet effect of acetylsalicylic acid (an increase in the incidence of acute coronary insufficiency in patients receiving small doses of acetylsalicylic acid as an antiplatelet agent is possible after starting ibuprofen);
other NSAIDs, in particular selective COX-2 inhibitors: simultaneous use of two or more drugs from the NSAID group should be avoided due to a possible increased risk of side effects;
ibuprofen enhances the effect of direct (heparin) and indirect (coumarin and indanedione derivatives) anticoagulants, thrombolytic agents (alteplase, anistreplase, streptokinase, urokinase), antiplatelet agents, colchicine – the risk of developing hemorrhagic complications increases;
insulin and oral hypoglycemic drugs: increased hypoglycemic effect;
antihypertensive drugs (ACE inhibitors and angiotensin II antagonists) and diuretics: NSAIDs may reduce the effectiveness of drugs in these groups. In some patients with impaired renal function (eg, dehydrated patients or elderly patients with impaired renal function), co-administration of ACE inhibitors or angiotensin II antagonists and cyclooxygenase inhibitors may lead to a deterioration of renal function, including the development of acute renal failure (usually reversible). These interactions should be considered in patients taking coxibs concomitantly with ACE inhibitors or angiotensin II antagonists. In this regard, the combined use of the above drugs should be prescribed with caution, especially in the elderly. It is necessary to prevent dehydration in patients, and consider monitoring renal function after initiation of this combination treatment and periodically thereafter. Diuretics and ACE inhibitors may increase the nephrotoxicity of NSAIDs;
glucocorticosteroids: increased risk of gastrointestinal ulcers and gastrointestinal bleeding;
ethanol, corticotropin: increased risk of erosive and ulcerative lesions of the gastrointestinal tract;
antiplatelet agents and selective serotonin reuptake inhibitors: increased risk of gastrointestinal bleeding;
cardiac glycosides: simultaneous administration of NSAIDs and cardiac glycosides can lead to worsening heart failure, a decrease in glomerular filtration rate and an increase in the concentration of cardiac glycosides in the blood plasma;
lithium preparations, methotrexate: there is evidence of the likelihood of an increase in the concentration of lithium in the blood plasma during the use of NSAIDs;
cyclosporine: increased risk of nephrotoxicity with simultaneous administration of NSAIDs and cyclosporine;
gold preparations: increased risk of nephrotoxicity with simultaneous administration of NSAIDs and gold preparations;
mifepristone: NSAIDs should be started no earlier than 8-12 days after taking mifepristone, since NSAIDs may reduce the effectiveness of mifepristone;
tacrolimus: with simultaneous administration of NSAIDs and tacrolimus, the risk of nephrotoxicity may increase;
Zidovudine: Concomitant use of NSAIDs and zidovudine may result in increased hematotoxicity. There is evidence of an increased risk of hemarthrosis and hematomas in HIV-positive patients with hemophilia who received concomitant treatment with zidovudine and ibuprofen;
quinolone antibiotics: in patients receiving concomitant treatment with NSAIDs and quinolone antibiotics, the risk of seizures may increase;
cefamandole, cefoperazone, cefotetan, valproic acid, plicamycin: increased incidence of hypoprothrombinemia;
myelotoxic drugs increase the manifestation of hematotoxicity of the drug;
caffeine enhances the analgesic effect;
drugs that block tubular secretion: decreased excretion and increased plasma concentration of ibuprofen;
inducers of microsomal oxidation (phenytoin, ethanol, barbiturates, rifampicin, phenylbutazone, tricyclic antidepressants): increased production of hydroxylated active metabolites, increased risk of developing severe intoxications;
microsomal oxidation inhibitors: reducing the risk of hepatotoxicity;
uricosuric drugs: decreased effectiveness of drugs.
If you are using the above or other medications (including over-the-counter medications), consult your doctor before using Paracitolgin.
Overdose
Overdose
Symptoms: gastrointestinal disorders (diarrhea, nausea, vomiting, anorexia, pain in the epigastric region), increased prothrombin time, bleeding after 12-48 hours, lethargy, drowsiness, depression, headache, tinnitus, impaired consciousness, cardiac arrhythmias, decreased blood pressure, manifestations of hepato- and nephrotoxicity, convulsions, possible development hepatonecrosis. If you suspect an overdose, you should immediately seek medical help.
Treatment: gastric lavage during the first 4 hours; alkaline drinking, forced diuresis; activated carbon orally, administration of SH-group donors and precursors for the synthesis of glutathione-methionine 8-9 hours after an overdose and N-acetylcysteine orally or intravenously – after 12 hours, antacid drugs; hemodialysis; symptomatic therapy.
The need for additional therapeutic measures (further administration of methionine, intravenous administration of N-acetylcysteine) is determined depending on the concentration of paracetamol in the blood, as well as the time elapsed after its administration.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C.
Keep out of the reach of children.
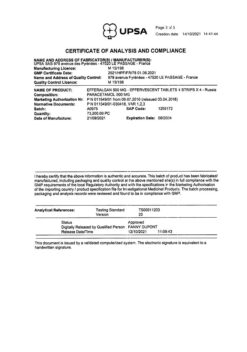
Shelf life
Shelf life
3 years.
Do not use after expiration date.
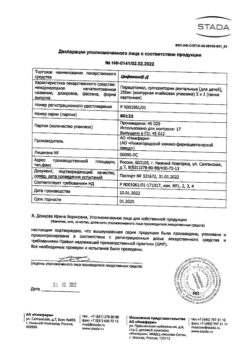
Manufacturer
Manufacturer
Sintez, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | At a temperature not higher than 25 ° C. Keep out of reach of children. |
| Manufacturer | Sintez OAO, Russia |
| Medication form | pills |
| Brand | Sintez OAO |
Other forms…
Related products
Buy Paracytolgin, 400 mg+325 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.