No products in the cart.
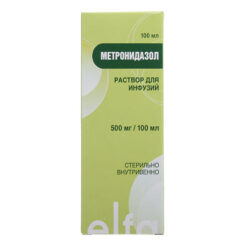
Metronidazole, tablets 250 mg 40 pcs
€6.41 €5.00
Description
Pharmacotherapeutic group: antimicrobial and antiprotozoal agent
ATX code: J01XD01
Pharmacological properties
Pharmacodynamics
Metronidazole is a 5-nitroimidazole derivative. The mechanism of action of metronidazole consists in biochemical reduction of the 5-nitrogroup of metronidazole by intracellular transport proteins of anaerobic microorganisms and protozoa. The reduced 5-nitrogroup of metronidazole interacts with the deoxyribonucleic acid (DNA) of the microbial cell, inhibiting the synthesis of their nucleic acids, which leads to the death of the microorganisms.
Active against Trichomonas vaginalis, Entamoeba histolytica, as well as Gram-negative anaerobes Bacteroides spp. (including B. fragilis, B. distasonis, B. ovatus, B. thetaiotaomicron, B. vulgatus), Fusobacterium spp, and some gram-positive anaerobes (sensitive strains of Eubacterium spp., Clostridium spp., Peptococcus niger., Peptostreptococcus spp.). The minimum suppressive concentration for these strains is 0.125-6.25 µg/ml. In combination with amoxicillin it shows activity against Helicobacter pylori (amoxicillin suppresses development of resistance to metronidazole).
Metronidazole is not sensitive to aerobic microorganisms and facultative anaerobes, but in the presence of mixed flora (aerobes and anaerobes) metronidazole acts synergistically with antibiotics effective against common aerobes.
Pharmacokinetics
Metronidazole is rapidly and almost completely absorbed when ingested (about 80% in 1 hour). Food intake has no effect on absorption of metronidazole. Bioavailability is at least 80%. After oral administration of metronidazole in a dose of 500 mg, its concentration in blood plasma is 10 µg/ml after 1 hour, 13.5 µg/ml after – 3 hours. Binding to blood proteins is insignificant and does not exceed 10-20%. Metronidazole quickly penetrates into tissues (lungs, kidneys, liver, skin, bile, cerebrospinal fluid, saliva, seminal fluid, vaginal secretion), into breast milk and passes through the placental barrier. About 30-60% of metronidazole is metabolized by hydroxylation, oxidation and glucuronidation. The main metabolite (2-oxymetronidazole) also has antiprotozoal and antimicrobial effects.
40-70% of metronidazole is excreted by the kidneys (unchanged – about 35% of the taken dose). The elimination half-life is 8-10 hours.
In patients with impaired renal function when taking metronidazole during a course of treatment, its concentration in serum may increase.
Indications
Indications
Protozoal infections: extraintestinal amebiasis (including amoebic liver abscess), intestinal amebiasis (amoebic dysentery), trichomoniasis.
Infections caused by Bacteroides spp. (including B. fragilis, B. distasonis, B. ovatus, B. thetaiotaomicron, B. vulgatus); infections of bones and joints, infections of the central nervous system (CNS), including meningitis, brain abscess; bacterial endocarditis; pneumonia, empyema and lung abscess; sepsis.
Infections caused by Clostridium spp., Peptococcus niger and Peptostreptococcus spp.: abdominal infections (peritonitis, liver abscess), pelvic infections (endometritis, fallopian tube and ovarian abscess, vaginal vault infections).
Antibiotic-associated pseudomembranous colitis.
Gastritis or duodenal ulcer associated with Helicobacter pylori (as part of complex therapy).
Prevention of postoperative complications (especially after operations on the colon, in the pararectal area, appendectomy, gynecological operations).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antimicrobial and antiprotozoal agent
ATX code: J01XD01
Pharmacological properties
Pharmacodynamics
Metronidazole is a derivative of 5-nitroimidazole. The mechanism of action of metronidazole is the biochemical reduction of the 5-nitro group of metronidazole by intracellular transport proteins of anaerobic microorganisms and protozoa. The reduced 5-nitro group of metronidazole interacts with the deoxyribonucleic acid (DNA) of microbial cells, inhibiting the synthesis of their nucleic acids, which leads to the death of microorganisms.
Active against Trichomonas vaginalis, Entamoeba histolytica, as well as gram-negative anaerobes Bacteroides spp. (including B. fragilis, B. distasonis, B. ovatus, B. thetaiotaomicron, B. vulgatus), Fusobacterium spp., and some gram-positive anaerobes (susceptible strains of Eubacterium spp., Clostridium spp., Peptococcus niger., Peptostreptococcus spp.). The minimum inhibitory concentration for these strains is 0.125-6.25 μg/ml. In combination with amoxicillin, it is active against Helicobacter pylori (amoxicillin suppresses the development of resistance to metronidazole).
Aerobic microorganisms and facultative anaerobes are not sensitive to metronidazole, but in the presence of mixed flora (aerobes and anaerobes), metronidazole acts synergistically with antibiotics effective against common aerobes.
Pharmacokinetics
When taken orally, metronidazole is rapidly and almost completely absorbed (approximately 80% in 1 hour). Eating does not affect the absorption of metronidazole. Bioavailability is at least 80%. After oral administration of metronidazole at a dose of 500 mg, its concentration in the blood plasma is 10 mcg/ml after 1 hour, 13.5 mcg/ml after 3 hours. Binding to blood proteins is insignificant and does not exceed 10-20%. Metronidazole quickly penetrates into tissues (lungs, kidneys, liver, skin, bile, cerebrospinal fluid, saliva, seminal fluid, vaginal secretions), into breast milk and passes through the placental barrier. About 30-60% of metronidazole is metabolized by hydroxylation, oxidation and glucuronidation. The main metabolite (2-oxymetronidazole) also has antiprotozoal and antimicrobial effects.
40-70% of metronidazole is excreted by the kidneys (unchanged – about 35% of the dose taken). The half-life is 8-10 hours.
In patients with impaired renal function, a course of taking metronidazole may increase its concentration in the blood serum.
Special instructions
Special instructions
Since simultaneous use of metronidazole with alcohol (ethanol) can have an effect similar to that of disulfiram (skin hyperemia, flushing of the skin, vomiting, tachycardia), patients should be warned that during treatment and for at least one day after stopping use of the drug, they should not drink alcoholic beverages or medications containing ethanol.
You should carefully weigh the indications for long-term use of the drug and, in the absence of strict indications, avoid its long-term use. If, in the presence of strict indications, the drug is used for a longer period than is usually recommended, then treatment should be carried out under the control of hematological parameters (especially leukocytes) and adverse reactions, such as peripheral or central neuropathy, manifested (paresthesia, ataxia, dizziness, convulsions), upon the occurrence of which treatment should be discontinued.
When treating trichomonas vaginitis in women and trichomonas urethritis in men, it is necessary to abstain from sexual intercourse. Simultaneous treatment of sexual partners is mandatory. Treatment should not be stopped during menstruation. After treatment for trichomoniasis, control tests should be carried out during 3 consecutive cycles before and after menstruation.
Severe hepatotoxicity/acute liver failure (including fatal cases that occurred very rapidly after initiation of treatment) has been reported in patients with Cockayne syndrome when treated with systemic metronidazole. In this category of patients, metronidazole should be prescribed only after a careful assessment of the benefit/risk ratio and only in the absence of alternative treatment.
Liver function tests should be performed before the start of treatment, during therapy and after its completion until liver function tests reach normal values, or until the initial values of these indicators are achieved. If liver function indicators are significantly exceeded during treatment, then use of the drug should be discontinued.
Patients with Cockayne syndrome should be advised to immediately report the development of any symptoms of potential liver damage to their physician and discontinue use of metronidazole.
It must be taken into account that metronidazole can immobilize treponemes, which leads to a false-positive Nelson test.
Impact on the ability to drive vehicles and machinery
Considering the risk of developing such adverse reactions as confusion, dizziness, hallucinations, visual impairment, it is recommended during treatment to refrain from driving or engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Metronidazole
Composition
Composition
For one tablet:
Active ingredient: metronidazole – 250 mg.
Excipients: potato starch, stearic acid, povidone (low molecular weight medical polyvinylpyrrolidone 12600±2700, plasdon K-17), sucrose (powdered sugar).
Pregnancy
Pregnancy
Since metronidazole crosses the placental barrier and its effect on human fetal organogenesis is unknown, the use of the drug during pregnancy is contraindicated.
Metronidazole passes into breast milk, so the use of the drug during breastfeeding is contraindicated.
Contraindications
Contraindications
– hypersensitivity to metronidazole, to other nitroimidazole derivatives, to imidazoles or to other components of the drug;
– organic lesions of the central nervous system (including epilepsy);
– leukopenia (including history);
– liver failure (in case of prescribing large doses);
– pregnancy;
– period of breastfeeding;
– children under 6 years of age;
– sucrase/isomaltase deficiency, fructose intolerance, glucose-galactose malabsorption.
With caution
– hepatic encephalopathy;
– acute and chronic diseases of the peripheral and central nervous system (risk of worsening neurological symptoms);
– renal failure.
Side Effects
Side Effects
Gastrointestinal disorders
– Epigastric pain, nausea, vomiting, diarrhea.
– Inflammation of the oral mucosa (glossitis, stomatitis), taste disturbances (“metallic” taste in the mouth), decreased appetite, anorexia, dry oral mucosa, constipation.
– Pancreatitis (reversible cases).
– Change in the color of the tongue/”coated” tongue (due to excessive growth of fungal microflora).
Immune system disorders
– Angioedema, anaphylactic shock.
Nervous system disorders
– Peripheral sensory neuropathy.
– Headache, cramps, dizziness.
– The development of encephalopathy (for example, confusion) and subacute cerebellar syndrome (impaired coordination and synergism of movements, ataxia, dysarthria, gait disturbances, nystagmus and tremor), which reverse after discontinuation of metronidazole, have been reported.
– Aseptic meningitis.
Mental disorders
– Psychotic disorders, including confusion, hallucinations.
– Depression, insomnia, irritability, increased excitability.
Visual disorders
– Transient visual impairments such as diplopia, myopia, blurred vision, decreased visual acuity, impaired color perception.
– Neuropathy/optic neuritis.
Hearing and labyrinth disorders
– Hearing impairment/hearing loss (including sensorineural deafness).
– Noise in the ears.
Blood and lymphatic system disorders
– Agranulocytosis, leukopenia, neutropenia and thrombocytopenia.
Disorders of the liver and biliary tract
– Increased activity of liver enzymes (aspartate aminotransferase (AST) and alanine aminotransferase (ALT), alkaline phosphatase), development of cholestatic or mixed hepatitis, hepatocellular liver damage, sometimes accompanied by jaundice.
– Cases of liver failure requiring liver transplantation have been observed in patients treated with metronidazole in combination with other antibiotics.
Skin and subcutaneous tissue disorders
– Rash, itching, flushing of the skin, skin hyperemia, urticaria.
– Pustular skin rash.
– Fixed drug rash.
– Stevens-Johnson syndrome, toxic epidermal necrolysis.
Renal and urinary tract disorders
– Urine may be brownish-reddish in color, due to the presence of a water-soluble metabolite of metronidazole in the urine.
– Dysuria, polyuria, cystitis, urinary incontinence, candidiasis.
General and administration site disorders
– Fever, nasal congestion, arthralgia, weakness.
Laboratory and instrumental data
– Flattening of the T wave on the ECG.
Interaction
Interaction
With disulfiram
The development of psychotic reactions has been reported in patients receiving concomitant metronidazole and disulfiram (the interval between the use of these drugs should be at least 2 weeks).
With ethanol
Disulfiram-like reactions may occur (hyperemia of the skin, flushing of the skin, vomiting, tachycardia).
With indirect anticoagulants (warfarin)
Increased anticoagulant effect and increased risk of bleeding associated with decreased hepatic metabolism of indirect anticoagulants, which can lead to prolongation of prothrombin time. In case of simultaneous use of metronidazole and indirect anticoagulants, more frequent monitoring of prothrombin time and, if necessary, dose adjustment of anticoagulants is required.
With lithium preparations
With the simultaneous use of metronidazole with lithium preparations, the concentration of the latter in the blood plasma may increase. With simultaneous use, the concentrations of lithium, creatinine and electrolytes in the blood plasma should be monitored.
With cyclosporine
With simultaneous use of metronidazole with cyclosporine, the concentration of cyclosporine in the blood plasma may increase. If simultaneous use of metronidazole and cyclosporine is necessary, the concentrations of cyclosporine and creatinine in the blood plasma should be monitored.
With cimetidine
Cimetidine inhibits the metabolism of metronidazole, which may lead to an increase in its concentration in the blood plasma and an increased risk of side effects.
With drugs that induce microsomal oxidation isoenzymes in the liver (phenobarbital, phenytoin)
The simultaneous use of metronidazole with drugs that induce microsomal oxidation isoenzymes in the liver (phenobarbital, phenytoin) can accelerate the elimination of metronidazole, resulting in a decrease in its concentration in the blood plasma.
With fluorouracil
Metronidazole reduces the clearance of fluorouracil, leading to increased toxicity.
With busulfan
Metronidazole increases the concentration of busulfan in the blood plasma, which can lead to the development of severe toxic effects of busulfan.
With non-depolarizing muscle relaxants (vecuronium bromide)
It is not recommended for use with non-depolarizing muscle relaxants (vecuronium bromide).
With sulfonamides
Sulfonamides enhance the antimicrobial effect of metronidazole.
Overdose
Overdose
Ingestion of single doses of metronidazole up to 12 g has been reported in suicide attempts and accidental overdoses.
Symptoms: vomiting, ataxia, slight disorientation.
Treatment: There is no specific antidote for metronidazole overdose. If a significant dose overdose is suspected, symptomatic and supportive therapy should be provided.
Storage conditions
Storage conditions
In a place protected from light at a temperature not exceeding 25 ° C. Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after expiration date.
Manufacturer
Manufacturer
Velfarm LLC, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store in a dark place at a temperature not exceeding 25 °С. Keep out of reach of children. |
| Manufacturer | Welfarm, Russia |
| Medication form | pills |
| Brand | Welfarm |
Other forms…
Related products
Buy Metronidazole, tablets 250 mg 40 pcs with delivery to USA, UK, Europe and over 120 other countries.