No products in the cart.
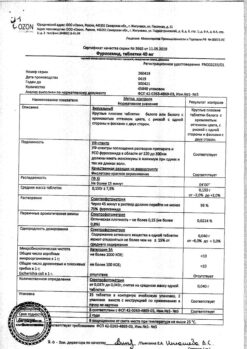
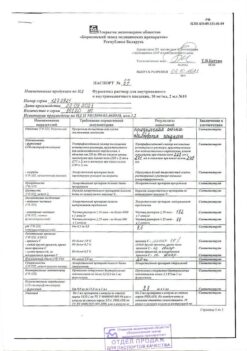
Furosemide, tablets 40 mg 56 pcs
€3.68 €2.32
Description
Pharmacotherapeutic group: Diuretic.
ATC code: C03CA01
Pharmacological properties
Pharmacodynamics
Furosemide is a fast-acting diuretic that is a sulfonamide derivative. Furosemide blocks the transport system of sodium, potassium, chlorine ions in the thick segment of ascending knee of Genle loop, due to which its diuretic action depends on entering the drug into renal tubules lumen (due to mechanism of anion transport). Diuretic effect of Furosemide is associated with inhibition of sodium chloride reabsorption in this part of the Genle loop. Secondary effects to the increase in sodium excretion are: increase in the amount of excreted urine (due to osmotically bound water) and increased potassium secretion in the distal part of the renal tubule. At the same time the excretion of calcium and magnesium ions increases.
If tubular secretion is decreased or if furosemide binds to albumin in the tubular lumen (e.g., in nephrotic syndrome), the effect of furosemide is reduced.
Furosemide does not decrease diuretic activity when administered as a course because furosemide interrupts the tubule-glomerular feedback in Macula densa (a tubular structure closely associated with the juxtaglomerular complex). Furosemide causes dose-dependent stimulation of the renin-angiotensin-aldosterone system.
In heart failure, furosemide rapidly reduces preload (through vein dilation), reduces pulmonary artery pressure and left ventricular filling pressure. This rapidly developing effect appears to be mediated through the effects of prostaglandins, and therefore a condition for its development is the absence of disturbances in prostaglandin synthesis, in addition to which sufficient preservation of renal function is also required to realize this effect.
Furosemide has hypotensive effect due to increase in sodium excretion, decrease in circulating blood volume and decrease in vascular smooth muscle response to vasoconstrictor stimuli (due to the natriuretic effect furosemide reduces vascular response to catecholamines which concentration is increased in patients with arterial hypertension).
After oral administration of 40 mg of Furosemide, the diuretic effect develops within 60 minutes and lasts about 3-6 hours. When increasing the dosage of Furosemide from 10 to 100 mg, a dose-dependent increase in diuresis and natriuresis is observed.
Pharmacokinetics
Intake
Furosemide is rapidly absorbed in the gastrointestinal tract. The time to reach maximum blood concentration (Tmax) is 1 to 1.5 hours. Bioavailability of furosemide in healthy volunteers is approximately 50-70%. In patients, the bioavailability of furosemide may decrease up to 30%, as it may be affected by various factors, including the underlying disease.
Distribution
The volume of distribution of furosemide is 0.1-0.2 L/kg body weight. Furosemide binds to plasma proteins (more than 98%), mainly to albumin.
Metabolism/Exhaustion
Furosemide is excreted predominantly unchanged and mainly by secretion in the proximal tubules. Glucuronized metabolites of furosemide account for 10-20% of the drug excreted by the kidneys. The remaining dose is excreted through the intestine, apparently by biliary secretion. Final elimination half-life of furosemide is approximately 1-1.5 hours. Furosemide penetrates the placental barrier and is excreted in the mother’s milk. Its concentrations in the fetus and the newborn are the same as in the mother.
Peculiarities of pharmacokinetics in selected groups of patients
In renal failure elimination of furosemide is delayed and the elimination half-life is prolonged; in severe renal insufficiency, the final elimination half-life may be prolonged up to 24 hours.
In nephrotic syndrome, decreased plasma protein concentrations lead to increased concentrations of unbound furosemide (its free fraction), thereby increasing the risk of ototoxic effects. On the other hand, the diuretic effect of furosemide in these patients may be reduced due to the binding of furosemide to albumin in the tubules and decreased tubular secretion of furosemide.
In hemodialysis and peritoneal dialysis, and continuous ambulatory peritoneal dialysis, furosemide is marginally excreted.
In hepatic insufficiency, the half-life of furosemide is increased by 30-90%, mainly due to increased volume of distribution. Pharmacokinetic parameters in this category of patients may vary significantly.
In heart failure, severe arterial hypertension and in elderly patients excretion of furosemide is delayed due to decreased renal function.
Indications
Indications
Edema syndrome in chronic heart failure;
edema syndrome in chronic renal failure;
acute renal failure, including that during pregnancy and burns (to maintain fluid excretion);
edema syndrome in nephrotic syndrome (in nephrotic syndrome, treatment of the underlying disease is in the foreground);
edema syndrome in liver diseases (if necessary in addition to treatment with aldosterone antagonists);
arterial hypertension.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: diuretic.
ATX code: C03CA01
Pharmacological properties
Pharmacodynamics
Furosemide is a fast-acting diuretic that is a sulfonamide derivative. Furosemide blocks the transport system of sodium, potassium, and chlorine ions in the thick segment of the ascending limb of the loop of Henle, and therefore its diuretic effect depends on the drug entering the lumen of the renal tubules (due to the anion transport mechanism). The diuretic effect of the drug Furosemide is associated with inhibition of sodium chloride reabsorption in this section of the loop of Henle. Secondary effects to the increase in sodium excretion are: an increase in the amount of urine excreted (due to osmotically bound water) and an increase in the secretion of potassium in the distal part of the renal tubule. At the same time, the excretion of calcium and magnesium ions increases.
When tubular secretion decreases or when furosemide binds to albumin located in the tubular lumen (for example, in nephrotic syndrome), the effect of furosemide is reduced.
With a course of furosemide, its diuretic activity does not decrease, since furosemide interrupts the tubular-glomerular feedback in the Macula densa (a tubular structure closely associated with the juxtaglomerular complex). Furosemide causes dose-dependent stimulation of the renin-angiotensin-aldosterone system.
In heart failure, furosemide quickly reduces preload (due to venous dilatation), reduces pulmonary artery pressure and left ventricular filling pressure. This rapidly developing effect appears to be mediated through the effects of prostaglandins, and therefore the condition for its development is the absence of disturbances in the synthesis of prostaglandins, in addition to which the realization of this effect also requires sufficient preservation of renal function.
Furosemide has a hypotensive effect, which is caused by an increase in sodium excretion, a decrease in circulating blood volume and a decrease in the response of vascular smooth muscle to vasoconstrictor stimuli (due to the natriuretic effect, furosemide reduces the vascular response to catecholamines, the concentration of which is increased in patients with arterial hypertension).
After oral administration of 40 mg of Furosemide, the diuretic effect develops within 60 minutes and lasts about 3-6 hours. When the dosage of Furosemide is increased from 10 to 100 mg, a dose-dependent increase in diuresis and natriuresis is observed.
Pharmacokinetics
Suction
Furosemide is rapidly absorbed from the gastrointestinal tract. The time to reach maximum concentration in the blood (Tmax) ranges from 1 to 1.5 hours. The bioavailability of furosemide in healthy volunteers is approximately 50-70%. In patients, the bioavailability of furosemide may be reduced by up to 30%, as it may be influenced by various factors, including the underlying disease.
Distribution
The volume of distribution of furosemide is 0.1-0.2 l/kg body weight. Furosemide binds to blood plasma proteins (more than 98%), mainly to albumin.
Metabolism/Excretion
Furosemide is excreted predominantly unchanged and mainly by secretion in the proximal tubules. Glucuronidated metabolites of furosemide account for 10-20% of the drug excreted by the kidneys. The remaining dose is excreted through the intestines, apparently by biliary secretion. The terminal half-life of furosemide is approximately 1-1.5 hours. Furosemide penetrates the placental barrier and is excreted into breast milk. Its concentrations in the fetus and newborn are the same as in the mother.
Features of pharmacokinetics in certain groups of patients
In renal failure, the elimination of furosemide slows down and the half-life increases; with severe renal failure, the terminal half-life may increase to 24 hours.
In nephrotic syndrome, a decrease in plasma protein concentrations leads to an increase in the concentration of unbound furosemide (its free fraction), and therefore the risk of developing ototoxicity increases. On the other hand, the diuretic effect of furosemide in these patients may be reduced due to the binding of furosemide to tubular albumin and decreased tubular secretion of furosemide.
During hemodialysis and peritoneal dialysis, and continuous outpatient peritoneal dialysis, furosemide is excreted insignificantly.
In liver failure, the half-life of furosemide is increased by 30-90%, mainly due to an increase in the volume of distribution. Pharmacokinetic parameters in this category of patients can vary significantly.
In heart failure, severe arterial hypertension and in elderly patients, the excretion of furosemide slows down due to decreased renal function.
Special instructions
Special instructions
Symptomatic hypotension, leading to dizziness, fainting or loss of consciousness, may occur in patients receiving furosemide, especially: elderly patients; in patients taking other drugs that can lead to arterial hypotension; as well as in patients with other diseases that carry a risk of developing arterial hypotension. These patients should be treated with caution and/or may require a dose reduction of furosemide.
Before starting treatment with Furosemide, the presence of pronounced disturbances in the outflow of urine, including unilateral ones, should be excluded. Patients with partial obstruction of urinary outflow require careful monitoring, especially at the beginning of treatment with Furosemide.
During treatment with Furosemide, regular monitoring of sodium, potassium and creatinine concentrations in the blood serum is required; Particularly careful monitoring should be carried out in patients at high risk of developing fluid and electrolyte imbalance in cases of additional fluid and electrolyte losses (for example, due to vomiting, diarrhea or intense sweating).
Before and during treatment with Furosemide, it is necessary to monitor and, if occurring, correct hypovolemia or dehydration, as well as clinically significant disturbances in water-electrolyte balance and/or acid-base status, which may require short-term cessation of treatment with Furosemide.
When treating with Furosemide, it is always advisable to eat foods rich in potassium (lean meat, potatoes, bananas, tomatoes, cauliflower, spinach, dried fruits, etc.). In some cases, taking potassium supplements or taking potassium-sparing drugs may be indicated.
In patients with hypoproteinemia, such as that associated with nephrotic syndrome, the effectiveness of furosemide may be reduced and its ototoxicity may be increased. Careful dose increases are required.
There was a higher incidence of death in elderly patients with dementia receiving concomitant treatment with risperidone and furosemide compared with patients receiving either furosemide alone or risperidone alone. The pharmacophysiological mechanism of this effect has not been established. Concomitant use of risperidone with other diuretics (mainly low-dose thiazide diuretics) was not associated with an increase in mortality in elderly patients with dementia. In elderly patients with dementia, furosemide and risperidone should be used concomitantly with caution, carefully weighing the balance of benefit and risk. Because dehydration is a common risk factor for increased mortality, dehydration of the patient should be avoided when deciding to use this combination in elderly patients with dementia.
There is a possibility of worsening the course or exacerbation of systemic lupus erythematosus.
The selection of a dosage regimen for patients with ascites against the background of liver cirrhosis should be carried out in a hospital (imbalances in water and electrolyte balance can lead to the development of hepatic coma).
Impact on the ability to drive vehicles and machinery
Some side effects (for example, a significant decrease in blood pressure) may impair the ability to concentrate and reduce psychomotor reactions, which can be dangerous when driving or engaging in other potentially hazardous activities. This especially applies to the period of starting treatment or increasing the dose of the drug, as well as to cases of simultaneous use of antihypertensive drugs or alcohol. In such cases, it is not recommended to drive vehicles or engage in potentially hazardous activities.
Active ingredient
Active ingredient
Furosemide
Composition
Composition
Active ingredient: Furosemide 40.00 mg
Excipients:
potato starch 56.88 mg
lactose monohydrate 53.00 mg
pregelatinized corn starch 7.00 mg
talc 2.40 mg
colloidal silicon dioxide (Aerosil) 0.40 mg
magnesium stearate 0.32 mg
Pregnancy
Pregnancy
Pregnancy
Furosemide crosses the placental barrier, so the drug should not be prescribed during pregnancy. Taking furosemide is possible only if the expected benefit to the mother outweighs the potential risk to the fetus; in such cases, careful monitoring of the fetus’s condition is necessary.
Breastfeeding period
During lactation, taking the drug is contraindicated, since furosemide can be excreted in breast milk and suppress lactation. Women taking furosemide should stop breastfeeding.
Contraindications
Contraindications
Hypersensitivity to the active substance or to any of the excipients of the drug;
in patients with an allergy to sulfonamides (sulfonamide antimicrobial agents or sulfonylurea derivatives), since it is possible to develop a “cross” allergy to furosemide;
renal failure with anuria (in the absence of response to furosemide);
hepatic coma and precoma associated with hepatic encephalopathy;
severe hypokalemia (see section “Side effects”);
severe hyponatremia;
hypovolemia (with or without a decrease in blood pressure) or dehydration;
severe disturbances in the outflow of urine of any etiology, including unilateral damage to the urinary tract;
intoxication with cardiac glycosides;
acute glomerulonephritis;
decompensated aortic and mitral stenosis, hypertrophic obstructive cardio-
myopathy;
increased central venous pressure (over 10 mm Hg);
rare hereditary galactose intolerance, lactase deficiency, glucose-galactose malabsorption syndrome;
children under 3 years of age (solid dosage form);
pregnancy (see section “Use during pregnancy and breastfeeding”);
period of breastfeeding (see section “Use during pregnancy and breastfeeding”).
With caution
With arterial hypotension;
in conditions where an excessive decrease in blood pressure is especially dangerous (severe stenosis of the coronary and/or cerebral arteries);
in case of acute myocardial infarction (increased risk of developing cardiogenic shock);
with latent or manifest diabetes mellitus;
for gout;
with hepatorenal syndrome (functional renal failure associated with liver disease);
with hypoproteinemia (for example, nephrotic syndrome, when the diuretic effect may decrease and the risk of developing the ototoxic effect of furosemide may increase); Dosage selection in such patients should be carried out with extreme caution;
with partial obstruction of the urinary tract (prostatic hyperplasia, narrowing of the urethra);
with an increased risk of developing disorders of the water-electrolyte balance and acid-base state or in case of significant fluid losses (vomiting, diarrhea, profuse sweating – monitoring of the water-electrolyte balance and acid-base state is required and, if necessary, correction of their disorders before starting the use of furosemide);
with pancreatitis;
with a history of ventricular arrhythmias;
with systemic lupus erythematosus;
with simultaneous use of risperidone in elderly patients with dementia (risk of increased mortality).
Side Effects
Side Effects
Below are the adverse reactions (ARs) that were identified during clinical studies, as well as during the use of furosemide in clinical practice.
To assess the frequency of ADR, the following criteria were used: “very often” (≥ 1/10); “often” (≥ 1/100, < 1/10); “uncommon” (≥ 1/1000, < 1/100); “rare” (≥ 1/10000, < 1/1000); “very rare” (< 1/10000). AEs are grouped in accordance with the system-organ classes of the medical dictionary for regulatory activities MedDRA; within each class, AEs are listed in descending order of frequency of occurrence; within each group, allocated by frequency of occurrence, AEs are distributed in decreasing order of their importance.
Blood and lymphatic system disorders
Often:
hemoconcentration.
Uncommon:
thrombocytopenia.
Rarely:
leukopenia, eosinophilia.
Very rarely:
agranulocytosis, aplastic anemia or hemolytic anemia.
Immune system disorders
Rarely:
severe anaphylactic or anaphylactoid reactions up to the development of anaphylactic shock.
Frequency unknown:
worsening of the course or exacerbation of systemic lupus erythematosus.
Metabolic and nutritional disorders
Very often:
disturbances of water and electrolyte balance, including disturbances of water and electrolyte balance that occur with clinical symptoms. Symptoms indicating the development of water and electrolyte imbalances may include headache, convulsions, tetany, muscle weakness, heart rhythm disturbances and dyspeptic disorders. Such disorders can develop either gradually (over a long time) or quickly (over a very short time, for example, in the case of high doses of Furosemide in patients with normal renal function). Factors contributing to the development of water-electrolyte imbalances are underlying diseases (for example, cirrhosis of the liver or heart failure), concomitant therapy with drugs that change the water-electrolyte balance, poor nutrition and drinking regimen, vomiting, diarrhea, profuse sweating;
dehydration and hypovolemia (decrease in circulating blood volume), especially in elderly patients, which can lead to hemoconcentration with an increased risk of thrombosis (see below);
increased concentration of creatinine in the blood;
increased concentration of triglycerides in the blood serum.
Often:
hyponatremia, hypochloremia, hypokalemia, increased concentration of cholesterol in the blood;
an increase in the concentration of uric acid in the blood and attacks of gout.
Uncommon:
decreased glucose tolerance. Latent diabetes mellitus can become manifest (see section “Special instructions”).
Frequency unknown:
hypocalcemia, hypomagnesemia, increased urea concentration in the blood, metabolic alkalosis, pseudo-Bartter syndrome with improper and/or long-term use of furosemide.
Nervous system disorders
Often:
hepatic encephalopathy in patients with hepatocellular insufficiency (see section “Contraindications”).
Rarely:
paresthesia.
Frequency unknown:
dizziness, syncope (fainting) or loss of consciousness, headache.
Disorders of the hearing organ and labyrinth
Uncommon:
hearing impairment, usually transient, especially in patients with renal failure,
hypoproteinemia (for example, in nephrotic syndrome) and/or rapid intravenous administration of furosemide. Cases of deafness, sometimes irreversible, have been reported after oral or intravenous administration of furosemide.
Rarely:
tinnitus.
Vascular disorders
Very often (for intravenous infusion):
decreased blood pressure, including orthostatic hypotension (this adverse reaction mainly relates to parenteral use of furosemide).
Rarely:
vasculitis
Frequency unknown:
thrombosis.
Gastrointestinal disorders
Uncommon:
nausea.
Rarely:
vomiting, diarrhea.
Very rarely:
acute pancreatitis.
Disorders of the liver and biliary tract
Very rarely:
cholestasis, increased activity of “liver” transaminases.
Skin and subcutaneous tissue disorders
Uncommon:
skin itching, urticaria, rash, bullous dermatitis, erythema multiforme, pemphigoid, exfoliative dermatitis, purpura, photosensitivity reactions.
Frequency unknown:
Stevens-Johnson syndrome, toxic epidermal necrolysis, acute generalized exanthematous pustulosis, DRESS syndrome: drug rash with eosinophilia and systemic symptoms.
Muscle, skeletal and connective tissue disorders
Frequency unknown:
Cases of rhabdomyolysis have been reported, often associated with severe hypokalemia (see section “Contraindications”).
Renal and urinary tract disorders
Often:
increase in urine volume.
Rarely:
tubulointerstitial nephritis.
Frequency unknown:
increased sodium and chloride levels in the urine;
urinary retention (in patients with partial obstruction of the urinary tract, see section “Special instructions”);
nephrocalcinosis/nephrolithiasis in premature infants (see section “Special instructions”). This HP applies only to the injection dosage form of Furosemide, since children under 3 years of age are contraindicated in taking Furosemide tablets;
renal failure (see section “Interaction with other drugs”).
Congenital, familial and genetic disorders
Frequency unknown:
increased risk of patent ductus arteriosus when furosemide is administered to premature infants during the first weeks of life (applies to parenteral dosage form only).
General disorders and reactions at the injection site
Rarely:
fever.
Since some adverse events (such as changes in the blood picture, severe anaphylactic or anaphylactoid reactions, severe allergic skin reactions) under certain conditions can threaten the lives of patients, if any adverse events occur, they should be reported to the doctor immediately.
Interaction
Interaction
Combinations not recommended
Chloral hydrate – intravenous infusion of furosemide within a 24-hour period after administration of chloral hydrate may lead to flushing of the skin, profuse sweating, restlessness, nausea, increased blood pressure and tachycardia. Therefore, the use of furosemide in combination with chloral hydrate is not recommended.
Aminoglycosides – slowing down the excretion of aminoglycosides by the kidneys when used simultaneously with furosemide and increasing the risk of developing ototoxic and nephrotoxic effects of aminoglycosides. For this reason, the use of this combination of drugs should be avoided, except in cases where it is necessary for health reasons, in which case an adjustment (reduction) of maintenance doses of aminoglycosides is required.
Combinations to use with caution
Ototoxic drugs – furosemide potentiates their ototoxicity. Such drugs can be used simultaneously with Furosemide only for strict medical indications, since combined use can lead to irreversible damage to the hearing organ.
Cisplatin – when used simultaneously with furosemide, there is a risk of ototoxicity. In addition, the nephrotoxic effect of cisplatin may be enhanced when furosemide is used for forced diuresis during treatment with cisplatin, unless furosemide is used in a low dose (for example, 40 mg in patients with normal renal function) and without combination with appropriate hydration of the patient.
Sucralfate – decreases the absorption of furosemide when taken orally and weakens its effect (furosemide and sucralfate when taken orally should be taken at least two hours apart).
Lithium salts – under the influence of furosemide, the excretion of lithium is reduced, due to which the content of lithium in the blood serum increases, which increases the risk of its toxic effects, including cardiotoxic and neurotoxic effects. Therefore, when using this combination, monitoring of serum lithium levels is required.
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor antagonists – use of ACE inhibitors or angiotensin II receptor antagonists in patients
previously treated with furosemide, can lead to an excessive decrease in blood pressure with deterioration of renal function, and in some cases – to the development of acute renal failure, therefore, 3 days before starting treatment or increasing the dose of ACE inhibitors or angiotensin II receptor antagonists, it is recommended to discontinue furosemide or reduce its dose.
Risperidone – Caution should be exercised, carefully weighing the balance of risk and benefit, before deciding to use a combination of risperidone with furosemide or other strong diuretics, as an increase in mortality has been observed in elderly patients with dementia receiving concomitant treatment with risperidone and furosemide.
Levothyroxine-furosemide in high doses can inhibit the binding of thyroid hormones to carrier proteins and thus lead initially to a transient increase in the concentrations of free thyroid hormones, and then, overall, to a decrease in the total concentration of thyroid hormones. When using this combination, thyroid hormone concentrations should be monitored.
Interactions to Consider
Nonsteroidal anti-inflammatory drugs (NSAIDs) – NSAIDs, including acetylsalicylic acid, may reduce the diuretic effect of furosemide.
In patients with hypovolemia and dehydration (including while taking Furosemide), NSAIDs can cause the development of acute renal failure. Furosemide may increase the toxicity of salicylates.
Phenytoin – decreases the diuretic effect of furosemide.
Glucocorticosteroids, carbenoxolone, licorice preparations in large quantities and prolonged use of laxatives when combined with furosemide increase the risk of developing hypokalemia.
Cardiac glycosides, drugs that cause prolongation of the QT interval – if water and electrolyte imbalances (hypokalemia or hypomagnesemia) develop during the use of furosemide, the toxic effect of cardiac glycosides and drugs that cause prolongation of the QT interval increases (the risk of developing cardiac arrhythmias increases).
Antihypertensives, diuretics or other drugs that can lower blood pressure – when combined with furosemide, a more pronounced decrease in blood pressure is possible.
Probenecid, methotrexate or other drugs that, like furosemide, are excreted in the renal tubules, may reduce the effects of furosemide (same route of renal excretion); on the other hand, furosemide may lead to decreased renal excretion of these drugs. All this increases the risk of developing adverse reactions of both furosemide and the above-mentioned medications taken simultaneously with it.
Hypoglycemic agents (both for oral administration and insulin preparations), pressor amines (epinephrine, norepinephrine) – weakening of effects when combined with furosemide.
Theophylline, diazoxide, curare-like muscle relaxants – enhanced effects when combined with furosemide.
Medicines with nephrotoxic effects – when combined with furosemide, the risk of developing their nephrotoxic effect increases.
High doses of some cephalosporins (excreted primarily by the kidneys) – in combination with furosemide, the risk of nephrotoxicity from cephalosporins increases.
Cyclosporine A – when combined with furosemide, the risk of developing gouty arthritis increases due to hyperuricemia caused by furosemide and impaired renal urate excretion under the influence of cyclosporine.
Radiocontrast agents – Patients at high risk of developing nephropathy due to radiocontrast administration who were treated with furosemide had a higher incidence of renal dysfunction after administration of radiocontrast agents, compared with patients at high risk of developing nephropathy due to administration of radiocontrast agents who received only intravenous fluids (hydration) before administration of radiocontrast agents.
Overdose
Overdose
If you suspect an overdose, you should definitely consult a doctor, since in the event of an overdose, certain therapeutic measures may be required.
Symptoms: the clinical picture of acute or chronic drug overdose depends mainly on the degree and consequences of loss of fluid and electrolytes. Overdose may be manifested by hypovolemia, dehydration, hemoconcentration, cardiac rhythm and conduction disturbances (including atrioventricular block and ventricular fibrillation). Symptoms of these disorders are a pronounced decrease in blood pressure, progressing to the development of shock, acute renal failure, thrombosis, delirium, flaccid paralysis, apathy and confusion.
Treatment: There is no specific antidote. If a little time has passed after oral administration, then to reduce the absorption of furosemide from the gastrointestinal tract, you should try to induce vomiting or perform gastric lavage, and then take activated charcoal orally.
Treatment is aimed at correcting clinically significant disturbances in water-electrolyte balance and acid-base status under the control of the content of electrolytes in the blood serum, indicators of acid-base status, hematocrit, as well as at preventing or treating possible serious complications that develop against the background of these disorders.
Storage conditions
Storage conditions
In a place protected from light at a temperature not exceeding 25 ºС.
Keep out of the reach of children.
Shelf life
Shelf life
4 years.
Do not use after expiration date.
Manufacturer
Manufacturer
Update of PFC JSC, Russia
Additional information
| Shelf life | 4 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In the dark place at a temperature not exceeding 25 ºC. Keep out of reach of children. |
| Manufacturer | Update PFC AO, Russia |
| Medication form | pills |
| Brand | Update PFC AO |
Other forms…
Related products
Buy Furosemide, tablets 40 mg 56 pcs with delivery to USA, UK, Europe and over 120 other countries.