No products in the cart.
Lopirel, 75 mg 28 pcs.
€15.14 €13.12
Description
Pharmacotherapeutic group: anti-aggregant drug
ATX code:
Pharmacological properties
Pharmacodynamics
Mechanism of action
Clopidogrel is a prodrug, one of whose metabolites is active and inhibits platelet aggregation. The active metabolite clopidogrel selectively inhibits adenosine diphosphate (ADP) binding to the P2Y12 receptor of platelets and subsequent ADP-mediated activation of the glycoprotein IIb/IIIa complex, leading to suppression of platelet aggregation. Through irreversible binding, platelets remain immune to ADP stimulation for the remainder of their lives (approximately 7-10 days), and recovery of normal platelet function occurs at a rate consistent with the rate of platelet renewal.
The aggregation of platelets caused by agonists other than ADP is also inhibited by blocking the enhanced activation of platelets by the released ADP. Because the formation of the active metabolite occurs via P450 system isoenzymes, some of which may be polymorphic or may be inhibited by other drugs, adequate inhibition of platelet aggregation is not possible in all patients.
Pharmacodynamic properties
When clopidogrel is taken daily at a dose of 75 mg, significant inhibition of ADP-induced platelet aggregation is noted from the first day of administration, which gradually increases over 3-7 days and then reaches a constant level (when the equilibrium state is reached). In the equilibrium state at a dose of 75 mg/day, platelet aggregation is suppressed by an average of 40-60%. After stopping clopidogrel administration, platelet aggregation and bleeding time gradually return to baseline within an average of 5 days.
Clinical efficacy and safety
Clopidogrel can prevent the development of atherothrombosis in any localization of atherosclerotic vascular lesions, particularly in lesions of the cerebral, coronary or peripheral arteries.
.The ACTIVE-A clinical trial showed that patients with atrial fibrillation who had at least one risk factor for vascular complications but were unable to take indirect anticoagulants, clopidogrel combined with acetylsalicylic acid (compared with taking acetylsalicylic acid alone) reduced the incidence of stroke, myocardial infarction, systemic thromboembolism outside the central nervous system (CNS), or vascular mortality combined, more by reducing the risk of stroke.
The efficacy of clopidogrel in combination with acetylsalicylic acid was detected early and persisted for up to 5 years. The reduction in the risk of major vascular complications in the group of patients who took clopidogrel in combination with acetylsalicylic acid was mainly due to a greater reduction in the incidence of strokes. The risk of stroke of any severity when receiving clopidogrel in combination with acetylsalicylic acid decreased, and there was a tendency to a lower incidence of myocardial infarction in the group treated with clopidogrel in combination with acetylsalicylic acid, but there were no differences in the frequency of non-CNS thromboembolism or vascular death. In addition, taking clopidogrel in combination with acetylsalicylic acid reduced the total number of days of hospitalization for cardiovascular causes.
Pharmacokinetics
absorption
Clopidogrel is rapidly absorbed after a single dose and when taken orally at a dose of 75 mg/day. Mean values of maximum plasma concentrations (Cmax) of unchanged clopidogrel are about 2.2-2.5 ng/ml and are reached about 45 minutes after intake. According to the excretion of clopidogrel metabolites by the kidneys, its absorption is at least 50%.
Distribution
In vitro clopidogrel and its major circulating inactive metabolite are reversibly bound to plasma proteins by 98% and 94%, respectively. In vitro this binding is unsaturated over a wide range of concentrations.
Metabolism
Clopidogrel is extensively metabolized in the liver. In vitro and in vivo clopidogrel is metabolized in two ways: the first is through esterases and subsequent hydrolysis to form an inactive carboxylic acid derivative (85%) from metabolites circulating in the systemic bloodstream, and the second way is through the cytochrome P450 system. Initially, clopidogrel is metabolized to 2-oxoclopidogrel, which is an intermediate metabolite. Subsequent metabolism of
2-oxoclopidogrel leads to the formation of the active metabolite of clopidogrel – thiol derivative of clopidogrel. In vitro this metabolic pathway occurs with the participation of the CYP3A4, CYP2C19, CYP1A2 and CYP2B6 isoenzymes. The active thiol metabolite of clopidogrel, which has been isolated in in vitro studies, binds rapidly and irreversibly to platelet receptors, thus inhibiting platelet aggregation.
The Cmax of the active metabolite is 2 times greater than the Cmax when clopidogrel is taken at a single loading dose of 300 mg for 4 days. Cmax active metabolite is reached 30-60 min after clopidogrel administration.
Elimation
For 120 hours after human oral administration of 14C-labeled clopidogrel, approximately 50% of the radioactivity is excreted through the kidneys and approximately 46% of the radioactivity through the gut. After a single oral dose of 75 mg, the half-life (T1/2) of clopidogrel is about 6 hours. After a single dose and repeated doses, the T1/2 of the main circulating inactive metabolite in blood is 8 hours.
Pharmacogenetics
The CYP2C19 isoenzyme is used to form both the active metabolite and the intermediate metabolite, 2-oxlopidogrel. The pharmacokinetics and antiaggregant effects of the active metabolite clopidogrel, when studied in platelet aggregation ex vivo, vary depending on the genotype of the CYP2C19 isoenzyme.
The CYP2C19*1 gene allele corresponds to fully functional metabolism, whereas the CYP2C19*2 and CYP2C19*3 gene alleles are nonfunctional. The CYP2C19*2 and CYP2C19*3 gene alleles cause reduced metabolism in the majority of Caucasoid (85%) and Mongoloid races (99%). Other alleles that are associated with absence or reduced metabolism are less common and include, but are not limited to, CYP2C19*4, *5, *6, *7, and *8 alleles. Patients who are poor metabolizers must have the two loss-of-function gene alleles listed above. The published frequencies of CYP2C19 weak metabolizer phenotypes are 2% in Caucasian race individuals, 4% in non-Hispanic race individuals, and 14% in Chinese individuals.
.In a cross-sectional study conducted on 40 volunteers, 10 people in each group with four subtypes of the CYP2C19 isoenzyme (ultrafast metabolizers, intensive metabolizers, intermediate metabolizers, weak metabolizers) were evaluated for pharmacokinetics and antiplatelet effects when clopidogrel was given at a dose of 300 mg followed by 75 mg/day and when clopidogrel was given at a dose of 600 mg followed by 150 mg/day for 5 days (reaching equilibrium). No significant differences in active metabolite exposure and mean values of platelet aggregation inhibition (IAT) (induced by ADP) were found in ultrafast, intensive and intermediate metabolizers. Weak metabolizers had a 63-71% reduction in active metabolite exposure compared with intensive metabolizers. When the 300 mg/75 mg treatment regimen was used, antiplatelet action was reduced in weak metabolizers with average IAT values of 24% (after 24 h) and 37% (by day 5 of treatment) compared to IAT values of 39% (after 24 h) and 58% (by day 5 of treatment) in intensive metabolizers and 37% (after 24 h) and 60% (by day 5 of treatment) in intermediate metabolizers. When weak metabolizers received the 600 mg/150 mg treatment regimen, exposure to the active metabolite was higher than when receiving the 300 mg/75 mg treatment regimen. In addition, IAT was 32% (after 24 h) and 61% (on day 5 of treatment), which was higher in weak metabolizers receiving the 300 mg/75 mg regimen and was similar to that in the groups of patients with higher CYP2C19-metabolism intensity receiving the 300 mg/75 mg regimen. However, the dosing regimen of clopidogrel for patients in this group has not yet been established in studies with clinical outcomes.
.Consistent with the results of this study, a meta-analysis of six studies that included data from 335 volunteers who received clopidogrel and were at equilibrium concentrations showed that intermediate metabolizers had a 28% reduction in active metabolite exposure and weak metabolizers had a 72% reduction in IAT, although IAT was reduced compared with intensive metabolizers with differences in IAT of 5.9% and 21.4%, respectively.
No impact of CYP2C19 genotype on clinical outcomes in patients treated with clopidogrel has been evaluated in prospective, randomized, controlled trials. However, several retrospective analyses are currently available. Genotyping results are available in the following clinical trials: CURE (n=2721), CHARISMA (n=2428), CLARITY-TIMI 28 (n=227), TRITON-TIMI 38 (n=1477) and ACTIVE-A (n=601) as well as several published cohort studies.
In the TRITON-TIMI 38 study and 3 cohort studies (Collet, Sibbing, Giusti), patients in the combined group with intermediate or poor metabolism had a higher incidence of cardiovascular complications (death, myocardial infarction, and stroke) or stent thrombosis compared with those in intensive metabolizers.
In the CHARISMA study and one cohort study (Simon), increased rates of cardiovascular complications were observed only in weak metabolizers (when compared with intensive metabolizers).
In the CURE, CLARITY, ACTIVE-A, and one cohort study (Trenk), there was no increase in the incidence of cardiovascular complications as a function of CYP2C19-metabolism intensity.
The clinical studies conducted to date have not had sufficient sample size to detect differences in clinical outcome in patients with low CYP2C19 isoenzyme activity.
Pharmacokinetics in special clinical cases
The pharmacokinetics of the active metabolite clopidogrel in selected groups of patients has not been studied.
In elderly volunteers (over 75 years of age), no differences in platelet aggregation and bleeding time were obtained when compared to younger volunteers. No dose adjustment is required in elderly patients.
Pharmacokinetics of clopidogrel in children has not been studied.
.In patients with severe renal impairment (creatinine clearance (CK) 5-15 ml/min) after repeated doses of clopidogrel at 75 mg/day initiation of ADP-induced platelet aggregation was lower (25%) compared to that in healthy volunteers, but prolongation of bleeding time was similar to that in healthy volunteers receiving clopidogrel at 75 mg/day. Clopidogrel was well tolerated in all patients.
In patients with severe liver injury, inhibition of ADP-induced platelet aggregation was similar to that in healthy volunteers after daily clopidogrel doses of 75 mg/day for 10 days. The mean bleeding time was also comparable in both groups.
The prevalence of CYP2C9 isoenzyme gene alleles responsible for intermediate and reduced metabolism is different between racial groups. There is very little literature data among members of the Mongoloid race, which makes it impossible to assess the significance of CYP2C19 isoenzyme genotyping for the development of ischemic complications.
Indications
Indications
Prevention of atherothrombotic complications
In adult patients with myocardial infarction (with a duration of several days to 35 days), ischemic stroke (with a duration of 7 days to 6 months) or with diagnosed peripheral arterial occlusive disease.
In adult patients with acute coronary syndrome:
without ST segment elevation (unstable angina or non-Q wave myocardial infarction), including patients who underwent stenting during percutaneous coronary intervention (in combination with acetylsalicylic acid);
with ST segment elevation (acute myocardial infarction) with drug treatment and the possibility of thrombolysis (in combination with acetylsalicylic acid).
Prevention of atherothrombotic and thromboembolic complications, including stroke, in atrial fibrillation (atrial fibrillation).
Patients with atrial fibrillation (atrial fibrillation) who have at least one risk factor for the development of vascular complications cannot take indirect anticoagulants and have a low risk of bleeding (in combination with acetylsalicylic acid).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antiplatelet agent
ATX code:
Pharmacological properties
Pharmacodynamics
Mechanism of action
Clopidogrel is a prodrug, one of whose metabolites is active and inhibits platelet aggregation. The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to the platelet P2Y12 receptor and subsequent ADP-mediated activation of the glycoprotein IIb/IIIa complex, leading to suppression of platelet aggregation. Due to irreversible binding, platelets remain immune to ADP stimulation for the remainder of their life (approximately 7-10 days), and restoration of normal platelet function occurs at a rate consistent with platelet turnover.
Platelet aggregation caused by agonists other than ADP is also inhibited by blocking enhanced platelet activation by released ADP. Since the formation of the active metabolite occurs with the help of isoenzymes of the P450 system, some of which may differ in polymorphism or may be inhibited by other drugs, adequate inhibition of platelet aggregation is not possible in all patients.
Pharmacodynamic properties
When taking clopidogrel daily at a dose of 75 mg, from the first day of administration there is a significant suppression of ADP-induced platelet aggregation, which gradually increases over 3-7 days and then reaches a constant level (when an equilibrium state is reached). At steady state, when taking a dose of 75 mg/day, platelet aggregation is suppressed by an average of 40-60%. After discontinuation of clopidogrel, platelet aggregation and bleeding time gradually returned to baseline levels within an average of 5 days.
Clinical efficacy and safety
Clopidogrel is able to prevent the development of atherothrombosis in any localization of atherosclerotic vascular lesions, in particular in lesions of the cerebral, coronary or peripheral arteries.
The ACTIVE-A clinical trial showed that in patients with atrial fibrillation who had at least one risk factor for vascular complications but were unable to take indirect anticoagulants, clopidogrel in combination with acetylsalicylic acid (compared with acetylsalicylic acid alone) reduced the incidence of stroke, myocardial infarction, and non-central systemic thromboembolism combined. nervous system (CNS) or vascular mortality, largely due to a reduced risk of stroke.
The effectiveness of taking clopidogrel in combination with acetylsalicylic acid was detected early and persisted for up to 5 years. The reduction in the risk of major vascular complications in the group of patients taking clopidogrel in combination with acetylsalicylic acid was mainly due to a greater reduction in the incidence of stroke. The risk of stroke of any severity was reduced when taking clopidogrel in combination with acetylsalicylic acid, and there was a trend towards a decrease in the incidence of myocardial infarction in the group treated with clopidogrel in combination with acetylsalicylic acid, but there were no differences in the incidence of non-CNS thromboembolism or vascular death. In addition, taking clopidogrel in combination with acetylsalicylic acid reduced the total number of days of hospitalization for cardiovascular reasons.
Pharmacokinetics
Suction
After a single dose and during a course of oral administration at a dose of 75 mg/day, clopidogrel is rapidly absorbed. The average maximum plasma concentration (Cmax) of unchanged clopidogrel is about 2.2-2.5 ng/ml and is reached approximately 45 minutes after administration. According to the excretion of clopidogrel metabolites by the kidneys, its absorption is at least 50%.
Distribution
In vitro, clopidogrel and its main circulating inactive metabolite are reversibly bound to plasma proteins by 98% and 94%, respectively. In vitro, this bond is unsaturable over a wide range of concentrations.
Metabolism
Clopidogrel is extensively metabolized in the liver. In vitro and in vivo, clopidogrel is metabolized in two ways: the first – through esterases and subsequent hydrolysis with the formation of an inactive carboxylic acid derivative (85%) from metabolites circulating in the systemic circulation, and the second way – through the cytochrome P450 system. Initially, clopidogrel is metabolized to 2-oxoclopidogrel, which is an intermediate metabolite. Subsequent metabolism
2-oxoclopidogrel leads to the formation of an active metabolite of clopidogrel – a thiol derivative of clopidogrel. In vitro, this metabolic pathway occurs with the participation of the isoenzymes CYP3A4, CYP2C19, CYP1A2 and CYP2B6. The active thiol metabolite of clopidogrel, which was isolated in in vitro studies, rapidly and irreversibly binds to platelet receptors, thereby inhibiting platelet aggregation.
With a single dose of clopidogrel at a loading dose of 300 mg, the Cmax of the active metabolite is 2 times higher than the Cmax when taking clopidogrel at a maintenance dose of 75 mg for 4 days. Cmax of the active metabolite is achieved 30-60 minutes after taking clopidogrel.
Removal
Within 120 hours after human ingestion of 14C-labeled clopidogrel, approximately 50% of the radioactivity is excreted through the kidneys and approximately 46% of the radioactivity through the intestines. After a single oral dose of 75 mg, the half-life (T1/2) of clopidogrel is about 6 hours. After a single dose and repeated doses, T1/2 of the main inactive metabolite circulating in the blood is 8 hours.
Pharmacogenetics
With the help of the CYP2C19 isoenzyme, both the active metabolite and the intermediate metabolite – 2-oxoclopidogrel – are formed. The pharmacokinetics and antiplatelet effect of the active metabolite of clopidogrel, when studying platelet aggregation ex vivo, vary depending on the genotype of the CYP2C19 isoenzyme.
The allele of the CYP2C19*1 gene corresponds to a fully functional metabolism, while the alleles of the CYP2C19*2 and CYP2C19*3 genes are non-functional. Alleles of the CYP2C19*2 and CYP2C19*3 genes are the cause of decreased metabolism in the majority of representatives of the Caucasian (85%) and Mongoloid races (99%). Other alleles associated with absent or decreased metabolism are less common and include, but are not limited to, the CYP2C19*4, *5, *6, *7, and *8 alleles. Patients who are poor metabolizers must have the two loss-of-function gene alleles listed above. Published frequencies of CYP2C19 poor metabolizer phenotypes are 2% in Caucasians, 4% in Blacks, and 14% in Chinese.
In a crossover study conducted on 40 volunteers, 10 people in each group with four subtypes of the CYP2C19 isoenzyme (ultra-rapid metabolizers, extensive metabolizers, intermediate metabolizers, poor metabolizers), the pharmacokinetics and antiplatelet effect were assessed when taking clopidogrel at a dose of 300 mg, followed by 75 mg/day and at taking clopidogrel at a dose of 600 mg followed by 150 mg/day for 5 days (reaching an equilibrium state). There were no significant differences in active metabolite exposure and mean platelet aggregation inhibition (API) (ADP-induced) values between ultrarapid, extensive, and intermediate metabolizers. In poor metabolizers, exposure to the active metabolite was reduced by 63-71% compared to extensive metabolizers. When using the 300 mg/75 mg treatment regimen in poor metabolizers, the antiplatelet effect was reduced with mean IAT values of 24% (at 24 hours) and 37% (at 5 days of treatment) compared with IATs of 39% (at 24 hours) and 58% (at 5 days of treatment) in extensive metabolizers and 37% (at 24 h) and 60% (on the 5th day of treatment) in intermediate metabolizers. When poor metabolizers received the 600 mg/150 mg regimen, exposure to the active metabolite was higher than when receiving the 300 mg/75 mg regimen. In addition, the IAT was 32% (at 24 hours) and 61% (at day 5 of treatment), which was greater than that in poor metabolizers receiving the 300 mg/75 mg treatment regimen and was similar to that in the groups of patients with higher intensity of CYP2C19 metabolism receiving the 300 mg/75 mg treatment regimen. However, clinical outcome studies have not yet established a clopidogrel dosing regimen for patients in this group.
Consistent with the results of this study, a meta-analysis of six studies that included data from 335 volunteers treated with clopidogrel at steady state found that intermediate metabolizers had a 28% reduction in active metabolite exposure and poor metabolizers had a 72% reduction in exposure to the active metabolite, although IAT was reduced compared with extensive metabolizers with differences in IAT of 5.9% and 21.4%, respectively.
The effect of CYP2C19 genotype on clinical outcomes in patients treated with clopidogrel has not been assessed in prospective, randomized, controlled studies. However, few retrospective analyzes are currently available. Genotyping results are available from the following clinical studies: CURE (n=2721), CHARISMA (n=2428), CLARITY-TIMI 28 (n=227), TRITON-TIMI 38 (n=1477) and ACTIVE-A (n=601), as well as several published cohort studies.
In the TRITON-TIMI 38 study and 3 cohort studies (Collet, Sibbing, Giusti), patients in the combination group who were intermediate or poor metabolizers had a higher incidence of cardiovascular events (death, myocardial infarction, and stroke) or stent thrombosis compared with those of extensive metabolizers.
In the CHARISMA study and one cohort study (Simon), an increase in the incidence of cardiovascular events was observed only in poor metabolizers (when compared with extensive metabolizers).
In the CURE, CLARITY, ACTIVE-A and one of the cohort studies (Trenk), there was no increase in the incidence of cardiovascular events depending on the intensity of CYP2C19 metabolism.
Clinical studies conducted to date have not had a sufficient sample size to detect differences in clinical outcome in patients with low CYP2C19 activity.
Pharmacokinetics in special clinical situations
The pharmacokinetics of the active metabolite of clopidogrel in certain groups of patients has not been studied.
In elderly volunteers (over 75 years of age), when compared with young volunteers, there were no differences in platelet aggregation and bleeding time. No dose adjustment is required in elderly patients.
The pharmacokinetics of clopidogrel in children has not been studied.
In patients with severe renal impairment (creatinine clearance (CR) 5-15 ml/min), after repeated doses of clopidogrel 75 mg/day, the initiation of ADP-induced platelet aggregation was lower (25%) compared with that in healthy volunteers, but the prolongation of bleeding time was similar to that in healthy volunteers receiving clopidogrel 75 mg/day. Clopidogrel was well tolerated in all patients.
In patients with severe liver damage, after daily administration of clopidogrel 75 mg/day for 10 days, the inhibition of ADP-induced platelet aggregation was similar to that in healthy volunteers. The mean bleeding time was also comparable in both groups.
The prevalence of alleles of the CYP2C9 isoenzyme genes responsible for intermediate and reduced metabolism differs among representatives of different racial groups. There are very few literary data among representatives of the Mongoloid race, which does not allow us to assess the significance of genotyping the CYP2C19 isoenzyme for the development of ischemic complications.
Special instructions
Special instructions
Bleeding and hematological disorders
Due to the risk of bleeding and hematological undesirable effects (see section Side effects), if clinical symptoms suspicious for bleeding appear during treatment, you should urgently do a clinical blood test, determine the activated partial thromboplastin time (aPTT), platelet count, indicators of platelet functional activity and conduct other necessary studies.
Clopidogrel, like other antiplatelet drugs, should be used with caution in patients who have an increased risk of bleeding associated with trauma, surgery or other pathological conditions, as well as in patients receiving acetylsalicylic acid, other NSAIDs, including COX-2 inhibitors, heparin, SSRIs or glycoprotein IIb/IIIa inhibitors.
During treatment with clopidogrel, especially during the first weeks of treatment and/or after invasive cardiac procedures/surgery, patients should be closely monitored for signs of bleeding, including occult bleeding.
The combined use of clopidogrel with warfarin may increase the intensity of bleeding (see section Interactions with other drugs), therefore, with the exception of special rare clinical situations (such as the presence of a floating thrombus in the left ventricle, stenting in patients with atrial fibrillation), the combined use of clopidogrel and warfarin is not recommended.
If the patient is undergoing elective surgery and there is no need for an antiplatelet effect, clopidogrel should be discontinued 7 days before surgery.
Before any upcoming surgery and before starting any new drug, patients should tell their doctor (including their dentist) that they are taking clopidogrel.
Clopidogrel prolongs bleeding time and should be used with caution in patients with diseases predisposing to the development of bleeding (especially gastrointestinal and intraocular).
Patients should be warned that it may take longer to stop bleeding when taking clopidogrel (alone or in combination with acetylsalicylic acid), and that if they experience unusual bleeding (in location or duration) they should inform their doctor.
Thrombotic thrombocytopenic purpura
Very rarely, after the use of clopidogrel (sometimes even for a short period), cases of the development of TTP, which is characterized by thrombocytopenia and microangiopathic hemolytic anemia, accompanied by neurological disorders, renal dysfunction and fever, have been reported. TTP is a potentially life-threatening condition that requires immediate treatment, including plasmapheresis.
Acquired hemophilia
Acquired hemophilia has been reported with the use of clopidogrel. If a prolongation of the aPTT with or without the development of bleeding is confirmed, the presence of acquired hemophilia should be questioned. If acquired hemophilia is diagnosed, appropriate treatment should be initiated and clopidogrel should be discontinued.
Recent ischemic stroke
Taking Lopirel is not recommended for acute ischemic stroke less than 7 days old (as there is no data on its use in this condition).
In patients with recent ischemic stroke or transient ischemic attack and a high risk of recurrent atherothrombotic events, combination therapy with clopidogrel and acetylsalicylic acid has not been shown to be superior to clopidogrel monotherapy, but may increase the risk of major bleeding.
Cytochrome P450 isoenzyme CYP2C19
Pharmacogenetics: In patients with a slow metabolism of the CYP2C19 isoenzyme, when taking clopidogrel in recommended doses, the active metabolite of clopidogrel is formed in smaller quantities and a weaker effect on platelet aggregation is observed. Tests are available to determine the CYP2C19 genotype in patients.
Since clopidogrel is metabolized to active metabolites partly with the participation of the CYP2C19 isoenzyme, the use of drugs that inhibit the activity of this enzyme will lead to a decrease in the concentration of the active metabolite of clopidogrel. The clinical significance of this interaction is unknown. As a precautionary measure, simultaneous use of strong and moderate inhibitors of the CYP2C19 isoenzyme is not recommended (see the Interactions with other drugs section for clarification of drugs and the Pharmacokinetics section).
Cross-reactions with thienopyridines
Since hypersensitivity cross-reactions have been reported during treatment with thienopyridines, before starting treatment, it is necessary to clarify the patient’s history of hypersensitivity reactions to thienopyridines (clopidogrel, ticlopidine, prasugrel) (see section Side effects).
Thienopyridines may cause allergic reactions of varying severity, such as rash, angioedema or hematological cross-reactions (thrombocytopenia and neutropenia). Patients who have experienced allergic reactions and/or hematological reactions during previous treatment with one of the thienopyridines may be at increased risk of developing similar or other reactions when taking another thienopyridine. Monitoring for hypersensitivity symptoms is recommended in patients with a history of allergic reactions to thienopyridines.
Renal dysfunction
Experience with the use of clopidogrel in patients with impaired renal function is limited, so it should be used with caution in this group of patients (see Dosage and Administration).
Liver dysfunction
Experience in patients with moderate liver dysfunction who are at risk of developing hemorrhagic diathesis is limited. The drug Lopirel should be used with caution in this group of patients (see section Dosage and Administration).
Lactose content in the preparation
Lopirel should not be taken by patients with rare hereditary galactose intolerance, lactase deficiency and glucose-galactose malabsorption syndrome (see section Contraindications).
Impact on the ability to drive vehicles and machinery
Clopidogrel does not have a significant effect on the abilities required to drive a car or operate machinery.
Active ingredient
Active ingredient
Clopidogrel
Composition
Composition
Active ingredient:
clopidogrel hydrogen sulfate 97.87 mg, corresponding to 75 mg clopidogrel base;
Excipients:
lactose,
microcrystalline cellulose,
crospovidone (type A),
glyceryl dibehenate,
talc,
Opadry II 85 G34669 pink (polyvinyl alcohol, talc, titanium dioxide (E171),
macrogol 3350,
lecithin (E322),
iron oxide red dye (E172))
Pregnancy
Pregnancy
Pregnancy
As a precautionary measure, the use of Lopirel during pregnancy is contraindicated due to the lack of clinical data on its use by pregnant women, although animal studies of clopidogrel have not revealed any direct or indirect adverse effects on pregnancy, embryonic development, childbirth and postnatal development.
Breastfeeding period
Breastfeeding should be discontinued during treatment with Lopirel, since studies in rats have shown that clopidogrel and/or its metabolites are excreted into breast milk. It is unknown whether clopidogrel passes into human breast milk.
Contraindications
Contraindications
hypersensitivity to clopidogrel or any excipient of the drug;
severe liver failure;
acute bleeding, such as bleeding from a peptic ulcer or intracranial hemorrhage;
rare hereditary lactose intolerance, lactase deficiency and glucose-galactose malabsorption syndrome;
pregnancy and lactation;
children under 18 years of age (safety and effectiveness of use have not been established).
With caution
with moderate liver failure, in which there may be a predisposition to bleeding (limited clinical experience);
for renal failure (limited clinical experience);
in case of injuries, surgical interventions (risk of increased bleeding);
for diseases in which there is a predisposition to the development of bleeding (especially gastrointestinal or intraocular);
with simultaneous administration of serotonin reuptake inhibitors (SSRIs);
while taking non-steroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors;
with simultaneous administration of warfarin, heparin, glycoprotein IIb/IIIa inhibitors;
when there is a history of allergic and hematological reactions to other thienopyridines (such as ticlopidine, prasugrel) due to the possibility of cross-allergic and hematological reactions (see section “Special instructions”);
in patients with a genetically determined decrease in the function of the CYP2C19 isoenzyme (in patients who are weak CYP2C19 metabolizers, when clopidogrel is used in recommended doses, less of the active metabolite of clopidogrel is formed and its antiplatelet effect is less pronounced; weak metabolizers receiving clopidogrel in recommended doses, with acute coronary syndrome or percutaneous coronary artery disease intervention may have a higher incidence of cardiovascular complications than patients with normal CYP2C19 function).
Side Effects
Side Effects
The safety of clopidogrel was studied in more than 44,000 patients, including more than 12,000 patients treated for a year or longer. The overall tolerability of clopidogrel was similar to that of acetylsalicylic acid, regardless of patient age, gender, and race. The following are clinically significant adverse effects observed in clinical trials: CAPRIE, CURE, CLARITY, COMMIT and ACTIVE A. The tolerability of clopidogrel at a dose of 75 mg/day in the CAPRIE trial was consistent with the tolerability of acetylsalicylic acid at a dose of 325 mg/day. This included reports of adverse reactions in spontaneous reports.
Most often in clinical studies, as well as during post-marketing use of clopidogrel, bleeding was reported, most of which developed in the first month of treatment.
In the CAPRIE clinical trial, the overall bleeding rate in patients receiving clopidogrel or acetylsalicylic acid was 9.3%. The incidence of severe bleeding with clopidogrel was similar to that with acetylsalicylic acid.
In the CURE clinical trial, there was no increase in the incidence of major bleeding when clopidogrel with acetylsalicylic acid was used within seven days after coronary artery bypass surgery in patients who stopped therapy more than 5 days before surgery. In patients who continued therapy for five days before the start of coronary artery bypass surgery, the incidence of this event was 9.6% for the combination of clopidogrel with acetylsalicylic acid and 6.3% for placebo in combination with acetylsalicylic acid.
In the CLARITY clinical trial, an overall increase in the incidence of bleeding was observed in the clopidogrel + acetylsalicylic acid group compared with the placebo + acetylsalicylic acid group. The incidence of major bleeding was similar in both groups and was practically independent of the initial characteristics of the patients and the type of fibrinolytic or heparin therapy.
In the COMMIT clinical trial, the overall incidence of noncerebral major bleeding or cerebral hemorrhage was low and did not differ significantly between the two groups.
In the ACTIVE-A clinical trial, the incidence of major bleeding in the clopidogrel + acetylsalicylic acid group was higher than in the placebo + acetylsalicylic acid group (6.7% versus 4.3%). Major bleeding was mainly extracranial in both groups (5.3% vs 3.5%), and gastrointestinal bleeding was mainly observed (3.5% vs 1.8%). There were more intracranial hemorrhages in the clopidogrel + acetylsalicylic acid group compared to the placebo + acetylsalicylic acid group (1.4% versus 0.8%, respectively). There were no statistically significant differences between these treatment groups in the incidence of fatal bleeding (1.1% vs. 0.7%) and hemorrhagic stroke (0.8% vs. 0.6%).
The following are adverse reactions that were observed in clinical studies or spontaneously reported. The frequency of reactions is presented according to the following classification: very often (≥1/10); often (≥1/100, <1/10); uncommon (>1/1000, <1/100); rare (≥1/10,000, <1/1000); very rare (< 1/10,000), frequency unknown (cannot be determined from available data). In each of the subgroups according to the classification of organs and organ systems, adverse reactions are presented in order of decreasing severity.
From the blood and lymphatic system: infrequently – thrombocytopenia, leukopenia, eosinophilia; rarely – neutropenia, including severe neutropenia; very rarely – thrombotic thrombocytopenic purpura (TTP) (see section Special instructions), aplastic anemia, pancytopenia, agranulocytosis, severe thrombocytopenia, acquired hemophilia type A, granulocytopenia, anemia.
From the heart: frequency unknown – Kounis syndrome (vasospastic allergic angina / allergic myocardial infarction) in the context of a hypersensitivity reaction caused by clopidogrel.
From the immune system: very rarely – serum sickness, anaphylactoid reactions; frequency unknown – hypersensitivity cross-reactions with thienopyridines (such as ticlopidine, prasugrel) (see section Special instructions).
Mental disorders: very rarely – hallucinations, confusion.
From the nervous system: infrequently – intracranial hemorrhage (some cases were fatal), headache, paresthesia, dizziness; very rarely – taste disturbance, ageusia.
From the organ of vision: infrequently – ocular hemorrhages (in the conjunctiva, in the tissue of the eye, the retina).
From the organ of hearing and labyrinthine disorders: rarely – vertigo.
From the blood vessels: often – hematomas, very rarely – severe bleeding, bleeding from surgical wounds, vasculitis, decreased blood pressure.
From the respiratory system, chest and mediastinal organs: often – nosebleeds; very rarely – bleeding from the respiratory system (hemoptysis, pulmonary hemorrhage), bronchospasm, intestinal pneumonitis, eosinophilic pneumonia.
From the gastrointestinal tract: often – bleeding of the gastrointestinal tract, diarrhea, abdominal pain, dyspepsia; uncommon – gastric and duodenal ulcers, gastritis, vomiting, nausea, constipation, flatulence; rarely – retroperitoneal bleeding; very rarely – gastrointestinal and retroperitoneal bleeding with a fatal outcome, pancreatitis, colitis (including ulcerative or lymphocytic), stomatitis.
From the liver and biliary tract: very rarely – acute liver failure, hepatitis, abnormalities in laboratory tests of the functional state of the liver.
From the skin and subcutaneous tissues: often – bruising; uncommon – rash, itchy skin, purpura (spotty capillary hemorrhages into the skin, under the skin or into mucous membranes); very rarely – bullous dermatitis (toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme, acute generalized exanthematous pustulosis (AGEP)), angioedema, drug hypersensitivity syndrome, drug rash with eosinophilia and systemic symptoms (DRESS syndrome), erythematous or exfoliative rash, urticaria, eczema, lichen planus.
From the musculoskeletal and connective tissue: very rarely – hemorrhages in the musculoskeletal system (hemarthrosis), arthritis, arthralgia, myalgia.
From the kidneys and urinary tract: infrequently – hematuria; very rarely – glomerulonephritis, increased creatinine concentration in the blood.
Disorders of the genital organs and breast: rarely – gynecomastia.
General disorders and disorders at the injection site: often – bleeding from the puncture site; very rarely – fever.
Laboratory and instrumental data: infrequently – prolongation of bleeding time, decrease in the number of neutrophils, decrease in the number of platelets.
Interaction
Interaction
Indirect anticoagulants: simultaneous use of clopidogrel and indirect anticoagulants is not recommended due to a possible increase in bleeding intensity (see section Special instructions). Although clopidogrel 75 mg/day did not affect the pharmacokinetics of S-warfarin or the international normalized ratio in patients receiving long-term warfarin therapy, concomitant use of clopidogrel with warfarin increases the risk of bleeding due to an independent effect on hemostasis.
IIb/IIIa receptor blockers: the administration of IIb/IIIa receptor blockers together with clopidogrel requires caution (see section Special instructions).
Acetylsalicylic acid does not change the effect of clopidogrel, which inhibits ADP-induced platelet aggregation, but clopidogrel potentiates the effect of acetylsalicylic acid on collagen-induced platelet aggregation. However, concomitant administration of acetylsalicylic acid with clopidogrel at a dose of 500 mg 2 times a day for 1 day did not cause a significant increase in the bleeding time caused by taking clopidogrel. There may be a pharmacodynamic interaction between clopidogrel and acetylsalicylic acid, which leads to an increased risk of bleeding. Therefore, caution should be exercised when using them simultaneously (see Special Instructions), although in clinical studies patients received combination therapy with clopidogrel and acetylsalicylic acid for up to one year.
Heparin: According to a clinical trial conducted in healthy subjects, clopidogrel did not require a change in the dose of heparin and did not alter its anticoagulant effect. Concomitant use of heparin did not change the antiplatelet effect of clopidogrel. There may be a pharmacodynamic interaction between clopidogrel and heparin, which may increase the risk of bleeding, so the simultaneous use of these drugs requires caution (see section Special instructions).
Thrombolytics: The safety of concomitant use of clopidogrel, fibrin-specific or non-fibrin-specific thrombolytic drugs and heparin has been studied in patients with acute myocardial infarction. The frequency of clinically significant bleeding was similar to that observed in the case of combined use of thrombolytic agents and heparin with acetylsalicylic acid (see section Side effects).
NSAIDs: In a clinical study in healthy volunteers, coadministration of clopidogrel and naproxen increased occult gastrointestinal blood loss. However, due to the lack of interaction studies between clopidogrel and other NSAIDs, it is currently unknown whether there is an increased risk of gastrointestinal bleeding when clopidogrel is taken with other NSAIDs. Therefore, the prescription of NSAIDs, including COX-2 inhibitors, in combination with clopidogrel should be done with caution (see section Special instructions).
Selective serotonin reuptake inhibitors (SSRIs): Because SSRIs affect platelet activation and increase the risk of bleeding, caution should be exercised when taking them concomitantly with clopidogrel.
Other combination therapy. Since clopidogrel is metabolized to the formation of its active metabolite in part by the CYP2C19 system, the use of drugs that inhibit this system may lead to a decrease in the concentration of the active metabolite of clopidogrel in the blood plasma and a decrease in its clinical effectiveness. The clinical significance of this interaction is unknown. As a precaution, simultaneous use of strong and moderate inhibitors of the CYP2C19 isoenzyme should be avoided (see section Special instructions and Pharmacokinetics).
Medicines that inhibit CYP2C19 include omeprazole and esomeprazole, fluvoxamine, fluoxetine, moclobemide, voriconazole, fluconazole, ticlopidine, ciprofloxacin, cimetidine, carbamazepine, oxcarbamazepine and chloramphenicol.
Overdose
Overdose
Symptoms: an overdose of clopidogrel can lead to an increase in bleeding time with subsequent complications in the form of bleeding.
Treatment: when bleeding occurs, appropriate treatment measures are required. If rapid correction of prolonged bleeding time is necessary, platelet transfusion is recommended. An antidote for clopidogrel has not been established.
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C. Keep out of the reach of children!
Shelf life
Shelf life
3 years. Do not use after expiration date.
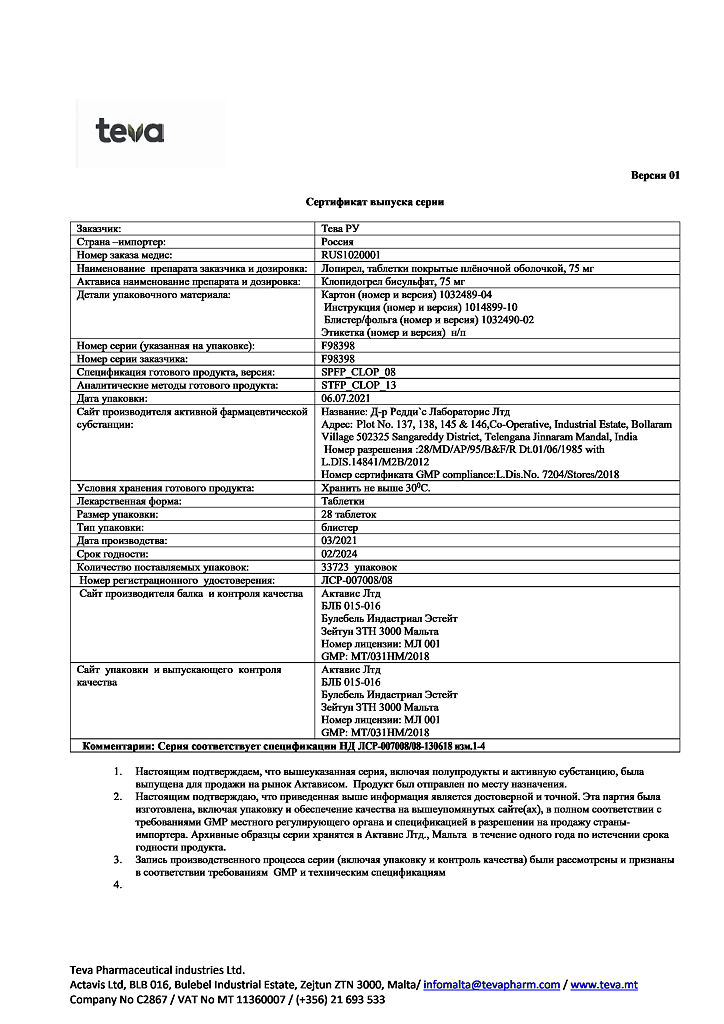
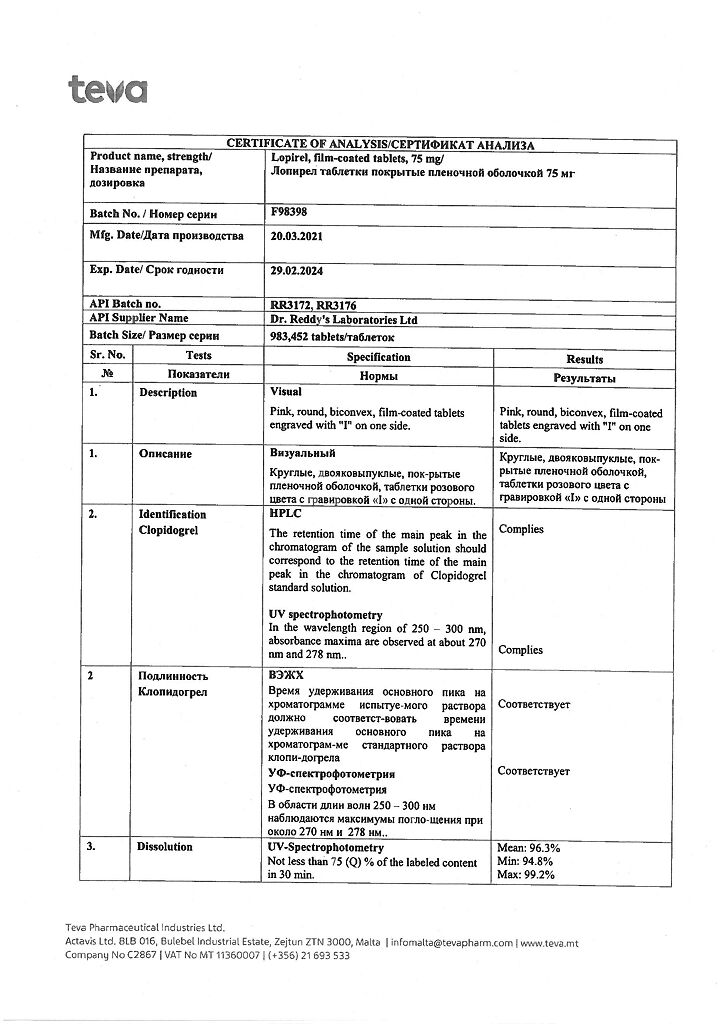
Manufacturer
Manufacturer
Actavis Ltd, Malta
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 ° C. Keep out of reach of children! |
| Manufacturer | Actavis Ltd, Malta |
| Medication form | pills |
| Brand | Actavis Ltd |
Related products
Buy Lopirel, 75 mg 28 pcs. with delivery to USA, UK, Europe and over 120 other countries.