No products in the cart.
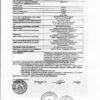
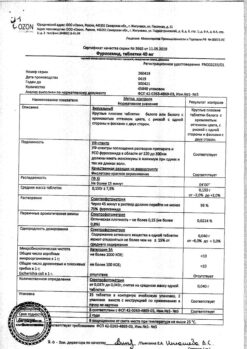
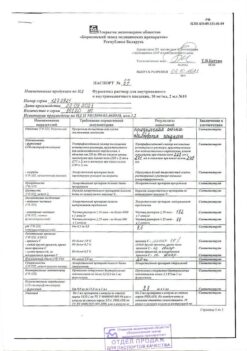
Furosemide, 10 mg/ml 2 ml 10 pcs
€1.64 €1.49
Description
“Loop” diuretic. Disrupts reabsorption of sodium, chlorine ions in the thick segment of the ascending part of the loop of Genle. Due to the increased excretion of sodium ions, there is a secondary (mediated by osmotically bound water) enhanced excretion of water and increased secretion of potassium ions in the distal part of the renal tubule. At the same time, the excretion of calcium and magnesium ions increases.
It has secondary effects due to release of intrarenal mediators and redistribution of intrarenal blood flow. There is no attenuation of the effect during the course of treatment.
In case of heart failure, it quickly leads to reduction of the preload on the heart by expanding the large veins. It has a hypotensive effect due to increased excretion of sodium chloride and due to decreased reaction of vascular smooth muscle to vasoconstrictor effects and due to reduction of the blood circulation volume. The action of furosemide after intravenous injection occurs after 5-10 min, after oral administration – after 30-60 min, maximum action – after 1-2 hours, the duration of effect – 2-3 hours (with reduced renal function – up to 8 hours). During the period of action, excretion of sodium ions increases significantly, but after its cessation the excretion rate decreases below the initial level (the syndrome of “ricochet” or “withdrawal”). The phenomenon is due to a sharp activation of renin-angiotensin and other antinatriuretic neurohumoral regulatory links in response to massive diuresis; it stimulates the arginine-vasopressive and sympathetic systems. Reduces the level of atrial natriuretic factor in plasma, causes vasoconstriction.
Owing to the “ricochet” phenomenon, once daily administration may have no significant effect on the daily excretion of sodium ions and BP. When administered intravenously, it causes dilatation of peripheral veins, reduces preload, decreases left ventricular filling pressure and pulmonary artery pressure as well as systemic BP.
The diuretic effect develops 3-4 min after IV administration and lasts 1-2 h; after oral administration, it takes 20-30 min and lasts up to 4 h.
Pharmacokinetics
After oral administration absorption is 60-70%. In severe kidney disease or chronic heart failure the degree of absorption decreases.
The Vd is 0.1 l/kg. Binding with plasma proteins (mainly with albumin) is 95-99%. Metabolized in liver. Excreted by kidneys – 88%, with bile – 12%. T1/2 in patients with normal renal and hepatic function is 0.5-1.5 hours. In anuria T1/2 may be increased up to 1.5-2.5 hours, in concomitant renal and hepatic failure – up to 11-20 hours.
Indications
Indications
Edema syndrome of various origins, incl. for chronic heart failure stage II-III, liver cirrhosis (portal hypertension syndrome), nephrotic syndrome. Pulmonary edema, cardiac asthma, cerebral edema, eclampsia, forced diuresis, severe arterial hypertension, some forms of hypertensive crisis, hypercalcemia.
Pharmacological effect
Pharmacological effect
“Loop” diuretic. It disrupts the reabsorption of sodium and chlorine ions in the thick segment of the ascending loop of Henle. Due to an increase in the release of sodium ions, a secondary (mediated by osmotically bound water) increased excretion of water and an increase in the secretion of potassium ions occurs in the distal part of the renal tubule. At the same time, the excretion of calcium and magnesium ions increases.
It has secondary effects due to the release of intrarenal mediators and redistribution of intrarenal blood flow. During the course of treatment, the effect does not weaken.
In heart failure, it quickly leads to a decrease in preload on the heart by dilating large veins. It has a hypotensive effect due to an increase in the excretion of sodium chloride and a decrease in the response of vascular smooth muscles to vasoconstrictor effects and as a result of a decrease in blood volume. The effect of furosemide after intravenous administration occurs within 5-10 minutes; after oral administration – after 30-60 minutes, maximum effect – after 1-2 hours, duration of effect – 2-3 hours (with reduced kidney function – up to 8 hours). During the period of action, the excretion of sodium ions increases significantly, but after its cessation, the rate of excretion decreases below the initial level (rebound or withdrawal syndrome). The phenomenon is caused by a sharp activation of renin-angiotensin and other antinatriuretic neurohumoral regulation units in response to massive diuresis; stimulates the arginine-vasopressive and sympathetic systems. Reduces the level of atrial natriuretic factor in plasma, causing vasoconstriction.
Due to the “ricochet” phenomenon, when taken once a day, it may not have a significant effect on the daily excretion of sodium ions and blood pressure. When administered intravenously, it causes dilatation of peripheral veins, reduces preload, reduces left ventricular filling pressure and pulmonary artery pressure, as well as systemic blood pressure.
The diuretic effect develops 3-4 minutes after IV administration and lasts 1-2 hours; after oral administration – after 20-30 minutes, lasts up to 4 hours.
Pharmacokinetics
After oral administration, absorption is 60-70%. In severe kidney disease or chronic heart failure, the degree of absorption decreases.
Vd is 0.1 l/kg. Binding to plasma proteins (mainly albumin) is 95-99%. Metabolized in the liver. Excreted by the kidneys – 88%, with bile – 12%. T1/2 in patients with normal renal and liver function is 0.5-1.5 hours. With anuria, T1/2 can increase to 1.5-2.5 hours, with combined renal and liver failure – up to 11-20 hours.
Special instructions
Special instructions
Use with caution in prostatic hyperplasia, SLE, hypoproteinemia (risk of developing ototoxicity), diabetes mellitus (decreased glucose tolerance), with stenotic atherosclerosis of the cerebral arteries, against the background of long-term therapy with cardiac glycosides, in elderly patients with severe atherosclerosis, pregnancy (especially the first half), lactation period.
Before starting treatment, electrolyte disturbances should be compensated. During treatment with furosemide, it is necessary to monitor blood pressure, levels of electrolytes and glucose in the blood serum, liver and kidney function.
To prevent hypokalemia, it is advisable to combine furosemide with potassium-sparing diuretics. With the simultaneous use of furosemide and hypoglycemic drugs, dose adjustment of the latter may be required.
It is not recommended to mix furosemide solution in the same syringe with any other drugs.
Impact on the ability to drive vehicles and operate machinery
When using furosemide, the possibility of a decrease in the ability to concentrate cannot be ruled out, which is important for people driving vehicles and working with machinery.
Active ingredient
Active ingredient
Furosemide
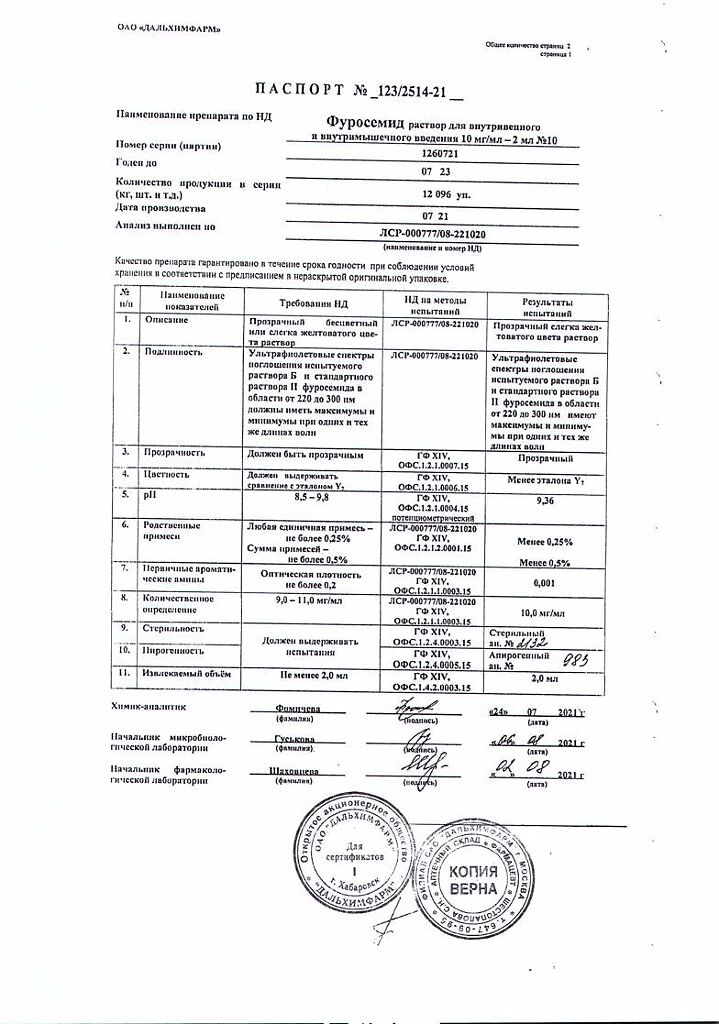
Composition
Composition
Solution for injection 1%
1 ml 1 amp.
furosemide 10 mg 20 mg
Contraindications
Contraindications
Acute glomerulonephritis, urethral stenosis, stone obstruction of the urinary tract, acute renal failure with anuria, hypokalemia, alkalosis, precomatous states, severe liver failure, hepatic coma and precoma, diabetic coma, precomatous states, hyperglycemic coma, hyperuricemia, gout, decompensated mitral or aortic stenosis, hypertrophic obstructive cardiomyopathy, increased central venous pressure (more than 10 mm Hg), arterial hypotension, acute myocardial infarction, pancreatitis, impaired water and electrolyte metabolism (hypovolemia, hyponatremia, hypokalemia, hypochloremia, hypocalcemia, hypomagnesemia), digitalis intoxication, increased sensitivity to furosemide.
Side Effects
Side Effects
From the cardiovascular system: decreased blood pressure, orthostatic hypotension, collapse, tachycardia, arrhythmias, decreased blood volume.
From the central nervous system and peripheral nervous system: dizziness, headache, myasthenia gravis, calf muscle cramps (tetany), paresthesia, apathy, adynamia, weakness, lethargy, drowsiness, confusion.
From the senses: visual and hearing impairment.
From the digestive system: loss of appetite, dry mouth, thirst, nausea, vomiting, constipation or diarrhea, cholestatic jaundice, pancreatitis (exacerbation).
From the genitourinary system: oliguria, acute urinary retention (in patients with prostatic hypertrophy), interstitial nephritis, hematuria, decreased potency.
From the hematopoietic system: leukopenia, thrombocytopenia, agranulocytosis, aplastic anemia.
From the side of water and electrolyte metabolism: hypovolemia, dehydration (risk of thrombosis and thromboembolism), hypokalemia, hyponatremia, hypochloremia, hypocalcemia, hypomagnesemia, metabolic alkalosis.
Metabolic: hypovolemia, hypokalemia, hyponatremia, hypochloremia, hypokalemic metabolic alkalosis (as a consequence of these disorders – arterial hypotension, dizziness, dry mouth, thirst, arrhythmia, muscle weakness, cramps), hyperuricemia (with possible exacerbation of gout), hyperglycemia.
Allergic reactions: purpura, urticaria, exfoliative dermatitis, exudative erythema multiforme, vasculitis, necrotizing angiitis, itching, chills, fever, photosensitivity, anaphylactic shock.
Other: with intravenous administration (additionally) – thrombophlebitis, kidney calcification in premature infants.
Interaction
Interaction
When used simultaneously with aminoglycoside antibiotics (including gentamicin, tobramycin), nephro- and ototoxic effects may be enhanced.
Furosemide reduces the clearance of gentamicin and increases plasma concentrations of gentamicin and tobramycin.
When used simultaneously with cephalosporin antibiotics, which can cause renal dysfunction, there is a risk of increased nephrotoxicity.
When used simultaneously with beta-agonists (including fenoterol, terbutaline, salbutamol) and corticosteroids, hypokalemia may increase.
When used simultaneously with hypoglycemic agents and insulin, the effectiveness of hypoglycemic agents and insulin may decrease, because furosemide has the ability to increase plasma glucose levels.
When used simultaneously with ACE inhibitors, the antihypertensive effect is enhanced. Severe arterial hypotension is possible, especially after taking the first dose of furosemide, apparently due to hypovolemia, which leads to a transient increase in the hypotensive effect of ACE inhibitors. The risk of renal dysfunction increases and the development of hypokalemia cannot be excluded.
When used simultaneously with furosemide, the effects of non-depolarizing muscle relaxants are enhanced.
When used simultaneously with indomethacin and other NSAIDs, the diuretic effect may be reduced, apparently due to inhibition of prostaglandin synthesis in the kidneys and sodium retention in the body under the influence of indomethacin, which is a nonspecific COX inhibitor; decrease in antihypertensive effect.
It is believed that furosemide interacts with other NSAIDs in a similar way.
When used simultaneously with NSAIDs, which are selective COX-2 inhibitors, this interaction is much less pronounced or practically absent.
When used simultaneously with astemizole, the risk of arrhythmia increases.
When used simultaneously with vancomycin, oto- and nephrotoxicity may increase.
When used simultaneously with digoxin and digitoxin, an increase in the toxicity of cardiac glycosides is possible, associated with the risk of developing hypokalemia while taking furosemide.
There are reports of the development of hyponatremia when used simultaneously with carbamazepine.
When used simultaneously with cholestyramine and colestipol, the absorption and diuretic effect of furosemide decreases.
When used simultaneously with lithium carbonate, the effects of lithium may be enhanced due to an increase in its concentration in the blood plasma.
When used simultaneously with probenecid, the renal clearance of furosemide decreases.
When used simultaneously with sotalol, hypokalemia and the development of ventricular arrhythmia of the “pirouette” type are possible.
When used simultaneously with theophylline, a change in the concentration of theophylline in the blood plasma is possible.
When used simultaneously with phenytoin, the diuretic effect of furosemide is significantly reduced.
After intravenous administration of furosemide during therapy with chloral hydrate, increased sweating, a feeling of heat, instability of blood pressure, and tachycardia are possible.
When used simultaneously with cisapride, hypokalemia may increase.
It is assumed that furosemide may reduce the nephrotoxic effect of cyclosporine.
When used simultaneously with cisplatin, the ototoxic effect may be enhanced.
Storage conditions
Storage conditions
In a place protected from light, at a temperature not exceeding 20 °C
Shelf life
Shelf life
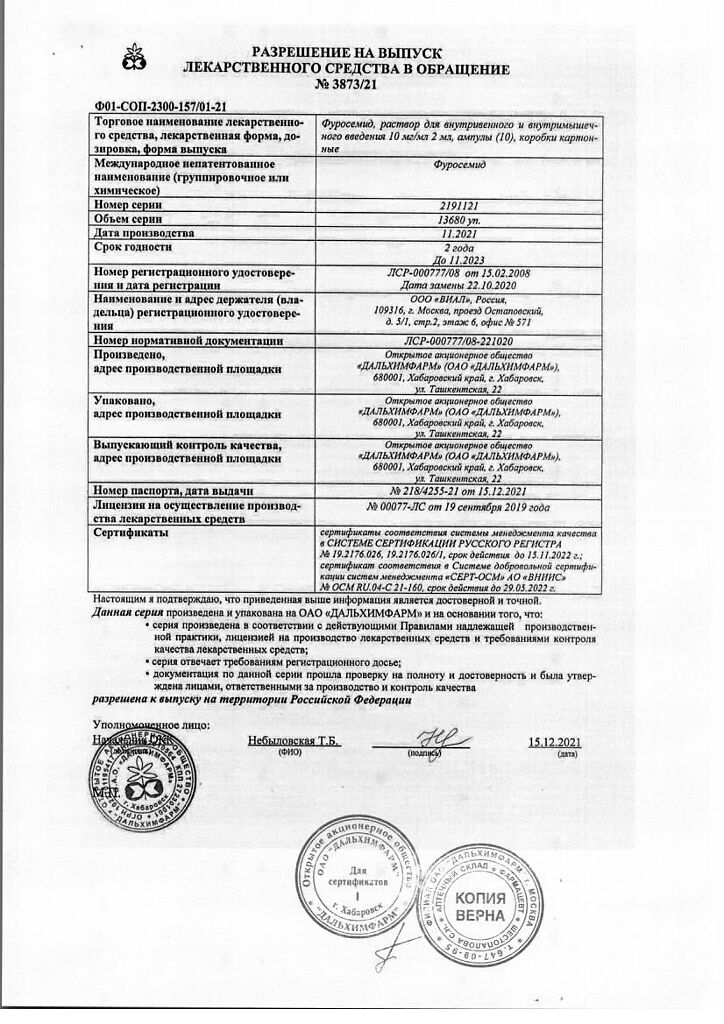
2 years
Manufacturer
Manufacturer
Dalkhimfarm, Russia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a light-protected place, at a temperature not exceeding 20 °C |
| Manufacturer | Dalkhimpharm, Russia |
| Medication form | solution |
| Brand | Dalkhimpharm |
Other forms…
Related products
Buy Furosemide, 10 mg/ml 2 ml 10 pcs with delivery to USA, UK, Europe and over 120 other countries.