No products in the cart.
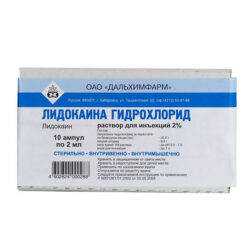
Lidocaine, 20 mg/ml 2 ml 10 pcs
€4.16 €3.69
EAN: 4680013242824
SKU: 280808
Categories: Anesthesia and resuscitation, Local anesthetics, Medicine
Description Pharmacotherapeutic group: Local anesthetic. Pharmacokinetics:
ATC:
N.01.B.B Amides
N.01.B.B.02 Lidocaine
C.01.B.B.01 Lidocaine
C.01.B.B Class Ib antiarrhythmic drugs
Pharmacodynamics:
Lidocaine is a short-acting local amide type anesthetic. Its mechanism of action is based on reduction of permeability of the neuron membrane for sodium ions. As a result, the rate of depolarization decreases and the excitation threshold increases, leading to reversible local numbness. Lidocaine is used to achieve conductive anesthesia in various parts of the body and to control arrhythmias. It has a rapid onset of action (about one minute after intravenous injection and fifteen minutes after intramuscular injection) and spreads quickly to surrounding tissues. The action lasts 10-20 minutes and about 60-90 minutes after intravenous and intramuscular injection, respectively.
Absorption
Lidocaine is rapidly absorbed from the gastrointestinal tract, but because of the “primary passage” effect through the liver, only a small amount reaches the systemic bloodstream.
The systemic absorption of lidocaine is determined by the site of administration, the dose and its pharmacological profile. The maximum concentration in the blood is achieved after intercostal blockade, then (in order of decreasing concentration), after administration to the lumbar epidural space, brachial plexus and subcutaneous tissues. The main factor determining the absorption rate and blood concentration is the total dose administered, regardless of the site of administration. There is a linear relationship between the amount of lidocaine administered and the resulting maximum blood concentration of the anesthetic.
Distribution
Lidocaine binds to plasma proteins, including α1-acid glycoprotein (AKT) and albumin. The degree of binding is variable, being approximately 66%. Plasma concentrations of AKT in newborns are low, so they have relatively high levels of the free bioactive fraction of lidocaine.
Lidocaine penetrates the blood-brain and placental barriers, probably by passive diffusion.
Metabolism
Lidocaine is metabolized in the liver, about 90% of the administered dose undergoes N-dealkylation to form monoethylglycincylidide (MEGX) and glycincylidide (GX), both contributing to the therapeutic and toxic effects of lidocaine. The pharmacological and toxic effects of MEGX and GX are comparable to those of lidocaine, but are weaker. GX has a longer half-life than lidocaine (about 10 hours) and may cumulate with repeated administration.
The metabolites produced by subsequent metabolism are excreted in the urine; the content of unchanged lidocaine in the urine is less than 10%.
The terminal elimination half-life of lidocaine after intravenous bolus administration in healthy adult volunteers is 1-2 hours. The terminal elimination half-life of GX is approximately 10 hours. MEGX is 2 hours.
Particular patient groups
Due to rapid metabolism, the pharmacokinetics of lidocaine may be affected by conditions that impair hepatic function. In patients with hepatic dysfunction, the elimination half-life of lidocaine may be increased by a factor of 2 or more.
Disordered renal function does not affect the pharmacokinetics of lidocaine, but may lead to cumulation of its metabolites.
In newborns, low ACT concentrations are noted, so binding to plasma proteins may be reduced. Because of the potentially high concentration of the free fraction, the use of lidocaine in neonates is not recommended.
.
Indications
Indications
Infiltration (including subconjunctival), conduction (including retrobulbar, parabulbar anesthesia), spinal and epidural anesthesia.
Relief of persistent paroxysms of ventricular tachycardia (including during myocardial infarction and cardiac surgery), prevention of repeated ventricular fibrillation in acute coronary syndrome and repeated paroxysms of ventricular tachycardia (usually within 12-24 hours), ventricular arrhythmias caused by glycoside intoxication (use a solution with a concentration of 100 mg/ml).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Local anesthetic.
ATX:
N.01.B.B Amides
N.01.B.B.02 Lidocaine
C.01.B.B.01 Lidocaine
C.01.B.B Class Ib antiarrhythmic drugs
Pharmacodynamics:
Lidocaine is a short-acting amide-type local anesthetic. Its mechanism of action is based on a decrease in the permeability of the neuron membrane to sodium ions. As a result, the rate of depolarization decreases and the excitation threshold increases, leading to reversible local numbness. Lidocaine is used to achieve conduction anesthesia in various parts of the body and control arrhythmias. It has a rapid onset of action (about one minute after intravenous administration and fifteen minutes after intramuscular administration), and quickly spreads into surrounding tissues. The action lasts 10-20 minutes and about 60-90 minutes after intravenous and intramuscular administration, respectively.
Pharmacokinetics:
Absorption
Lidocaine is rapidly absorbed from the gastrointestinal tract, but due to the first pass effect through the liver, only a small amount reaches the systemic circulation.
Systemic absorption of lidocaine is determined by the site of administration, dose and its pharmacological profile. The maximum concentration in the blood is achieved after intercostal blockade, then (in order of decreasing concentration), after injection into the lumbar epidural space, brachial plexus and subcutaneous tissue. The main factor determining the rate of absorption and concentration in the blood is the total dose administered, regardless of the site of administration. There is a linear relationship between the amount of lidocaine administered and the resulting maximum concentration of anesthetic in the blood.
Distribution
Lidocaine binds to plasma proteins, including α1-acid glycoprotein (AKT) and albumin. The degree of binding is variable, being approximately 66%. The plasma concentration of ACT in newborns is low, so they have a relatively high content of the free biologically active fraction of lidocaine.
Lidocaine penetrates the blood-brain and placental barriers, probably through passive diffusion.
Metabolism
Lidocaine is metabolized in the liver, with approximately 90% of the administered dose undergoing N-dealkylation to form monoethylglycine xylidide (MEGX) and glycine xylidide (GX), both of which contribute to the therapeutic and toxic effects of lidocaine. The pharmacological and toxic effects of MEGX and GX are comparable to those of lidocaine, but less pronounced. GX has a longer half-life than lidocaine (approximately 10 hours) and may accumulate with repeated administration.
Metabolites formed as a result of subsequent metabolism are excreted in the urine; the content of unchanged lidocaine in the urine does not exceed 10%.
Removal
The terminal half-life of lidocaine after intravenous bolus administration to healthy adult volunteers is 1-2 hours. The terminal half-life of GX is approximately 10 hours. MEGX – 2 hours.
Special patient groups
Due to its rapid metabolism, the pharmacokinetics of lidocaine may be influenced by conditions that impair liver function. In patients with hepatic dysfunction, the half-life of lidocaine may increase by 2 or more times.
Impaired renal function does not affect the pharmacokinetics of lidocaine, but may lead to the accumulation of its metabolites.
In newborns, ACT concentrations are low, so binding to plasma proteins may be reduced. Due to the potentially high concentration of the free fraction, the use of lidocaine in newborns is not recommended.
Special instructions
Special instructions
Prophylactic administration of the drug is not recommended for all patients with acute myocardial infarction without exception (routine prophylactic administration of lidocaine may increase the risk of death by increasing the incidence of asystole). If lidocaine is ineffective, it is necessary first to exclude hypokalemia; in emergency situations, there are several options for further action: carefully increasing the dose until side effects from the central nervous system appear (lethargy, difficulty speaking); prescription, sometimes combined, of class IA drugs (procainamide), transition to class III drugs (amioarone, bretylium tosylate).
It is necessary to discontinue monoamine oxidase inhibitors at least 10 days in case of planned use of lidocaine.
Caution should be exercised when performing local anesthesia in highly vascularized tissues; aspiration testing is recommended to avoid intravascular injection.
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Lidocaine
Composition
Composition
1 ml contains:
Active substances:
lidocaine hydrochloride (calculated as anhydrous substance) 20 mg
Excipients:
sodium chloride – 3 mg,
water for d/i – up to 1 ml.
Contraindications
Contraindications
sick sinus syndrome, severe bradycardia, atrioventricular block II-III degree (except when a probe is inserted to stimulate the ventricles), sinoatrial block, Wolff-Parkinson-White syndrome, acute and chronic heart failure (III-IV functional class), cardiogenic shock, Morgagni-Adams-Stokes syndrome, intraventricular conduction disorders; hypersensitivity to any of the components of the drug;
pregnancy, lactation period (penetrates the placental barrier, excreted in breast milk).
It is also necessary to take into account general contraindications to this or that type of anesthesia.
With caution: Chronic heart failure (functional class II), arterial hypotension, hypovolemia, first degree atrioventricular block, sinus bradycardia, severe hepatic and/or renal failure, myasthenia gravis, epileptiform seizures (including a history), reduced hepatic blood flow, frail or elderly patients (over 65 years of age), children under 18 years of age (due to slow metabolism, accumulation of lidocaine is possible), history of hypersensitivity to other amide local anesthetics.
Side Effects
Side Effects
From the nervous system, sensory organs and psyche: depression or excitation of the central nervous system, nervousness, euphoria, headache, dizziness, drowsiness, general weakness, neurotic reactions, confusion or loss of consciousness, depression or cessation of breathing, disorientation, convulsions (the risk of development increases against the background of hypercapnia and acidosis), tinnitus, paresthesia, diplopia, nystagmus, photophobia, tremor, trismus of facial muscles, anxiety.
From the cardiovascular system: decrease or increase in blood pressure, cardiac conduction disturbances, arrhythmia, sinus bradycardia, peripheral vasodilation, collapse, chest pain, cardiac arrest.
Allergic reactions: generalized exfoliative dermatitis, anaphylactic shock, angioedema, contact dermatitis (hyperemia at the application site, skin rash, urticaria, itching).
From the digestive system: nausea, vomiting.
Others: sensation of “hot”, “cold” or numbness of the extremities, persistent anesthesia, erectile dysfunction, malignant hyperthermia, methemoglobinemia, flashing of “flies” before the eyes and tachycardia when administered simultaneously with a vasoconstrictor.
Interaction
Interaction
Beta blockers and cimetidine increase the risk of toxic effects. Aymaline, amiodarone, verapamil and quinidine enhance the negative inotropic effect.
Inducers of microsomal liver enzymes (barbiturates, phenytoin, rifampicin) reduce the effectiveness of lidocaine.
Vasoconstrictors (epinephrine, methoxamine, phenylephrine) prolong the local anesthetic effect of lidocaine and can cause increased blood pressure and tachycardia.
Lidocaine reduces the effect of antimyasthenic drugs.
Combined use with procainamide can cause stimulation of the central nervous system and hallucinations.
Guanadrel, guanethidine, mecamylamine, trimethaphan camsylate increase the risk of a pronounced decrease in blood pressure and bradycardia. Strengthens and prolongs the effect of muscle relaxants.
The combined use of lidocaine and phenytoin should be used with caution, as it is possible to reduce the resorptive effect of lidocaine, as well as the development of an undesirable cardiodepressive effect.
Under the influence of monoamine oxidase inhibitors, the local anesthetic effect of lidocaine and a decrease in blood pressure are likely to be enhanced. Patients taking monoamine oxidase inhibitors should not be prescribed lidocaine.
With the simultaneous administration of lidocaine and polymyxin B, an increased inhibitory effect on neuromuscular transmission is possible. In this case, it is necessary to monitor the patient’s respiratory function.
When lidocaine is used in combination with hypnotics or sedatives, narcotic analgesics, hexenal or sodium thiopental, the inhibitory effect on the central nervous system and respiration may be enhanced. When lidocaine is administered intravenously to patients taking cimetidine, undesirable effects such as stunned state, drowsiness, bradycardia, paresthesia, etc. are possible. This is due to an increase in the concentration of lidocaine in the blood plasma, which is explained by the release of lidocaine from binding with blood proteins, as well as a slowdown in its inactivation in the liver. If combination therapy with these drugs is necessary, the dose of lidocaine should be reduced.
When treating the injection site with disinfectant solutions containing heavy metals, the risk of developing a local reaction in the form of pain and swelling increases.
Overdose
Overdose
Symptoms: the first signs of intoxication – dizziness, nausea, vomiting, euphoria, decreased blood pressure, asthenia; then – convulsions of facial muscles with transition to tonic-clonic convulsions of skeletal muscles, psychomotor agitation, bradycardia, asystole, collapse; when used during childbirth, the newborn may experience bradycardia, depression of the respiratory center, apnea.
Treatment is cessation of drug administration, pulmonary ventilation, oxygen inhalation. Symptomatic therapy. For convulsions, 10 mg of diazepam is administered intravenously. For bradycardia – m-cholinergic blockers (atropine), vasoconstrictors (norepinephrine, phenylephrine). Intubation, artificial ventilation, and resuscitation measures are possible. Hemodialysis is ineffective.
Storage conditions
Storage conditions
In a place protected from light at a temperature of 15 to 25 ° C. Keep out of the reach of children.
Shelf life
Shelf life
4 years. Do not use after the expiration date indicated on the package.
Manufacturer
Manufacturer
Grotex LLC, Russia
Additional information
| Shelf life | 4 years. Do not use after the expiration date stated on the package. |
|---|---|
| Conditions of storage | Store in a light-protected place at 15 to 25 °C. Keep out of reach of children. |
| Manufacturer | Grotex Ltd, Russia |
| Medication form | solution for injection |
| Brand | Grotex Ltd |
Other forms…
Related products
Buy Lidocaine, 20 mg/ml 2 ml 10 pcs with delivery to USA, UK, Europe and over 120 other countries.