No products in the cart.
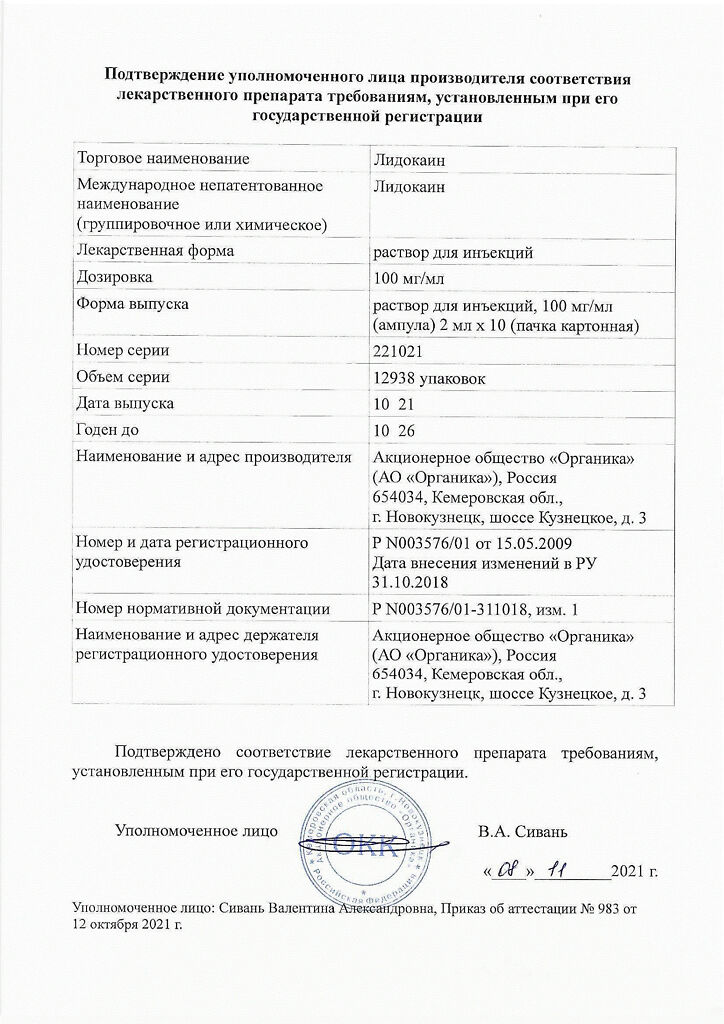
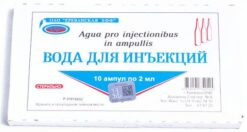
Lidocaine, 100 mg/ml 2 ml 10 pcs
€1.72 €1.56
Description It has local anesthetic effect, blocks potential-dependent sodium channels, which prevents the generation of impulses in the endings of sensitive nerves and impulse conduction along the nerve fibers. It suppresses not only pain impulses but also impulses of other modalities. Pharmacokinetics:
Anesthetic effect of lidocaine is 2-6 times stronger than procaine (effect is faster and longer – up to 75 minutes, and after adding epinephrine – more than 2 hours). When applied topically, it dilates blood vessels and has no local irritant effect on tissues.
During parenteral administration the degree of absorption depends on the site of administration and the dose. At a concentration of 20 mg/ml intravenous is not used. Time to reach maximum concentration (Tcmax) in epidural injection is less than 30 minutes.
Binding with plasma proteins is 50-80 %. It is administered quickly (half-life period of distribution phase is 6-9 minutes). Firstly the drug enters into well supplied with blood tissues (heart, lungs, brain, liver, spleen), then into fat and muscle tissues. It penetrates through the blood-brain barrier (BBB), placental barrier and is secreted with breast milk (40 % of concentration in mother’s plasma).
Metabolized in liver (90-95 %) with microsomal enzymes by dealkylation of amino group and breaking the amide bond to form active metabolites (monoethylglycystylidine and glycystylidine) with half-life (T1/2) of 2 and 10 hours, respectively. Metabolism intensity decreases and makes 50 % to 10 % of the normal value if liver function is disturbed.
It is eliminated in the bile (part of the dose is reabsorbed in the gastrointestinal tract) and the kidneys (up to 10 % unchanged). Cumulation of metabolites is possible in chronic renal failure. Urine acidification increases lidocaine excretion.
Indications
Indications
– local infiltration anesthesia;
– conduction anesthesia (including retrobulbar, parabulbar);
– spinal anesthesia;
– epidural anesthesia.
Pharmacological effect
Pharmacological effect
It has a local anesthetic effect, blocks voltage-gated sodium channels, which prevents the generation of impulses in the endings of sensory nerves and the conduction of impulses along nerve fibers. Suppresses the conduction of not only pain impulses, but also impulses of other modalities.
The anesthetic effect of lidocaine is 2-6 times stronger than procaine (it acts faster and longer – up to 75 minutes, and after adding epinephrine – more than 2 hours). When applied topically, it dilates blood vessels and does not have a local irritating effect on tissue.
Pharmacokinetics:
When administered parenterally, the extent of absorption depends on the site of administration and dose. At a concentration of 20 mg/ml it is not used intravenously. The time to reach maximum concentration (Tcmax) with epidural administration is less than 30 minutes.
Communication with plasma proteins – 50-80%. It is distributed quickly (the half-life of the distribution phase is 6-9 minutes), first the drug enters well-supplied tissues (heart, lungs, brain, liver, spleen), then into adipose and muscle tissue. Penetrates the blood-brain barrier (BBB), the placental barrier, and is secreted into breast milk (40% of the concentration in maternal plasma).
Metabolized in the liver (90-95%) with the participation of microsomal enzymes by dealkylation of the amino group and cleavage of the amide bond with the formation of active metabolites (monoethylglycinxylidine and glycinxylidine), the half-life of which (T1/2) is 2 hours and 10 hours, respectively. If liver function is impaired, the metabolic rate decreases and ranges from 50% to 10% of the normal value.
Excreted with bile (part of the dose is reabsorbed in the gastrointestinal tract) and kidneys (up to 10% unchanged). In chronic renal failure, accumulation of metabolites is possible. Acidification of urine increases the excretion of lidocaine.
Special instructions
Special instructions
The use of lidocaine, solution for injection (2%) as an antiarrhythmic agent is unacceptable.
Particular care should be taken when performing local anesthesia on organs rich in blood vessels; Intravascular injection should be avoided during administration. When injecting into vascularized tissues, an aspiration test is recommended. It is necessary to discontinue monoamine oxidase inhibitors (MAOIs) at least 10 days before planning subarachnoid anesthesia with lidocaine.
With rapid intravenous administration, a sharp decrease in blood pressure can occur and collapse may develop. In these cases, phenylephrine, ephedrine and other vasoconstrictors are used.
Impact on the ability to drive vehicles. Wed and fur.:
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Lidocaine
Composition
Composition
Active substance:
Contraindications
Contraindications
– hypersensitivity to any of the components of the drug;
– history of hypersensitivity to other amide local anesthetic drugs;
– infection of the intended injection site;
– sick sinus syndrome;
– atrioventricular block II-III degree (except for cases when an artificial pacemaker is installed);
– sinoauricular blockade;
– Wolff-Parkinson-White syndrome (WPW syndrome);
– cardiogenic shock;
– intraventricular conduction disorders;
– angle-closure glaucoma (with retrobulbar injection);
– pregnancy, breastfeeding (penetrates the placental barrier, excreted in breast milk).
It is also necessary to take into account general contraindications to this or that type of anesthesia.
With caution:
Chronic heart failure II-III functional class according to the New York Heart Association (NYHA) classification, severe liver failure, severe renal failure, hypovolemia, first degree atrioventricular block, sinus bradycardia, arterial hypotension, myasthenia gravis, a history of epileptiform seizures (including those caused by lidocaine), children under 12 years of age (due to delayed metabolism, accumulation of the drug is possible), seriously ill patients, debilitated patients, old age (over 65 years), local anesthesia of areas rich in blood vessels.
For spinal (subarachnoid) and epidural anesthesia – diseases of the central nervous system (CNS) (including infections, tumors), the presence of blood in the cerebrospinal fluid, parasthesia, psychosis, spinal deformity, peripheral neuropathy, aortic stenosis, antiplatelet therapy (including acetylsalicylic acid).
Side Effects
Side Effects
The incidence of side effects is given in accordance with the classification of the World Health Organization: very often – at least 10%; often – not less than 1% and less than 10%; not often – not less than 0.1% and less than 1%; rarely – not less than 0.01% and less than 0.1%; very rare – less than 0.01%, including isolated cases.
From the central nervous system and sensory organs: often – dizziness, headache, weakness, infrequently – motor restlessness, rarely – nystagmus, loss of consciousness, drowsiness, visual and auditory disturbances, tremor, trismus, convulsions (the risk of their development increases against the background of hypercapnia and acidosis), very rarely – paralysis of the respiratory muscles, respiratory arrest, motor and sensory block, respiratory paralysis (more often develops with subarachnoid anesthesia).
From the cardiovascular system: often – increase or decrease in blood pressure, rarely – bradycardia, arrhythmia, tachycardia – when administered with a vasoconstrictor, very rarely – peripheral vasodilation, collapse, chest pain.
From the gastrointestinal tract: often – nausea, vomiting, involuntary defecation.
From the blood: infrequently – methemoglobinemia.
Local reactions: often – with spinal anesthesia – back pain, with epidural anesthesia – accidental entry into the subarachnoid space.
Allergic reactions: often – skin rash, urticaria (on the skin and mucous membranes), skin itching, very rarely – angioedema, anaphylactic shock.
Other: infrequently – persistent anesthesia, very rarely – respiratory depression, even arrest, hypothermia.
Interaction
Interaction
Vasoconstrictors (epinephrine, methoxamine, phenylephrine) prolong the local anesthetic effect.
Cimetidine reduces the hepatic clearance of lidocaine (decreased metabolism due to inhibition of microsomal oxidation) and increases the risk of toxic effects.
Reduces the effect of antimyasthenic drugs. When treating the injection site of a local anesthetic with disinfectant solutions containing heavy metals, the risk of developing a local reaction in the form of pain and swelling increases.
When using local anesthetic drugs for spinal and epidural anesthesia with guanadrel, guanethidine, mecamylamine, trimethophan camsylate, the risk of severe hypotension and bradycardia increases.
Beta-blockers slow down the metabolism of lidocaine, increasing its toxicity (decreased hepatic blood flow). Cardiac glycosides weaken the cardiotonic effect. Strengthens and prolongs the effect of muscle relaxants. With the simultaneous administration of lidocaine and hypnotics and sedatives, their inhibitory effect on the central nervous system may be enhanced.
When used together with narcotic analgesics, an additive effect develops, which is used during epidural anesthesia, but respiratory depression increases.
Use with monoamine oxidase inhibitors (furazolidone, procarbazine, selegiline) increases the risk of low blood pressure.
Anticoagulants (including ardeparin sodium, dalteparin sodium, danaparoid sodium, enoxaparin sodium, heparin sodium, warfarin and others) increase the risk of bleeding.
Does not reduce the antimicrobial activity of sulfonamides (no formation of PABA (para-aminobenzoic acid) occurs during metabolism).
Overdose
Overdose
Symptoms: initial signs of intoxication – dizziness, nausea, vomiting, euphoria, drowsiness, headache, paresthesia, disorientation, blurred vision; then – convulsions of facial muscles with transition to tonic-clonic convulsions of skeletal muscles, psychomotor agitation, asthenia, apnea, bradycardia, decreased blood pressure, collapse, methemoglobinemia; when used during childbirth, in a newborn – bradycardia, depression of the respiratory center, apnea.
Treatment: when the first signs of intoxication appear, the administration is stopped, the patient is transferred to a horizontal position and oxygenation is carried out. For convulsions, 10 mg of diazepam is administered intravenously, for bradycardia – m-cholinergic blockers (atropine), vasoconstrictors (norepinephrine, phenylephrine). If necessary, intubation, artificial ventilation, and resuscitation measures are indicated. Dialysis is ineffective.
Storage conditions
Storage conditions
In a place protected from light, at a temperature not exceeding 25°C. Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after the expiration date stated on the package.
Manufacturer
Manufacturer
Organika, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date shown on the package. |
|---|---|
| Conditions of storage | Store in a dark place at a temperature not exceeding 25°C. Keep out of reach of children. |
| Manufacturer | Organika, Russia |
| Medication form | solution for injection |
| Brand | Organika |
Other forms…
Related products
Buy Lidocaine, 100 mg/ml 2 ml 10 pcs with delivery to USA, UK, Europe and over 120 other countries.