No products in the cart.
Nimulide, 100 mg 20 pcs.
€13.44 €11.20
Description
Nimulide is a non-narcotic anti-inflammatory drug (NSAID) of sulfonanilide class, a selective COX-2 inhibitor. It has anti-inflammatory, analgesic, antipyretic effects.
Nimesulide belongs to NSAIDs, the mechanism of action of which is connected with selective inhibition of COX-2 and influence on several other factors – inhibition of platelet-activating factor, tumor necrosis factor-alpha, inhibition of proteinases and histamine.
By selectively inhibiting COX-2 it decreases biosynthesis of PG in inflammation focus, has less pronounced inhibitory effect on COX-1 (less often causes side effects associated with inhibition of PG synthesis in healthy tissues).
Indications
Indications
Acute pain therapy:
– pain in the lower back and/or lumbar region;
– pain syndrome associated with diseases of the musculoskeletal system, including tendinitis, bursitis;
– pain from bruises, sprains and dislocations of joints;
– toothache;
– symptomatic treatment of osteoarthritis (osteoarthritis) with pain syndrome;
– primary algodismenorrhea.
The drug is intended for symptomatic therapy, reducing pain and inflammation at the time of use, does not affect the progression of the disease.
Nimesulide is recommended for therapy as a second-line drug.
Pharmacological effect
Pharmacological effect
PHARMACOTHERAPEUTIC GROUP
Non-steroidal anti-inflammatory drug (NSAID).
ATX code: M01AX17
PHARMACOLOGICAL PROPERTIES
Pharmacodynamics
Nimeulide is a non-steroidal anti-inflammatory drug from the sulfonamide class. Provides anti-inflammatory, analgesic and
antipyretic effect. Unlike non-selective NSAIDs, nimesulide mainly inhibits cyclooxygenase-2 (COX-2), inhibits the synthesis of prostaglandins at the site of inflammation; has a less pronounced inhibitory effect on cyclooxygenase-1 (COX-1).
Pharmacokinetics
Suction
Nimesulide is well absorbed from the gastrointestinal tract (GIT). The maximum concentration in blood plasma (Cmax) after oral administration of a single dose of nimesulide (100 mg) is achieved on average after 2-3 hours and is 3-4 mg/l.
Distribution
Communication with blood plasma proteins up to 97.5%. Penetrates into the tissues of the female genital organs, where after a single dose its concentration is about 40% of the concentration in plasma. Penetrates well into the acidic environment of the inflammation site (40%) and synovial fluid (43%). Easily penetrates histohematic barriers.
Metabolism
Nimesulide is actively metabolized in the liver using the cytochrome P450 (CYP)2C9 isoenzyme. There is a possibility of drug interaction with nimesulide when used simultaneously with drugs metabolized by the CYP2C9 isoenzyme. The main metabolite is the pharmacologically active parahydroxy derivative of nimesulide – hydroxynimesulide, found in blood plasma mainly in conjugated form, in the form of glucuronate.
Removal
The half-life (T1/2) of nimesulide is about 1.56-4.95 hours, hydroxynimesulide – 2.89-4.78 hours. Nimesulide is excreted from the body by the kidneys (65%) and bile (35%), and undergoes enterohepatic recirculation.
Use in patients with kidney disease
In a short-term study conducted in patients with mild to moderate renal failure (creatinine clearance 30-60 ml/min), Cmax of nimesulide and its main metabolite were no higher than in healthy volunteers. AUC and T1/2 were 50% higher, but were within the range of AUC and T1/2 values observed in healthy volunteers when using nimesulide. Repeated use did not lead to the accumulation of nimesulide.
Special instructions
Special instructions
Undesirable side effects can be minimized by using the drug in the minimum effective dose with the minimum duration of use necessary to relieve pain.
There is evidence of very rare cases of serious liver reactions, including deaths, associated with the use of nimesulide-containing drugs. If symptoms similar to signs of liver damage appear (anorexia, itching, yellowing of the skin, nausea, vomiting, abdominal pain, dark urine, increased activity of liver transaminases), you should immediately stop using nimesulide and consult a doctor. Repeated use of nimesulide in such patients is contraindicated.
After 2 weeks of using the drug, monitoring of liver function parameters (“transaminases”) is necessary.
Liver reactions, which are in most cases reversible, have been reported with short-term use of the drug.
While using nimesulide, the patient should refrain from taking other analgesics, including NSAIDs (including selective COX-2 inhibitors).
Nimesulide should be used with caution in patients with a history of gastrointestinal diseases (ulcerative colitis, Crohn’s disease), since exacerbation of these diseases is possible.
The risk of gastrointestinal bleeding, peptic ulcer/perforation of the stomach or duodenum increases in patients with a history of ulcerative lesions of the gastrointestinal tract (ulcerative colitis, Crohn’s disease), as well as in elderly patients, with increasing doses of NSAIDs, so treatment should begin with the lowest possible dose. In such patients, as well as in patients who require the simultaneous use of low doses of acetylsalicylic acid or other drugs that increase the risk of complications from the gastrointestinal tract,
additionally prescribe gastroprotectors (misoprostol or proton pump blockers). Patients with a history of gastrointestinal disease, especially older patients, should report new gastrointestinal symptoms (especially symptoms that may indicate possible gastrointestinal bleeding) to their physician.
Nimesulide should be administered with caution to patients taking medications that increase the risk of ulceration or bleeding (oral corticosteroids, anticoagulants such as warfarin, selective serotonin reuptake inhibitors or antiplatelet agents such as acetylsalicylic acid).
If gastrointestinal bleeding or gastrointestinal ulceration occurs in patients taking nimesulide, treatment with the drug should be stopped immediately.
Given reports of visual impairment in patients taking other NSAIDs, if any visual impairment occurs, use of nimesulide should be immediately discontinued and an ophthalmological examination performed.
The drug can cause fluid retention in tissues, therefore, in patients with arterial hypertension, renal and/or heart failure, coronary heart disease, peripheral arterial disease and/or cerebrovascular diseases, with risk factors for the development of cardiovascular diseases (for example: hyperlipidemia, diabetes mellitus, smokers), nimesulide should be used with special attention.
caution. If the condition worsens, treatment with nimesulide should be stopped.
Clinical studies and epidemiological data suggest that NSAIDs, especially in high doses and with long-term use, may lead to a slight increase in the risk of myocardial infarction or stroke. There is insufficient data to exclude the risk of such events when using nimesulide.
If signs of a “cold” or acute respiratory viral infection occur during the use of nimesulide, the drug should be discontinued.
Nimesulide can change the properties of platelets, so caution must be exercised when using the drug in people with hemorrhagic diathesis, however, the drug does not replace the preventive effect of acetylsalicylic acid in cardiovascular diseases.
Elderly patients are especially susceptible to adverse reactions to NSAIDs, including the risk of life-threatening gastrointestinal bleeding and perforation, and decreased renal, liver, and cardiac function. When taking nimesulide for this category of patients, proper clinical monitoring is necessary.
There is evidence of the occurrence in rare cases of skin reactions (such as exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis) when taking NSAIDs, including nimesulide. At the first manifestations of a skin rash, damage to the mucous membranes or other signs of an allergic reaction, nimesulide should be stopped immediately.
The use of the drug may adversely affect female fertility and is not recommended for women planning pregnancy.
INFLUENCE ON THE ABILITY TO DRIVE VEHICLES, MECHANISMS
The effect of nimesulide on the ability to drive vehicles and machines has not been studied, however, given the undesirable reactions from the nervous system (dizziness, drowsiness), you should refrain from driving vehicles and other machines.
Active ingredient
Active ingredient
Nimesulide
Composition
Composition
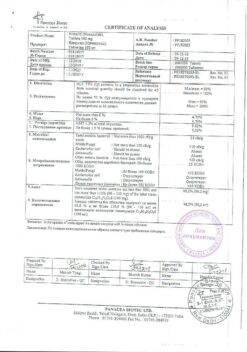
Each lozenge contains:
Active ingredient: nimesulide 100.00 mg
Excipients:
Mannitol 187.85 mg, sodium carboxymethyl starch 15.00 mg, aspartame 7.00 mg, magnesium stearate 5.00 mg, colloidal silicon dioxide 5.00 mg, croscarmellose sodium 3.00 mg, orange flavor 1.50 mg, potassium sorbate 0.346 mg, sodium methyl parahydroxybenzoate 0.281 mg, sodium propyl parahydroxybenzoate 0.021 mg.
Pregnancy
Pregnancy
Pregnancy
Like other drugs from the class of NSAIDs that inhibit the synthesis of prostaglandins, nimesulide can adversely affect the course of pregnancy and/or the development of the embryo and can lead to premature closure of the ductus arteriosus, hypertension in the fetal pulmonary artery system, impaired renal function, which can progress to renal failure with oliuria in the fetus, an increased risk of bleeding, decreased contractility of the uterus, and the occurrence of peripheral edema in the mother.
The use of nimesulide during breastfeeding is contraindicated.
Contraindications
Contraindications
Hypersensitivity to nimesulide or other components of the drug; complete or incomplete combination of bronchial asthma, recurrent nasal polyposis, paranasal sinuses and intolerance to acetylsalicylic acid and other NSAIDs (including a history); hepatotoxic reactions with potential hepatotoxicity (eg, other NSAIDs); chronic inflammatory bowel diseases (Crohn’s disease, ulcerative colitis) in the acute phase; period after coronary artery bypass surgery; febrile syndrome with colds and acute respiratory viral infections; suspicion of acute surgical pathology; peptic ulcer of the stomach or duodenum in the acute phase; erosive and ulcerative lesions of the gastrointestinal tract
intestinal tract in the acute phase; history of erosive and ulcerative lesions of the gastrointestinal tract; history of perforation or gastrointestinal bleeding, including those associated with previous NSAID therapy; history of cerebrovascular bleeding, other active bleeding or diseases accompanied by increased bleeding; severe blood clotting disorders; severe heart failure; severe renal failure (creatinine clearance less than 30 ml/min); progressive kidney disease; confirmed hyperkalemia; liver failure, active liver disease; children under 12 years of age; pregnancy and breastfeeding; alcoholism, drug addiction.
WITH CAUTION
Arterial hypertension; coronary heart disease; cerebrovascular diseases; severe heart failure; dyslipidemia/hyperlipidemia; diabetes mellitus; peripheral arterial disease; hemorrhagic diathesis; smoking; renal failure (creatinine clearance 30-60 ml/min); anamnestic data on the development of erosive and ulcerative lesions of the gastrointestinal tract, the presence of Helicobacter pylori infection; old age; long-term use of non-steroidal anti-inflammatory drugs; frequent alcohol consumption, severe somatic diseases, systemic lupus erythematosus (SLE) and other systemic connective tissue diseases; concomitant therapy with the following drugs:
– anticoagulants (for example, warfarin),
– antiplatelet agents (for example, acetylsalicylic acid, clopidogrel),
– oral glucocorticosteroids (for example, prednisolone),
– selective serotonin reuptake inhibitors (for example, citalopram, fluoxetine, paroxetine, sertraline).
Side Effects
Side Effects
The frequency is classified according to the recommendations of the World Health Organization, depending on the occurrence of the case: very common (≥ 1/10), common (≥ 1/100, < 1/10), uncommon (≥ 1/1000, < 1/100), rare (≥ 1/10000, < 1/1000), very rare (< 1/10000), including individual reports.
Blood and lymphatic system disorders
Rarely: anemia, eosinophilia, hemorrhage;
Very rare: thrombocytopenia, pancytopenia, thrombocytopenic purpura, prolonged bleeding time.
Immune system disorder
Interaction
Interaction
Glucocorticosteroids increase the risk of erosive and ulcerative lesions of the gastrointestinal tract or bleeding.
Antiplatelet agents and selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine, increase the risk of gastrointestinal bleeding.
Anticoagulants. NSAIDs may enhance the effect of anticoagulants such as warfarin or drugs that have antiplatelet effects such as acetylsalicylic acid. Due to the increased risk of bleeding, this combination is not recommended and is contraindicated in patients with severe coagulation disorders. If combination therapy cannot be avoided, careful monitoring of blood clotting parameters is necessary.
Other non-steroidal anti-inflammatory drugs (NSAIDs):
The simultaneous use of nimesulide-containing drugs with other NSAIDs, including acetylsalicylic acid in a single dose of more than 1 g or in a daily dose of more than 3 g, is not recommended.
Diuretics. NSAIDs may reduce the effect of diuretics.
In healthy volunteers, nimesulide temporarily reduces the excretion of sodium under the influence of furosemide, to a lesser extent – the excretion of potassium and reduces the actual diuretic effect.
The simultaneous use of nimesulide and furosemide leads to a decrease (by approximately 20%) in the area under the concentration-time curve (AUC) and a decrease in the cumulative excretion of furosemide without changing the renal clearance of furosemide.
The simultaneous use of furosemide and nimesulide requires caution in patients with renal or heart failure.
ACE inhibitors and angiotensin II receptor antagonists.
NSAIDs may reduce the effect of antihypertensive drugs. In patients with mild to moderate renal failure (creatinine clearance 30-60 ml/min), with simultaneous use of ACE inhibitors, angiotensin II receptor antagonists and drugs that suppress the cyclooxygenase system (NSAIDs, antiplatelet agents), further deterioration of renal function and the occurrence of acute renal failure, which is usually reversible, is possible. These interactions should be considered in patients taking nimesulide in combination with ACE inhibitors or angiotensin II receptor antagonists. Therefore, the simultaneous use of these drugs should be used with caution, especially in elderly patients. Patients should
Receive adequate fluids and renal function should be closely monitored after concomitant use is initiated.
Mifepristone.
Due to the theoretical risk of changes in the effectiveness of mifepristone under the influence of prostaglandin synthesis inhibitors, NSAIDs should not be used earlier than 8-12 days after discontinuation of mifepristone.
There is evidence that NSAIDs reduce the clearance of lithium, which leads to increased plasma lithium concentrations and its toxicity. When using nimesulide in patients undergoing lithium therapy, the concentration of lithium in the blood plasma should be regularly monitored.
No clinically significant interactions were observed with glibenclamide, theophylline, digoxin, cimetidine and antacid drugs (for example, a combination of aluminum and magnesium hydroxides).
Nimesulide inhibits the activity of the CYP2C9 isoenzyme. When drugs that are substrates of this enzyme are used simultaneously with nimesulide, the concentration of the latter in plasma may increase.
When prescribing nimesulide less than 24 hours before or after taking methotrexate, caution is required, since in such cases the level of methotrexate in the blood plasma and, accordingly, toxic effects may increase.
Due to their effect on renal prostaglandins, inhibitors of prostaglandin synthetase, such as nimesulide, may increase the nephrotoxicity of cyclosporines.
In vitro studies have shown that nimesulide is displaced from binding sites by tolbutamide, salicylic acid and valproic acid. Despite the fact that these interactions were determined in blood plasma, these effects were not observed during clinical use of the drug
Overdose
Overdose
Symptoms: apathy, drowsiness, nausea, vomiting, pain in the epigastric region. These symptoms are usually reversible with symptomatic and supportive therapy. Gastrointestinal bleeding, arterial hypertension, acute renal failure, respiratory depression, coma, anaphylactoid reactions may occur.
Treatment: symptomatic and supportive therapy. There is no specific antidote. If an overdose occurs within the last 4 hours, it is necessary to induce vomiting, take activated carbon (60-100 g per adult) and/or an osmotic laxative. Forced diuresis, hemodialysis, hemoperfusion, and urine alkalization are ineffective due to the high binding of the drug to proteins. It is necessary to monitor the state of kidney and liver function.
Storage conditions
Storage conditions
In a place protected from light, at a temperature not exceeding 25 ° C.
Keep out of the reach of children.
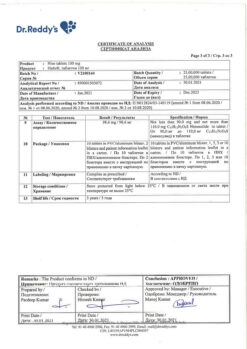
Shelf life
Shelf life
3 years.
Do not use the drug after the expiration date indicated on the package.
Manufacturer
Manufacturer
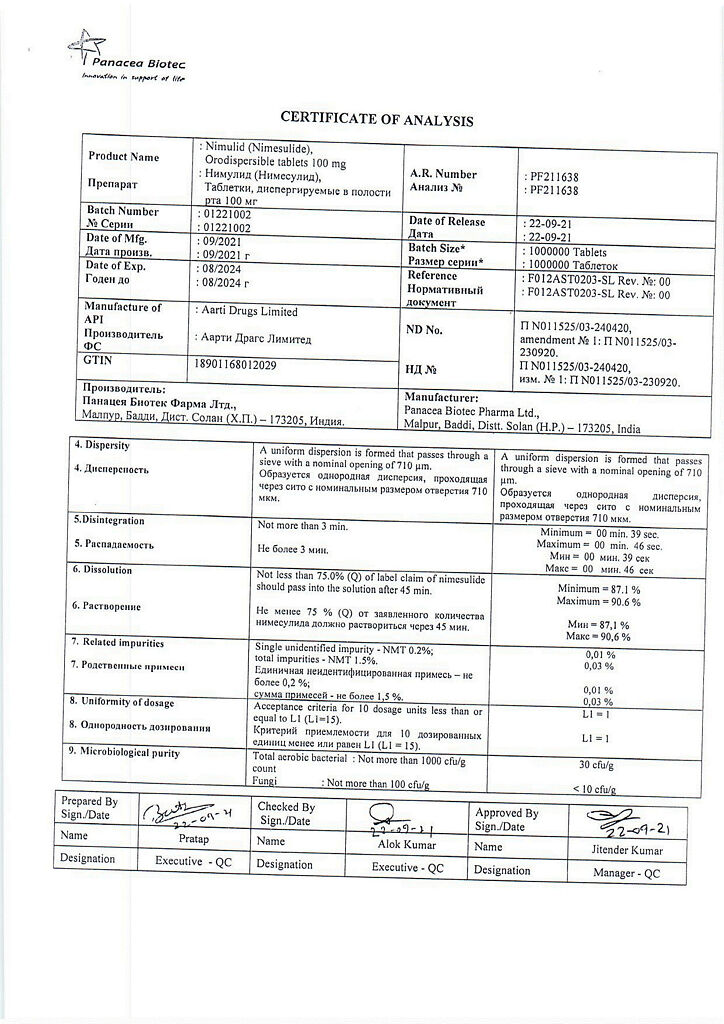
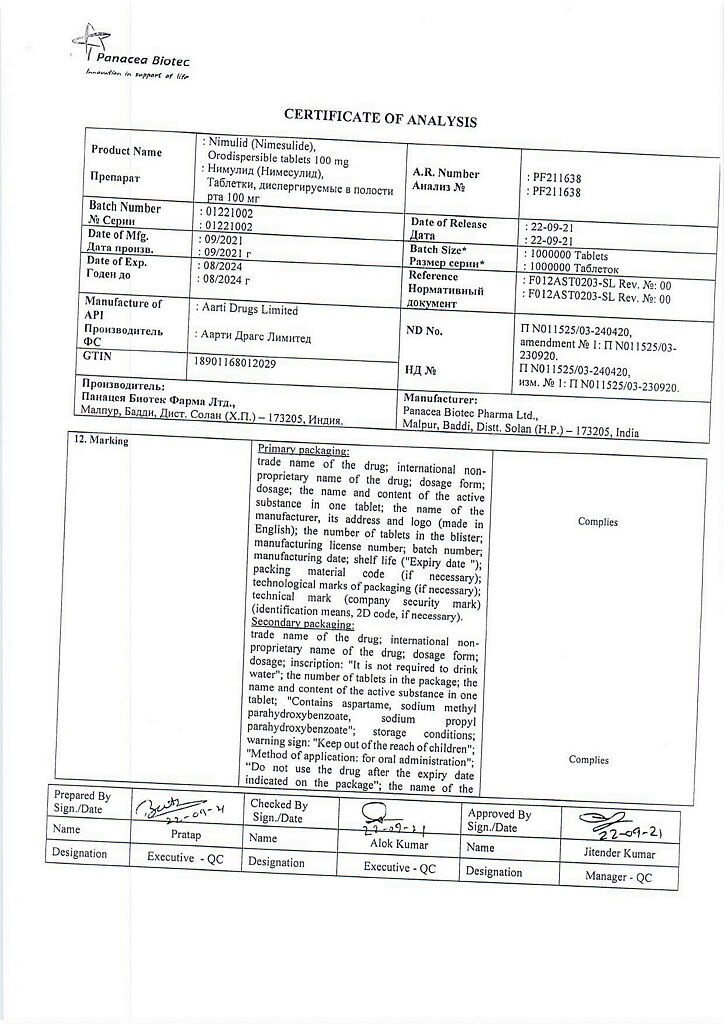
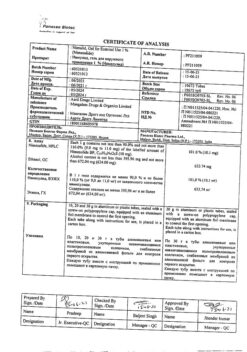
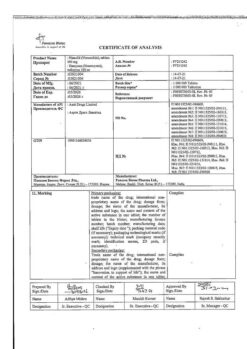
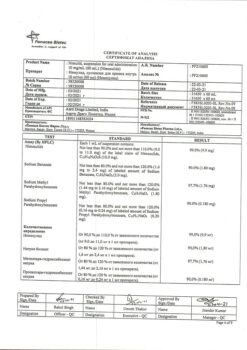
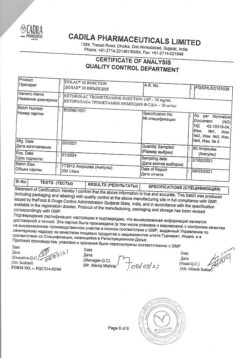
Panacea Biotech, India
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C |
| Manufacturer | Panacea Biotec, India |
| Medication form | Oral dispersible tablets |
| Brand | Panacea Biotec |
Other forms…
Related products
Buy Nimulide, 100 mg 20 pcs. with delivery to USA, UK, Europe and over 120 other countries.