No products in the cart.
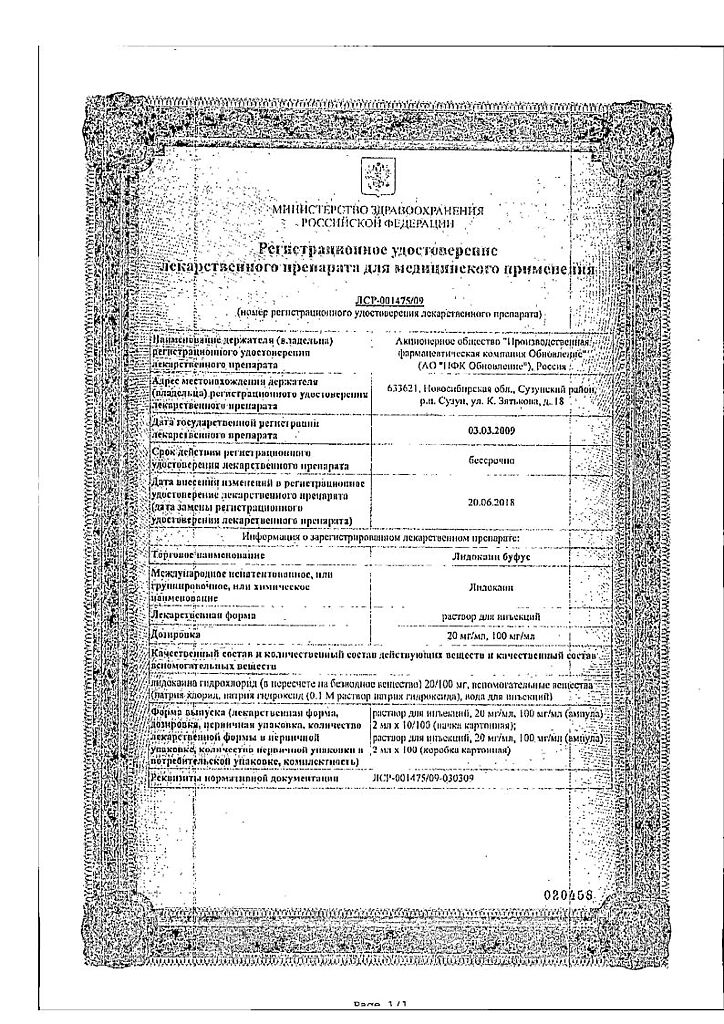
Lidocaine bufus, 100 mg/ml 2 ml 10 pcs
€4.42 €3.93
Description
It has antiarrhythmic (class Ib) action. Stabilizes cell membranes, blocks sodium channels, increases membrane permeability to potassium ions.
With almost no effect on the electrophysiological state of the atria, lidocaine accelerates repolarization in the ventricles, inhibits phase IV depolarization in Purkinje fibers (especially in ischemic myocardium), reducing their automaticity and duration of action potential, increases the minimum potential difference at which myofibrils respond to premature stimulation.
Shortens the duration of the action potential and the effective refractory period. It has no significant effect on myocardial conduction and contractility (suppression of conduction is observed only when administered in large doses, close to toxic) – the duration of intervals PQ , QT and the width of the QRS complex on the electrocardiogram does not change. Negative inotropic effect is also expressed insignificantly and appears transiently only when administered in high doses.
Pharmacokinetics
Absorption
The main factor determining the absorption rate and concentration in the blood is the total dose administered, regardless of the site of administration. There is a linear relationship between the amount of lidocaine administered and the resulting maximum concentration of the drug in the blood.
Distribution
Lidocaine binds to plasma proteins, including α1-acid glycoprotein (ACG) and albumin. The degree of binding is variable and is approximately 66%. Plasma concentration of AKG in newborns is low, so they have relatively high content of free bioactive fraction of lidocaine.
Lidocaine penetrates through the blood-brain and placental barriers, probably by passive diffusion.
Metabolism
Lidocaine is metabolized in the liver, with about 90% of the administered dose undergoing N-dealkylation to form monoethylglycincylidide (MEGX) and glycincylidide (GX), both contributing to the therapeutic and toxic effects of lidocaine. The pharmacological and toxic effects of MEGX and GX are comparable to those of lidocaine, but are weaker. GX has a longer half-life than lidocaine (about 10 hours) and may cumulate with repeated administration.
Metabolites resulting from subsequent metabolism are excreted with urine, the content of unchanged lidocaine in urine does not exceed 10%.
Excretion
The terminal elimination half-life of lidocaine after intravenous bolus injection in healthy adult volunteers is 1-2 hours. The terminal half-life of GX is approximately 10 hours, MEGX 2 hours.
Special patient groups
Due to rapid metabolism, the pharmacokinetics of lidocaine may be affected by conditions that impair hepatic function. In patients with hepatic dysfunction, the elimination half-life of lidocaine may increase two or more times.
Impaired renal function does not affect the pharmacokinetics of lidocaine, but may lead to cumulation of its metabolites.
Newborns have a low concentration of ACG, so binding to plasma proteins may be reduced. Due to the potentially high concentration of the free fraction, the use of lidocaine in neonates is not recommended.
Indications
Indications
Relief of persistent paroxysms of ventricular tachycardia, including during myocardial infarction and cardiac surgery. Prevention of repeated ventricular fibrillation in acute coronary syndrome and repeated paroxysms of ventricular tachycardia (usually within 12-24 hours).
Ventricular arrhythmias caused by glycoside intoxication.
Pharmacological effect
Pharmacological effect
Has antiarrhythmic (class Ib) effect. Stabilizes cell membranes, blocks sodium channels, increases membrane permeability for potassium ions.
With virtually no effect on the electrophysiological state of the atria, lidocaine accelerates repolarization in the ventricles, inhibits phase IV depolarization in Purkinje fibers (especially ischemic myocardium), reducing their automaticity and the duration of the action potential, and increases the minimum potential difference at which myofibrils respond to premature stimulation.
Shortens the duration of the action potential and the effective refractory period. It does not have a significant effect on the conductivity and contractility of the myocardium (inhibition of conductivity is noted when administered only in large, close to toxic doses) – the duration of the PQ, QT intervals and the width of the QRS complex does not change on the electrocardiogram. The negative inotropic effect is also slightly expressed and appears short-term only with rapid administration of the drug in large doses.
Pharmacokinetics
Absorption
The main factor determining the rate of absorption and concentration in the blood is the total dose administered, regardless of the site of administration. There is a linear relationship between the amount of lidocaine administered and the resulting maximum concentration of the drug in the blood.
Distribution
Lidocaine binds to plasma proteins, including α1-acid glycoprotein (ACG) and albumin. The degree of binding is variable, approximately 66%. The plasma concentration of ACH in newborns is low, so they have a relatively high content of the free biologically active fraction of lidocaine.
Lidocaine penetrates the blood-brain and placental barriers, probably through passive diffusion.
Metabolism
Lidocaine is metabolized in the liver, with approximately 90% of the administered dose undergoing N-dealkylation to form monoethylglycine xylidide (MEGX) and glycine xylidide (GX), both of which contribute to the therapeutic and toxic effects of lidocaine. The pharmacological and toxic effects of MEGX and GX are comparable to those of lidocaine, but less pronounced. GX has a longer half-life than lidocaine (approximately 10 hours) and may accumulate with repeated administration.
Metabolites formed as a result of subsequent metabolism are excreted in the urine; the content of unchanged lidocaine in the urine does not exceed 10%.
Removal
The terminal half-life of lidocaine after intravenous bolus administration to healthy adult volunteers is 1-2 hours. The terminal half-life of GX is approximately 10 hours, MEGX is 2 hours.
Special patient groups
Due to its rapid metabolism, the pharmacokinetics of lidocaine may be influenced by conditions that impair liver function. In patients with hepatic dysfunction, the half-life of lidocaine may increase by 2 times or more.
Impaired renal function does not affect the pharmacokinetics of lidocaine, but may lead to the accumulation of its metabolites.
In newborns, the concentration of AKG is low, so the connection with plasma proteins may be reduced. Due to the potentially high concentration of the free fraction, the use of lidocaine in newborns is not recommended.
Special instructions
Special instructions
Lidocaine should be used with caution in patients with myasthenia gravis, epilepsy, chronic heart failure, bradycardia and respiratory depression, as well as in combination with drugs that interact with lidocaine and lead to increased bioavailability, potentiation of effects (for example, phenytoin) or prolongation of elimination (for example, in hepatic or end-stage renal failure, in which metabolites may accumulate lidocaine).
Patients receiving class III antiarrhythmic drugs (eg, amiodarone) should be closely monitored and ECG monitored as the effects on the heart may be potentiated.
Lidocaine has been shown to cause porphyria in animals and should be avoided in persons with porphyria.
When administered into inflammatory or infected tissues, the effect of lidocaine may be reduced.
Before starting intravenous lidocaine, it is necessary to eliminate hypokalemia, hypoxia and acid-base imbalance.
Lidocaine injection solution is not recommended for use in newborns. The optimal serum concentration of lidocaine to avoid toxicities such as seizures and arrhythmias has not been established in neonates.
The influence of a medicinal product for medical use on the ability to drive vehicles and machinery
Depending on the dose and route of administration, lidocaine may have a temporary effect on motor ability and coordination. During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Lidocaine
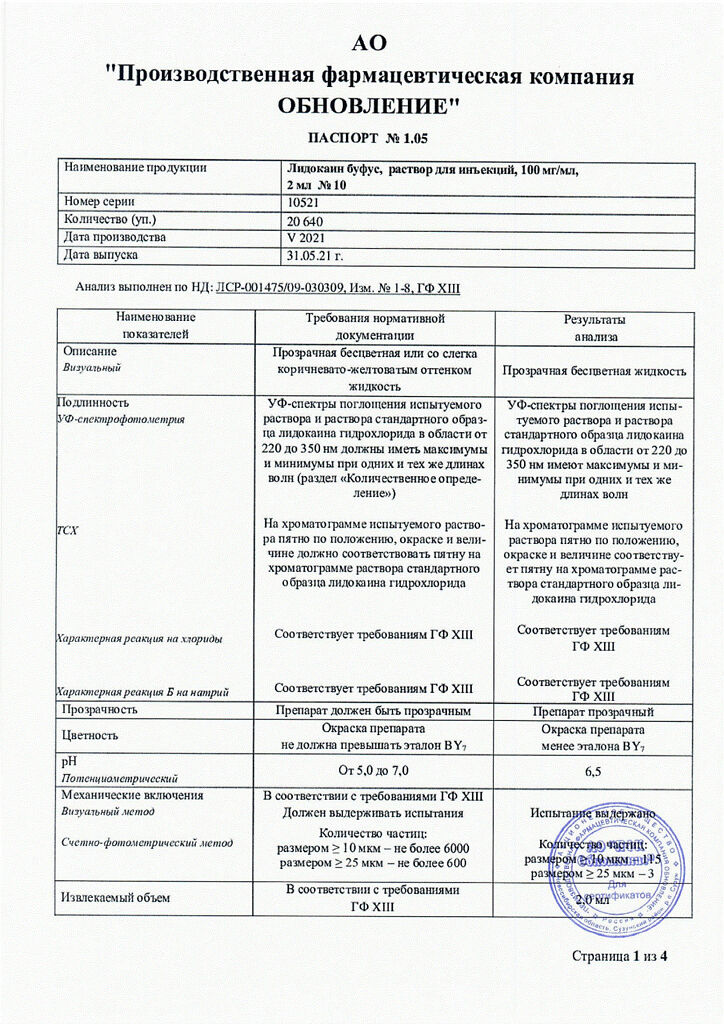
Composition
Composition
Active ingredient:
Lidocaine hydrochloride
(in terms of anhydrous substance) – 100 mg
Excipients:
sodium chloride − 6 mg
sodium hydroxide
(0.1 M sodium hydroxide solution) – up to pH 5.0-7.0
water for injection – up to 1 ml
Pregnancy
Pregnancy
Fertility
There are no data on the effect of lidocaine on human fertility.
Pregnancy
Use is possible if the expected benefit to the mother outweighs the potential risk to the fetus and child.
Breastfeeding
Lidocaine passes into breast milk in small quantities and its oral bioavailability is very low. Thus, the expected amount obtained through breast milk is very small, therefore the potential harm to the baby is very low. The decision about the possibility of using lidocaine during breastfeeding is made by the doctor.
Contraindications
Contraindications
Hypersensitivity to the components of the drug; sick sinus syndrome, severe bradycardia (heart rate less than 50 beats per minute), atrioventricular (AV) block II and III degrees (if an artificial pacemaker is not installed), sinoatrial block, WPW (Wolf-Parkinson-White) syndrome, acute and chronic heart failure (III-IV functional class according to the NYHA classification), cardiogenic shock, disorders intraventricular conduction; severe arterial hypotension, Morgagni Adams-Stokes syndrome.
With caution
The administration of lidocaine should be carried out with caution in patients with myasthenia gravis, epilepsy, chronic heart failure II and III degrees, hypovolemia, atrioventricular block I degree, sinus bradycardia, severe hepatic and/or renal failure, coagulopathy, complete and incomplete block of intracardiac conduction, convulsive disorders, Melkerson-Rosenthal syndrome, porphyria, reduced hepatic blood flow, debilitated or elderly patients (over 65 years of age), children under 18 years of age (due to slow metabolism, accumulation of the drug is possible), as well as the third trimester of pregnancy.
Side Effects
Side Effects
Adverse reactions are described according to MedDRA system organ classes.
Immune system disorders
Hypersensitivity reactions (allergic or anaphylactoid reactions, anaphylactic shock) – see also skin and subcutaneous tissue disorders. The lidocaine skin allergy test is considered unreliable.
Nervous system and mental disorders
Neurological signs of systemic toxicity include dizziness, nervousness, tremor, paresthesia around the mouth, numbness of the tongue, somnolence, seizures, coma.
Reactions from the nervous system can be manifested by its excitation or depression. Signs of central nervous system stimulation may be short-lived or not occur at all, so the first signs of toxicity may be confusion and drowsiness, followed by coma and respiratory failure.
Visual disorders
Signs of lidocaine toxicity may include blurred vision, diplopia, and transient amaurosis.
Disorders of the hearing organ and labyrinth
Tinnitus, hyperacusis.
Cardiovascular system disorders
Cardiovascular reactions are manifested by arterial hypotension, bradycardia, inhibition of myocardial contractile function (negative inotropic effect), arrhythmias; Possible cardiac arrest or circulatory failure.
Disorders of the respiratory system, chest and mediastinal organs
Dyspnea, bronchospasm, respiratory depression, respiratory arrest.
Gastrointestinal disorders
Nausea, vomiting.
Disorders of the skin and subcutaneous tissues
Rash, urticaria, angioedema, facial swelling.
Interaction
Interaction
It is not advisable to combine lidocaine with the following drugs:
With beta-blockers due to increased toxic properties of lidocaine, with digitoxin – due to a weakening of the cardiotonic effect, with curare-like drugs – muscle relaxation increases.
It is irrational to prescribe lidocaine together with ajmaline, amiodarone, verapamil or quinidine due to increased cardiodepressive effects.
The combined use of lidocaine and procainamide can cause central nervous system stimulation and hallucinations.
With intravenous administration of hexenal or thiopental sodium against the background of the action of lidocaine, respiratory depression is possible.
Under the influence of MAO inhibitors, the local anesthetic effect of lidocaine is likely to be enhanced. Patients taking MAO inhibitors should not be prescribed parenteral lidocaine.
With the simultaneous administration of lidocaine and polymyxin-B, an increased inhibitory effect on neuromuscular transmission is possible, so in this case it is necessary to monitor the patient’s respiratory function.
With the simultaneous use of lidocaine with sleeping pills or sedatives, their inhibitory effect on the central nervous system may be enhanced. When lidocaine is administered intravenously to patients taking cimetidine, undesirable effects such as stunned state, drowsiness, bradycardia, parasthesia, etc. are possible. This is due to an increase in the level of lidocaine in the blood plasma, which is explained by the release of lidocaine from binding to blood proteins, as well as a slowdown in its inactivation in the liver. If combination therapy with these drugs is necessary, the dose of lidocaine should be reduced.
Pharmaceutical interaction
When used concomitantly, the following drugs increase the concentration of lidocaine in the blood serum: aminazine, cimetidine, propranolol, pethidine, bupivacaine, quinidine, disopyramide, amitriptyline, imipramine, nortriptyline.
Overdose
Overdose
Symptoms. Toxicity from the central nervous system is manifested by symptoms of increasing severity. Initially, paresthesia around the mouth, numbness of the tongue, dizziness, hyperacusis and tinnitus may develop. Visual disturbances and muscle tremors or muscle twitching indicate more serious toxicity and precede generalized seizures.
Loss of consciousness and grand mal seizures may then occur, lasting from a few seconds to several minutes. Convulsions lead to a rapid increase in hypoxia and hypercapnia, caused by increased muscle activity and respiratory failure. Apnea may develop. In severe cases, disorders of the cardiovascular system occur.
At high systemic concentrations, hypotension, bradycardia, arrhythmia and cardiac arrest may develop, which can be fatal.
Resolution of an overdose occurs due to the redistribution of the drug from the central nervous system and its metabolism; it can occur quite quickly (unless a very large dose of the drug was administered).
Treatment. If signs of overdose occur, administration of the drug should be stopped immediately.
Seizures, central nervous system depression, and cardiotoxicity require medical attention. The main goals of therapy are to maintain oxygenation, stop seizures, maintain circulation, and reverse acidosis (if it develops).
In appropriate cases, it is necessary to ensure airway patency and administer oxygen, as well as establish auxiliary ventilation (mask or using an Ambu bag). Blood circulation is maintained by infusion of plasma or infusion solutions. If long-term circulatory maintenance is necessary, vasopressors should be considered, but they increase the risk of central nervous system stimulation.
Control of seizures can be achieved by intravenous diazepam (0.1 mg/kg) or sodium thiopental (1-3 mg/kg), although it should be noted that anticonvulsants may also depress respiration and circulation. Prolonged seizures may interfere with the patient’s ventilation and oxygenation, and early endotracheal intubation should be considered. If the heart stops, standard cardiopulmonary resuscitation is started.
The effectiveness of dialysis in the treatment of acute lidocaine overdose is very low.
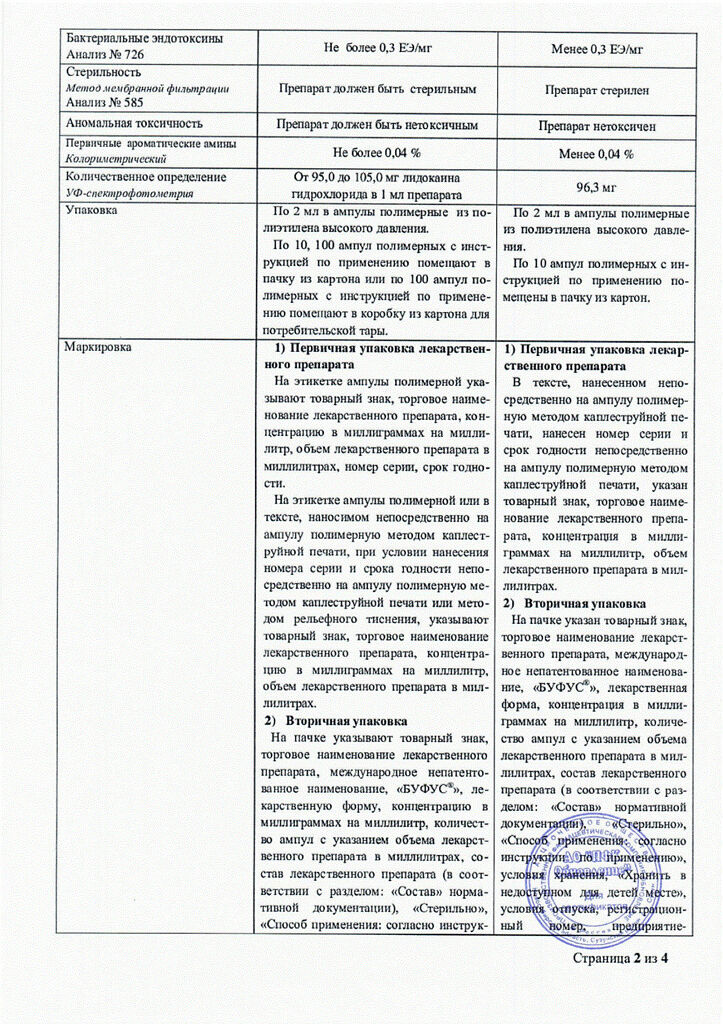
Storage conditions
Storage conditions
In a dry place, protected from light.
Shelf life
Shelf life
3 years.
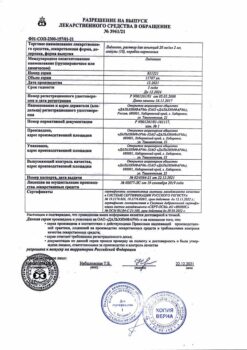
Manufacturer
Manufacturer
Update of PFC JSC, Russia
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | In a dry place protected from light. |
| Manufacturer | Update PFC AO, Russia |
| Medication form | solution for injection |
| Brand | Update PFC AO |
Other forms…
Related products
Buy Lidocaine bufus, 100 mg/ml 2 ml 10 pcs with delivery to USA, UK, Europe and over 120 other countries.