No products in the cart.
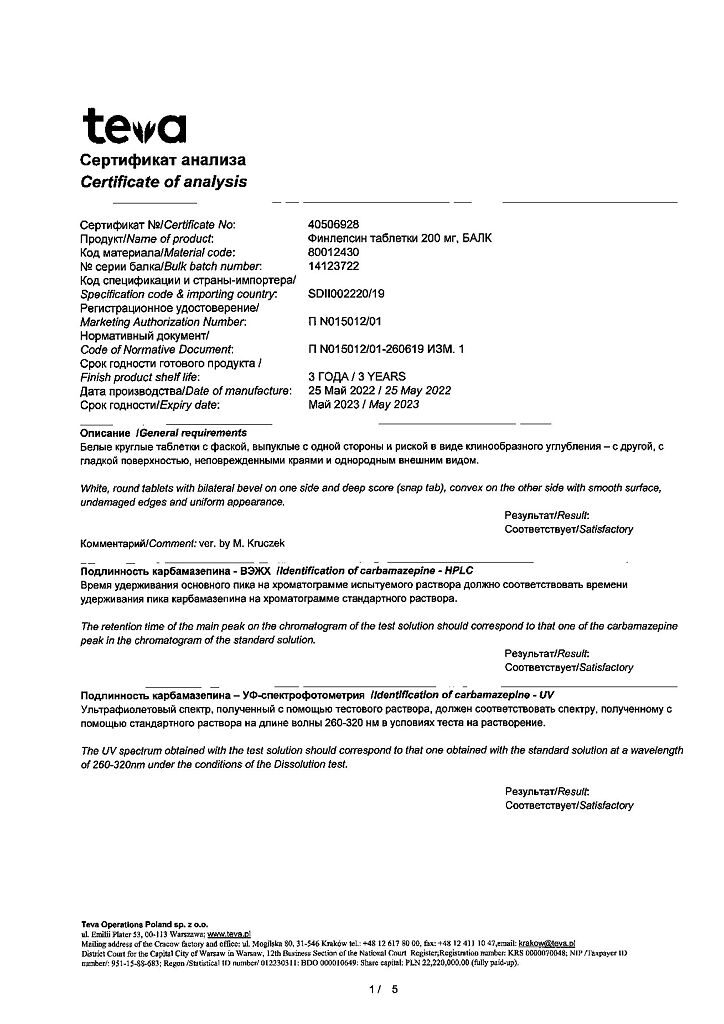
Finlepsin, tablets 200 mg 50 pcs
€8.35 €7.31
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: anti-epileptic drug
ATX code: N03AF01
Pharmacological properties
Mechanism of action Carbamazepine, the active ingredient in Finlepsin®, is a dibenzoazepine derivative. In addition to its antiepileptic effects, the drug also has neurotropic and psychotropic effects. The mechanism of action of carbamazepine has been only partially explained to date. Carbamazepine stabilizes the membranes of overexcited neurons, suppresses serial discharges of neurons and reduces synaptic transmission of excitatory impulses. Probably the main mechanism of action of carbamazepine is to prevent the reappearance of sodium-dependent action potentials in depolarized neurons by blockade of open potential-dependent sodium channels. Pharmacodynamics . When used as monotherapy in patients with epilepsy (especially in children and adolescents), psychotropic effects of the drug were observed, including a positive effect on symptoms of anxiety and depression, as well as reduction of irritability and aggressiveness. There is no unequivocal information about the effect of the drug on cognitive and psychomotor functions: some studies showed a dual or negative effect depending on the dose of the drug, other studies showed a positive effect of the drug on attention and memory. As a neurotropic agent the drug is effective in a number of neurological diseases. For example, in idiopathic and secondary trigeminal neuralgia, it prevents the occurrence of paroxysmal pain attacks. In alcohol withdrawal syndrome the drug increases seizure threshold, which is usually lowered in this condition, and reduces the severity of clinical manifestations of the syndrome, such as hyperexcitability, tremor and gait disturbances. In patients with non-sugar diabetes, the drug reduces diuresis and sense of thirst. As a psychotropic drug the drug is effective in affective disorders, viz: in the treatment of acute manic states, in the maintenance treatment of bipolar affective (manic-depressive) disorders (both in monotherapy and in combination with neuroleptic agents, antidepressants or lithium drugs), in schizoaffective psychosis attacks, in manic seizures where it is used in combination with neuroleptics, and in manic-depressive psychosis with rapid cycles. While decreased glutamate release and neuronal membrane stabilization may account for the antiepileptic effect, the drug’s ability to suppress manic manifestations may be due to inhibition of dopamine and norepinephrine metabolism. Pharmacokinetics absorption . After oral administration, carbamazepine is absorbed almost completely; absorption is relatively slow when the tablet form is taken. After a single dose of carbamazepine the average maximum plasma concentration (Cmah) is reached after 12 hours. After a single oral administration of a 400 mg carbamazepine tablet, the mean Cmah of the unchanged active ingredient is about 4.5 µg/ml. There are no clinically significant differences in the amount of absorbed active ingredient after administration of different oral dosage forms of carbamazepine. When using any dosage form of carbamazepine, food intake does not significantly affect the rate and degree of absorption of carbamazepine. The equilibrium plasma concentration of carbamazepine is reached within 1-2 weeks. Time of its achievement is individual and depends on the degree of autoinduction of liver enzyme systems by carbamazepine, heteroinduction by other, simultaneously used medicinal agents, as well as on patient’s state before the beginning of therapy, drug dose and duration of treatment. There is significant interindividual variation in equilibrium concentration in the therapeutic range: in most patients, these values range from 4 to 12 mcg/mL (17-50 μmol/L). Distribution and binding to plasma proteins The binding of carbamazepine to plasma proteins is 70-80%. The concentration of unchanged carbamazepine in cerebrospinal fluid and saliva is proportional to the proportion of the active substance not bound to plasma proteins (20-30%). The concentration of carbamazepine in breast milk is 25-60% of its concentration in plasma. Carbamazepine penetrates the blood-placental barrier. Taking into account the complete absorption of carbamazepine, the apparent volume of distribution is 0.8-1.9 L/kg. Metabolism Carbamazepine is metabolized in the liver. The main biotransformation pathway is the epoxydiol pathway, resulting in the main metabolites: the 10,11-transdiol derivative and its conjugate with glucuronic acid. The conversion of carbamazepine-10,11-epoxide to carbamazepine-10,11-transdiol in humans occurs with the microsomal enzyme epoxide hydrolase. The content of carbamazepine-10,11-epoxide (active metabolite) is approximately 30% of the plasma concentration of carbamazepine. The main isoenzyme that provides biotransformation of carbamazepine to carbamazepine-10,11-epoxide is cytochrome P450 3A4. These metabolic reactions also produce a minor amount of another metabolite, 9-hydroxy-methyl-10-carbamoylacridan. Other important pathways of carbamazepine metabolism are the formation of various monohydroxylated derivatives under the influence of the UGT2B7 isoenzyme, as well as N-glucuronides. Elimation The elimination half-life of unchanged carbamazepine after a single oral administration of the drug is on average about 36 hours, and after repeated administration of the drug – on average 16-24 hours depending on the duration of treatment (due to autoinduction of the liver monooxygenase system). It has been shown that in patients concomitantly taking other drugs inducing liver enzymes (e.g. phenytoin, phenobarbital) the elimination half-life of carbamazepine is on average 9-10 hours. When carbamazepine-10,11-epoxide is taken orally, its average half-life is about 6 hours. After a single oral dose of 400 mg of carbamazepine, 72% of the taken dose is excreted by the kidneys and 28% through the intestines. About 2% of the administered dose is excreted in the urine as unchanged carbamazepine, about 1% as pharmacologically active 10,11-epoxide metabolite. After a single oral administration 30% of carbamazepine is excreted by the kidneys as end products of the epoxidiol metabolic pathway. Peculiarities of pharmacokinetics in certain groups of patients Children and adolescents . In children, due to the faster excretion of carbamazepine, higher doses of the drug per kilogram of body weight may be required compared to adults. Elderly patients (aged 65 years and older) There is no evidence that the pharmacokinetics of carbamazepine are altered in elderly patients (compared to young adults). Patients with impaired renal or hepatic function There are no data on the pharmacokinetics of carbamazepine in patients with impaired renal or hepatic function to date.
Indications
Indications
Epilepsy:
complex or simple partial epileptic seizures (with or without loss of consciousness) with or without secondary generalization;
generalized tonic-clonic epileptic seizures;
mixed forms of epileptic seizures.
The drug Finlepsin® is usually ineffective for absence seizures and myoclonus epilepsy.
Acute manic states and maintenance therapy of bipolar affective disorders to prevent exacerbations or reduce the clinical manifestations of exacerbations.
Alcohol withdrawal syndrome.
Idiopathic trigeminal neuralgia and trigeminal neuralgia in multiple sclerosis (typical and atypical).
Idiopathic neuralgia of the glossopharyngeal nerve.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antiepileptic drug
ATX code: N03AF01
Pharmacological properties
Mechanism of action
Carbamazepine, the active substance of the drug Finlepsin®, is a dibenzoazepine derivative. Along with antiepileptic, the drug also has neurotropic and psychotropic effects.
The mechanism of action of carbamazepine has so far been only partially explained. Carbamazepine stabilizes the membranes of overexcited neurons, suppresses serial neuronal discharges and reduces synaptic transmission of excitatory impulses. It is likely that the main mechanism of action of carbamazepine is to prevent the re-emergence of sodium-gated action potentials in depolarized neurons by blocking open voltage-gated sodium channels.
Pharmacodynamics
When used as monotherapy in patients with epilepsy (especially children and adolescents), psychotropic effects of the drug were noted, including a positive effect on symptoms of anxiety and depression, as well as a decrease in irritability and aggressiveness. There is no clear data regarding the effect of the drug on cognitive and psychomotor functions: some studies showed a dual or negative effect that depended on the dose of the drug, while other studies showed a positive effect of the drug on attention and memory.
As a neurotropic agent, the drug is effective in a number of neurological diseases. For example, with idiopathic and secondary trigeminal neuralgia, it prevents the occurrence of paroxysmal pain attacks.
In alcohol withdrawal syndrome, the drug increases the threshold of convulsive readiness, which is usually reduced in this condition, and reduces the severity of clinical manifestations of the syndrome, such as increased excitability, tremor, and gait disturbances.
In patients with diabetes insipidus, the drug reduces diuresis and thirst.
As a psychotropic drug, the drug is effective in affective disorders, namely: in the treatment of acute manic states, in the maintenance treatment of bipolar affective (manic-depressive) disorders (both in monotherapy and in combination with neuroleptics, antidepressants or lithium drugs), in attacks of schizoaffective psychosis, in manic attacks, where it is used in combination with antipsychotics, and also in manic-depressive psychosis with rapid cycles.
Although a decrease in glutamate release and stabilization of the neuronal membrane may explain the antiepileptic effect, the drug’s ability to suppress manic symptoms may be due to inhibition of dopamine and norepinephrine metabolism.
Pharmacokinetics
Suction
After oral administration, carbamazepine is absorbed almost completely; when taken in tablet form, absorption is relatively slow. After a single dose of carbamazepine, the average maximum plasma concentration (Cmax) is reached after 12 hours. After a single oral dose of carbamazepine 400 mg tablets, the average Cmax value of the unchanged active substance is about 4.5 μg/ml. There are no clinically significant differences in the amount of absorbed active substance after the use of various dosage forms of carbamazepine for oral administration.
When using any dosage form of carbamazepine, food intake does not significantly affect the rate and extent of absorption of carbamazepine.
The equilibrium concentration of carbamazepine in plasma is achieved within 1-2 weeks. The time to achieve it is individual and depends on the degree of autoinduction of liver enzyme systems by carbamazepine, heteroinduction by other concomitantly used drugs, as well as on the patient’s condition before the start of therapy, the dose of the drug and the duration of treatment. There are significant interindividual differences in steady-state concentrations in the therapeutic range: in most patients these values range from 4 to 12 μg/ml (17-50 μmol/L).
Distribution and binding to plasma proteins
The binding of carbamazepine to plasma proteins is 70-80%. The concentration of unchanged carbamazepine in the cerebrospinal fluid and saliva is proportional to the proportion of the active substance not bound to plasma proteins (20-30%). The concentration of carbamazepine in breast milk is 25-60% of its concentration in blood plasma. Carbamazepine penetrates the blood-placental barrier. Considering the complete absorption of carbamazepine, the apparent volume of distribution is 0.8-1.9 l/kg.
Metabolism
Carbamazepine is metabolized in the liver. The main route of biotransformation is the epoxydiol pathway, resulting in the formation of the main metabolites: the 10,11-transdiol derivative and its conjugate with glucuronic acid. The conversion of carbamazepine-10,11-epoxide to carbamazepine-10,11-transdiol in the human body occurs with the help of the microsomal enzyme epoxide hydrolase.
The content of carbamazepine-10,11-epoxide (active metabolite) is about 30% of the concentration of carbamazepine in blood plasma. The main isoenzyme that ensures the biotransformation of carbamazepine into carbamazepine-10,11-epoxide is cytochrome P450 3A4. As a result of these metabolic reactions, a small amount of another metabolite, 9-hydroxy-methyl-10-carbamoylacridane, is also formed.
Other important pathways of carbamazepine metabolism are the formation, under the influence of the UGT2B7 isoenzyme, of various monohydroxylated derivatives, as well as N-glucuronides.
Removal
The half-life of unchanged carbamazepine after a single oral dose averages about 36 hours, and after repeated doses of the drug – on average 16-24 hours, depending on the duration of treatment (due to autoinduction of the liver monooxygenase system). It has been shown that in patients taking concomitantly other drugs that induce liver enzymes (for example, phenytoin, phenobarbital), the half-life of carbamazepine averages 9-10 hours.
When taken orally, carbamazepine 10,11-epoxide has an average half-life of approximately 6 hours.
After a single oral dose of 400 mg of carbamazepine, 72% of the dose taken is excreted by the kidneys and 28% through the intestines. About 2% of the dose taken is excreted in the urine as unchanged carbamazepine, about 1% as the pharmacologically active 10,11-epoxide metabolite. After a single oral dose, 30% of carbamazepine is excreted by the kidneys in the form of end products of the epoxydiol metabolic pathway. Features of pharmacokinetics in certain groups of patients
Children and teenagers
In children, due to the faster elimination of carbamazepine, higher doses of the drug per kilogram of body weight may be required compared to adults.
Elderly patients (aged 65 years and older)
There is no data indicating that the pharmacokinetics of carbamazepine changes in elderly patients (compared to young adults).
Patients with impaired renal or liver function
There are currently no data on the pharmacokinetics of carbamazepine in patients with impaired renal or hepatic function.
Special instructions
Special instructions
The drug should be taken only under medical supervision.
Patients with mixed forms of epileptic seizures, including absence and myoclonic seizures
The drug is usually ineffective for absence seizures (petit mal) and myoclonic seizures. In patients with mixed forms of epileptic seizures, the drug should be used with caution and only with regular medical supervision (due to a possible increase in seizures). If attacks intensify, Finlepsin® should be discontinued.
Decreased platelet and white blood cell counts
During the use of carbamazepine with varying frequency, a transient or persistent decrease in the number of platelets or leukocytes is observed. However, in most cases these phenomena are transient and usually do not predict the onset of aplastic anemia or agranulocytosis. Before starting treatment, as well as periodically during treatment, a clinical blood test should be performed, including counting the number of platelets and, possibly, reticulocytes, as well as determining the concentration of iron in the blood serum.
Patients should be informed of early signs of toxicity associated with possible hematological disorders, as well as skin and liver symptoms. The patient is informed of the need to immediately consult a doctor in case of adverse reactions such as fever, sore throat, rash, mouth ulcers, unexplained hemorrhages, hemorrhages in the form of petechiae or purpura.
If the number of leukocytes or platelets decreases (or tends to decrease), during drug therapy, the patient should be carefully monitored and the indicators of a comprehensive clinical blood test should be monitored. If signs of significant bone marrow suppression are detected, Finlepsin® should be discontinued.
Dermatological reactions
When using the drug, severe dermatological reactions were very rarely observed, including Stevens-Johnson syndrome and toxic epidermal necrolysis (Lyell’s syndrome).
Finlepsin® should be discontinued immediately and alternative therapy should be selected if signs and symptoms are observed that presumably indicate the development of severe dermatological reactions – for example, Stevens-Johnson syndrome or Lyell’s syndrome. If severe (in some cases life-threatening) skin reactions develop, the patient should be hospitalized in a hospital. In most cases, Stevens-Johnson syndrome and Lyell’s syndrome developed in the first months of drug therapy. These reactions occurred in approximately 1-6 cases per 10,000 people taking the drug for the first time in countries with a predominantly Caucasian population.
Data from a retrospective analysis in Japanese and Northern European patients demonstrated an association between severe skin lesions (Stevens-Johnson syndrome, Lyell’s syndrome, DRESS syndrome, acute generalized exanthematous pustulosis and macular nodular rash) in carriers of the HLA-A*3101 allele of the human leukocyte antigen (HLA) and the use of carbamazepine.
The frequency of the HLA-A*3101 allele may differ among different ethnic groups: about 2-5% in the European population, about 10% in the Japanese. The frequency of occurrence of this allele in the majority of the population of Australia, Asia, Africa and North America is less than 5%, with some exceptions ranging from 5-12%. A frequency of more than 15% has been found in some ethnic groups of South America (Argentina and Brazil), indigenous people of North America (Navajo and Sioux tribes, in Mexico – Sanora Seri), South India (Tamil Nadu), and 10-15% among other indigenous inhabitants of these regions.
When using carbamazepine in possible carriers of the HLA-A*3101 allele (for example, patients of Japanese nationality, Caucasians, Native Americans, Latin Americans, people of southern India and Arabs), it is recommended to carry out genotyping for this allele. The drug should be used in carriers of this allele only if the benefits of therapy outweigh the possible risks.
Patients already receiving carbamazepine are not recommended to undergo genotyping for this allele, since severe skin reactions in most cases were observed in the first months of drug use (regardless of the presence of HLA-A*3101).
According to a retrospective analysis of the use of carbamazepine in patients of Chinese and Thai nationality, there is a correlation between the incidence of Stevens-Johnson syndrome and Lyell’s syndrome and the presence of the HLA-B*1502 allele in the patient’s genome. The frequency of occurrence of this allele in patients of Chinese nationality is 2-12%, in Thai patients it is about 8%.
When carbamazepine was used in patients in the countries of the Asian region (Taiwan, Malaysia, the Philippines), where there is a high prevalence of the HLA-B*1502 allele, an increase in the incidence of Stevens-Johnson syndrome was detected (graded from “very rare” to “rare”). The frequency of distribution of the HLA-B*1502 allele is: in the Philippines and among some groups of the population of Malaysia – more than 15%. The prevalence of the HLA-B*1502 allele in Korea and India is 2% and 6%, respectively. The prevalence of this allele in people of Caucasian, Negroid races, Hispanics, Indians and Japanese is insignificant (< 1%).
These allele frequencies represent the percentage of chromosomes in specific populations that carry the allele. This means that the percentage of patients carrying a copy of the allele on at least one of their two chromosomes is almost twice the frequency of the allele. Thus, the percentage of patients who may be at risk is almost twice the allele frequency.
When using carbamazepine in possible carriers of the HLA-B*1502 allele, it is recommended to carry out genotyping for this allele. The drug should be used in carriers of this allele only if the benefits of therapy outweigh the possible risks. It is not recommended to carry out genotyping in representatives of nationalities in whose population the frequency of occurrence of the specified allele is low.
Patients already receiving carbamazepine are not recommended to undergo genotyping for this allele, since severe skin reactions in most cases were observed in the first months of drug use (regardless of the presence of HLA-B*1502).
It has been shown that identifying patients with the presence of the HLA-B*1502 allele and avoiding the use of carbamazepine in such patients reduces the incidence of carbamazepine-induced Stevens-Johnson syndrome or Lyell’s syndrome.
However, the results of genotyping should not affect the degree of monitoring of the patient’s condition and the doctor’s alertness regarding severe skin reactions. The development of severe skin lesions is possible in patients negative for these alleles. Also, in many cases, in patients positive for the HLA-B*1502 or HLA-A*3101 alleles, the development of severe skin syndromes was not observed when using carbamazepine.
The influence of other factors, such as the dose of anticonvulsants, patient compliance, concomitant therapy with other drugs, concomitant diseases, or the level of control of dermatological reactions, on the incidence and prevalence of severe skin reactions has not been established.
Mild skin reactions, for example, isolated macular or maculopapular exanthema, are in most cases transient and mild, usually disappearing within a few days or weeks with continued treatment or after reducing the dose of the drug. However, since differential diagnosis between early manifestations of severe skin reactions and mild, transient skin rashes can be difficult, if any skin reactions develop, the patient should be under medical supervision (with a view to promptly discontinuing drug therapy if the patient’s condition worsens).
There is a relationship between the presence of the HLA-A*3101 allele in the genome and the development of less severe skin reactions (such as hypersensitivity syndrome to anticonvulsants or mild maculopapular exanthema); such a relationship has not been established for the HLA-B*1502 allele.
Hypersensitivity reactions
With the development of hypersensitivity to carbamazepine, patients may experience various reactions, including DRESS syndrome, delayed multiorgan manifestations of hypersensitivity with the development of fever, skin rash, vasculitis, lymphadenopathy, pseudolymphoma, arthralgia, leukopenia, eosinophilia, hepatosplenomegaly, changes in liver function tests and bile duct destruction syndrome with a decrease in their number, which can occur in any combinations. Damage to other internal organs (including lungs, kidneys, pancreas, myocardium, colon) is also possible.
If manifestations and symptoms of hypersensitivity develop, the drug should be discontinued immediately.
Patients with known hypersensitivity to carbamazepine should be informed of the possibility of developing hypersensitivity reactions to oxcarbazepine in 25-30% of cases.
Hypersensitivity cross-reactions may develop between carbamazepine and aromatic antiepileptic drugs (for example, phenytoin, pyrimidone and phenobarbital).
Hyponatremia
The development of hyponatremia is associated with the use of carbamazepine. In patients with pre-existing renal impairment associated with low serum sodium or in patients receiving concomitant drugs that reduce sodium (eg, diuretics, drugs that affect antidiuretic hormone secretion), serum sodium should be determined before initiating carbamazepine therapy. Thereafter, sodium levels should be determined approximately two weeks later and then monthly for the first three months of therapy, or as clinically necessary. These risk factors are especially common in older patients. If hyponatremia is present, limiting fluid intake is important to determine the condition when clinically indicated.
Hypothyroidism
Carbamazepine may reduce serum concentrations of thyroid hormones through enzyme induction, requiring an increase in the dose of replacement therapy in patients with hypothyroidism. In this category of patients, monitoring of thyroid function is necessary to select the dose of replacement therapy drugs.
Liver dysfunction
Before using the drug Finlepsin® and during treatment, it is necessary to conduct a liver function test, especially in patients with a history of liver disease, as well as in elderly patients. If pre-existing liver dysfunction worsens or if active liver disease develops, Finlepsin® should be discontinued immediately.
Renal dysfunction
Before starting treatment with the drug and periodically during therapy, it is recommended to conduct a general urine test and determine the concentration of urea in the blood.
M-anticholinergic activity
The drug has weak m-anticholinergic activity. Therefore, patients with increased intraocular pressure, prostatic hyperplasia, and urinary retention should be carefully monitored while using these drugs simultaneously.
Mental disorders
Since the use of the drug may exacerbate latent mental disorders, elderly patients should be monitored to identify symptoms such as confusion and psychomotor agitation.
Suicidal behavior or intentions
Cases of suicidal behavior or intent have been reported in patients receiving anticonvulsants for a number of indications. The results of a meta-analysis of randomized placebo-controlled trials showed a small increase in the risk of developing suicidal behavior in patients receiving anticonvulsants. The mechanism of increased suicidal behavior in this category of patients has not been established. Therefore, careful monitoring of symptoms of suicidal behavior and intentions and decisions on appropriate treatment are necessary. Patients (and their caregivers) should be strongly advised to seek medical help if they experience symptoms of suicidal behavior or intent.
Endocrinological disorders
Due to enzyme induction, carbamazepine may weaken the therapeutic effect of oral contraceptives containing estrogens and/or progesterone. Patients with preserved reproductive potential should be advised to use alternative methods of contraception during drug therapy. It has been reported that bleeding from the vagina may occur between menstrual periods when the drug is used simultaneously with hormonal contraceptives (breakthrough bleeding).
Pregnancy and patients with preserved reproductive potential
Use of the drug during pregnancy may be associated with a risk to the fetus (see section “Use during pregnancy and breastfeeding”). The use of the drug during pregnancy is possible only if the expected benefits justify the potential risks.
Pregnant patients and patients with preserved reproductive potential should be fully informed about the risks to the fetus associated with the potential teratogenic effect of carbamazepine (see section “Use during pregnancy and breastfeeding”).
Patients with preserved reproductive potential should use reliable methods of contraception during therapy and for 2 weeks after taking the last dose of the drug (see subsection “Endocrinological disorders”, as well as sections “Interaction with other drugs” and “Use during pregnancy and breastfeeding”).
Determination of carbamazepine concentration in blood plasma
Although the relationship between the dose of the drug, the concentration of carbamazepine in the blood plasma, its clinical effectiveness or tolerability is very small, however, regular determination of the concentration of carbamazepine may be advisable in the following situations: with a sharp increase in the frequency of attacks, in order to check whether the patient is taking the drug properly; during pregnancy; when treating children or adolescents; if there is a suspicion of impaired absorption of carbamazepine; if toxic reactions are suspected if the patient is taking several medications.
Falls
Therapy with the drug was accompanied by ataxia, dizziness, somnolence, hypotension, confusion, sedation (see section “Side effects”), which can lead to falls and, as a result, fractures or other injuries. In patients with concomitant diseases, conditions, or those receiving concomitant drug therapy with drugs that may exacerbate the above effects, the risk of falling should be regularly assessed during long-term drug therapy.
Impact on the ability to drive vehicles and machinery
The ability of a patient taking Finlepsin® to respond quickly, especially at the beginning of therapy or during dose titration, may be impaired due to both the disease itself (for example, seizures) and due to side effects such as dizziness, drowsiness, ataxia, diplopia, impaired accommodation and visual impairment. Patients should be warned about possible dangers when driving vehicles and working with machinery.
Active ingredient
Active ingredient
Carbamazepine
Composition
Composition
1 tablet contains: active ingredient carbamazepine 200.00 mg; excipients: microcrystalline cellulose (type 12), gelatin, croscarmellose sodium, magnesium stearate.
Pregnancy
Pregnancy
Pregnancy
Summary of Risks
Carbamazepine quickly crosses the blood-placental barrier and is found in high concentrations in fetal tissues, especially in the liver and kidneys.
Children of patients with epilepsy are more often than others predisposed to developmental disorders, including congenital defects. Despite the lack of convincing data from controlled studies on the presence of a cause-and-effect relationship between these disorders and carbamazepine monotherapy in the mother, with the use of the drug there have been reports of cases of congenital diseases and malformations, including spina bifida and other congenital anomalies: developmental defects of craniofacial structures, cardiovascular and other organ systems, hypospadias.
According to the North American Pregnancy Registry, the incidence of gross malformations, defined as structural abnormalities requiring surgical, medical, or cosmetic correction, diagnosed within 12 weeks after birth was 3.0% in mothers taking carbamazepine monotherapy in the first trimester and 1.1% in mothers not taking any antiepileptic drugs.
Clinical significance
Treatment with Finlepsin® in pregnant women with epilepsy should be carried out with extreme caution.
If it is necessary to use the drug in pregnant women, as well as if pregnancy is diagnosed during use of the drug, or the patient is planning a pregnancy, the ratio of expected benefits and possible risks should be carefully assessed, especially in the first trimester of pregnancy.
If there is sufficient clinical efficacy in patients with preserved reproductive potential, Finlepsin® should be used in monotherapy, since the incidence of congenital fetal anomalies with combination antiepileptic therapy is higher than with monotherapy with these drugs. Depending on the drugs used in combination therapy, the risk of birth defects may be increased, especially when valproate is added to therapy.
Finlepsin® should be used in the minimum effective dose. Regular monitoring of the concentration of the active substance in the blood plasma is recommended. When anticonvulsant control is effective in a pregnant woman, carbamazepine plasma concentrations should be maintained to a minimum (therapeutic range 4-12 mcg/mL), as there are reports of a possible dose-related risk of birth defects (for example, the incidence of birth defects with doses less than 400 mg per day was lower than with higher doses).
Patients should be informed about the possibility of an increased risk of developmental defects and the need, in this regard, for antenatal diagnosis.
During pregnancy, effective antiepileptic treatment should not be interrupted, since progression of the disease can have a negative effect on the mother and the fetus.
Control and prevention
It is known that folic acid deficiency develops during pregnancy. Antiepileptic drugs have been reported to exacerbate these deficits. This may contribute to an increased incidence of birth defects in children born to women taking antiepileptic drugs. In connection with the above, supplemental intake of folic acid is recommended before and during pregnancy.
In order to prevent increased bleeding in newborns, women in the last weeks of pregnancy, as well as in newborns, are recommended to use vitamin K1.
Newborns
Several cases of epileptic seizures and/or respiratory depression have been described in newborns whose mothers took the drug simultaneously with other anticonvulsants. In addition, several cases of vomiting, diarrhea and/or malnutrition have also been reported in newborns whose mothers received the drug. It is possible that these reactions represent neonatal withdrawal symptoms.
Preclinical data
According to summarized data from various preclinical studies in animals (mice, rats, rabbits) when used in doses corresponding to those used in humans, carbamazepine has low or no teratogenic potential. However, data from preclinical studies were insufficient to exclude the teratogenic effect of carbamazepine. In a study of reproductive toxicity when using the drug in lactating rats at a dose of 192 mg/kg per day, a slowdown in body weight gain in offspring was noted.
Breast-feeding
Carbamazepine passes into breast milk, where its concentration is 25-60% of the concentration in blood plasma. In connection with the above, if it is necessary to use the drug during breastfeeding, the ratio of the expected benefits of breastfeeding to the possible risk of developing side effects of the drug should be carefully assessed. Newborns receiving breast milk should be monitored for side effects (eg, severe drowsiness, allergic skin reactions) as early as possible. Cases of cholestatic hepatitis have been described in newborns who received carbamazepine antenatally or through breast milk, and therefore such newborns should be monitored for the earliest possible diagnosis of side effects from the hepatobiliary system.
Contraception
Patients with preserved reproductive potential should use reliable methods of contraception during therapy and for 2 weeks after taking the last dose of the drug. Due to enzyme induction, carbamazepine may weaken the therapeutic effect of oral contraceptives containing estrogens and/or progesterone. Patients with preserved reproductive potential should be advised to use alternative methods of contraception during drug therapy.
Effect on reproductive potential
There have been very rare reports of decreased male fertility and/or impaired spermatogenesis.
Contraindications
Contraindications
Hypersensitivity to carbamazepine or chemically similar drugs (for example, tricyclic antidepressants) or to any other component of the drug.
Atrioventricular block.
A history of episodes of suppression of bone marrow hematopoiesis.
Hepatic porphyrias (eg, acute intermittent porphyria, porphyria cutanea tarda, variegated porphyria).
Use in combination with monoamine oxidase inhibitors (MAOIs, structurally similar to tricyclic antidepressants).
Children under 4 years of age (in patients of this category, the drug should be used in a different dosage form).
With caution
In patients with a history of heart disease (including decompensated chronic heart failure), liver disease (including liver failure), kidney disease (including renal failure), adverse hematological reactions to other drugs, or discontinuation of previous treatment with carbamazepine, therapy should be carried out only after a careful analysis of the relationship between the expected effect of treatment and the possible risk of therapy with careful regular monitoring of the patient’s condition.
The drug should be used with caution in patients:
with dilution hyponatremia, hypothyroidism;
elderly patients (taking into account the possibility of drug interactions and different pharmacokinetics of antiepileptic drugs);
with mixed forms of epileptic seizures, including absence, typical or atypical, and myoclonic seizures (taking into account the possible intensification of seizures);
with increased intraocular pressure, urinary retention and prostatic hyperplasia, given the weak m-anticholinergic activity of carbamazepine;
receiving anticonvulsants;
in carriers of the HLA-A*3101 and HLA-B*1502 alleles;
during pregnancy and during breastfeeding (see section “Use during pregnancy and during breastfeeding”).
Side Effects
Side Effects
Certain types of adverse reactions (AR), for example, from the central nervous system (dizziness, headache, ataxia, drowsiness, fatigue, diplopia), from the digestive system (nausea, vomiting), as well as allergic skin reactions, occur very often or frequently, especially at the beginning of treatment with the drug, or when using an excessively high initial dose of the drug, or when treating elderly patients.
Dose-related adverse events usually resolve within a few days, either spontaneously or after a temporary dose reduction. The development of adverse reactions from the central nervous system may be a consequence of a relative overdose of the drug or significant fluctuations in the concentration of the active substance in the blood plasma. In such cases, it is recommended to monitor the concentration of the active substance in the blood plasma.
Adverse drug reactions (ADRs) are grouped according to the MedDRA classification of organs and organ systems, and within each group they are listed in order of decreasing frequency of occurrence. Within each group, the frequencies of occurrence of ADRs are indicated in order of decreasing importance.
When assessing the frequency of occurrence of various ADRs, the following gradations were used: “very often” – ≥1/10, “often” – ≥1/100 – < 1/10, “infrequently” - ≥1/1000 - < 1/100 “rarely” - ≥1/10000 - < 1/1000, “very rare” - < 1/10000, including including individual messages.
Mental disorders: rarely – hallucinations (visual or auditory), depression, aggression, anxiety, agitation, confusion; very rarely – activation of psychosis.
Nervous system disorders: very often – ataxia, dizziness, somnolence; often – diplopia, headache; uncommon – abnormal involuntary movements (for example, tremor, fluttering tremor (asterixis), muscular dystonia, tic), nystagmus; rarely – dyskinesia, oculomotor disorders, speech disorders (for example, dysarthria, slurred speech), choreoathetosis, peripheral neuropathy, paresthesia, paresis; very rarely – neuroleptic malignant syndrome, aseptic meningitis with myoclonus and peripheral eosinophilia, dysgeusia.
Disorders of the skin and subcutaneous tissues: very often – urticaria, which can be significantly pronounced, allergic dermatitis; infrequently – exfoliative dermatitis; rarely – systemic lupus erythematosus, skin itching; very rarely – Stevens-Johnson syndrome (classified as “rare” in some Asian countries), toxic epidermal necrolysis (Lyell’s syndrome), photosensitivity reactions, erythema multiforme, erythema nodosum, skin pigmentation disorders, purpura, acne, hyperhidrosis, alopecia, hirsutism.
Disorders of the blood and lymphatic system: very often – leukopenia; often – thrombocytopenia, eosinophilia; rarely – leukocytosis, lymphadenopathy; very rarely – agranulocytosis, aplastic anemia, pancytopenia, true erythrocyte aplasia, anemia, megaloblastic anemia, reticulocytosis, hemolytic anemia.
While taking the drug, agranulocytosis and aplastic anemia may develop. However, because these conditions occur so rarely, it is difficult to quantify the risk of their occurrence. It is known that the total risk of developing agranulocytosis in the general untreated population is 4.7 cases per 1 million population per year, and aplastic anemia is 2.0 cases per 1 million population per year.
Disorders of the digestive system: very often – nausea, vomiting; often – dry mouth; infrequently – diarrhea, constipation; rarely – abdominal pain; very rarely – glossitis, stomatitis, pancreatitis.
Disorders of the liver and biliary tract: rarely – hepatitis of cholestatic, parenchymal (hepatocellular) or mixed type, destruction of intrahepatic bile ducts with a decrease in their number, jaundice; very rarely – liver failure, granulomatous liver damage.
Immune system disorders: rarely – multiorgan delayed-type hypersensitivity with fever, skin rashes, vasculitis, lymphadenopathy, pseudolymphoma, arthralgia, leukopenia, eosinophilia, hepatosplenomegaly and altered liver function tests and destruction of intrahepatic bile ducts with a decrease in their number (these manifestations occur in various combinations). Other organs may also be involved (eg, lungs, kidneys, pancreas, myocardium, colon); very rarely – anaphylactic reaction, angioedema, hypogammaglobulinemia. If the above hypersensitivity reactions occur, use of the drug should be discontinued.
Cardiac disorders: rarely – intracardiac conduction disorders; very rarely – arrhythmia, atrioventricular block with fainting, bradycardia, chronic heart failure, exacerbation of coronary heart disease.
Vascular disorders: rarely – arterial hypertension or hypotension; very rarely – circulatory collapse, thrombophlebitis, thromboembolism (for example, pulmonary embolism).
Endocrine system disorders: often – edema, fluid retention, weight gain, hyponatremia and a decrease in blood osmolarity due to an effect similar to the action of antidiuretic hormone, which in rare cases leads to water intoxication (dilution hyponatremia), accompanied by lethargy, vomiting, headache, disorientation and neurological disorders; very rarely – galactorrhea, gynecomastia.
Metabolic and nutritional disorders: rarely – folic acid deficiency, loss of appetite; very rarely – acute porphyria (acute intermittent porphyria and mixed porphyria), non-acute porphyria (late cutaneous porphyria).
Renal and urinary tract disorders: very rarely – tubulointerstitial nephritis, renal failure, renal dysfunction (for example, albuminuria, hematuria, oliguria, increased blood urea concentration/azotemia), urinary retention, frequent urination.
Disorders of the genital organs and mammary gland: very rarely – sexual dysfunction/erectile dysfunction, impaired spermatogenesis (decreased sperm count and motility).
Violations of the organ of vision: often – disturbance of accommodation (including blurred vision); very rarely – clouding of the lens, conjunctivitis.
Hearing disorders and labyrinthine disorders: very rarely – hearing disorders, incl. tinnitus, hyperacusis, hypoacusia, changes in the perception of pitch.
Musculoskeletal and connective tissue disorders: rarely – muscle weakness; very rarely – disorders of bone metabolism (decreased calcium and 25-hydroxycholecalciferol levels in the blood plasma, leading to osteomalacia/osteoporosis), arthralgia, myalgia and muscle spasm.
Disorders of the respiratory system, chest and mediastinal organs: very rarely – hypersensitivity reactions characterized by fever, shortness of breath, pneumonitis or pneumonia.
General disorders and disorders at the injection site: very often – increased fatigue.
Laboratory and instrumental data: very often – increased activity of gamma-glutamyltransferase (due to induction of liver enzymes), which usually has no clinical significance; often – increased activity of blood alkaline phosphatase; infrequently – increased transaminase activity; very rarely – increased intraocular pressure, increased concentrations of cholesterol, including high-density lipoprotein cholesterol and triglycerides, changes in thyroid function indicators – decreased concentrations of L-thyroxine (free and bound fraction) and triiodothyronine, increased concentrations of thyroid-stimulating hormone, which is usually not accompanied by clinical manifestations, increased concentrations of prolactin in the blood.
Adverse events identified in the post-registration period (reports were received from a population of unknown size, as a result of which the frequency of occurrence cannot be determined, “frequency unknown”):
Infectious and parasitic diseases: reactivation of herpes simplex virus type 6. Blood and lymphatic system disorders: bone marrow failure.
Injuries, intoxications and complications of manipulations: falls (associated with ataxia, dizziness, somnolence, arterial hypotension, confusion, sedation caused by taking the drug).
Nervous system disorders: sedation, memory impairment.
Gastrointestinal disorders: colitis.
Immune system disorders: drug rash with eosinophilia and systemic manifestations (DRESS syndrome).
Skin and subcutaneous tissue disorders: acute generalized exanthematous pustulosis, lichenoid keratosis, onychomadesis.
Musculoskeletal and connective tissue disorders: bone fracture.
Laboratory and instrumental data: decreased bone density.
If any of the side effects indicated in the instructions get worse, or you notice any other side effects not listed in the instructions, tell your doctor.
Interaction
Interaction
Carbamazepine is not recommended for use simultaneously with MAO inhibitors. Before using the drug, MAO inhibitors should be discontinued at least 2 weeks or earlier if the clinical situation allows.
Cytochrome P4503A4 (CYP3A4) is the main isoenzyme that provides the formation of carbamazepine-10,11-epoxide (active metabolite). Concomitant use of CYP3A4 isoenzyme inhibitors with the drug may lead to an increase in the concentration of carbamazepine in the blood plasma, which, in turn, can cause adverse reactions. The simultaneous use of inducers of the CYP3A4 isoenzyme may lead to an acceleration of the metabolism of carbamazepine and, thus, to a possible decrease in its plasma concentration and, consequently, to a possible decrease in the severity of the therapeutic effect of the drug. Cancellation of concomitantly taken inducers of the CYP3A4 isoenzyme may reduce the rate of biotransformation of carbamazepine, and, as a result, lead to an increase in the concentration of carbamazepine in the blood plasma.
Carbamazepine is a powerful inducer of the CYP3A4 isoenzyme and other hepatic enzyme systems of the first and second phases of drug metabolism, and when used simultaneously with drugs metabolized by the CYP3A4 isoenzyme, it can cause induction of metabolism and a decrease in their concentration in the blood plasma.
Since the conversion of carbamazepine-10,11-epoxide to carbamazepine-10,11-transdiol occurs with the help of microsomal epoxide hydrolase, the use of carbamazepine simultaneously with inhibitors of microsomal epoxide hydrolase may lead to an increase in the plasma concentration of carbamazepine-10,11-epoxide.
Drugs that may increase plasma concentrations of carbamazepine:
analgesic and non-steroidal anti-inflammatory drugs: dextropropoxyphene, ibuprofen;
antitumor agents (androgen): danazol;
antibiotics: macrolides (for example, erythromycin, troleandomycin, josamycin, clarithromycin), ciprofloxacin;
antidepressants: possibly desipramine, fluoxetine, fluvoxamine, nefazodone, paroxetine, trazodone, viloxazine;
antiepileptic drugs: stiripentol, vigabatrin;
antifungals: azole derivatives (for example, itraconazole, ketoconazole, fluconazole, voriconazole). Alternative anticonvulsants may be recommended in patients receiving voriconazole or itraconazole;
histamine H2 receptor blockers: loratadine, terfenadine;
antipsychotics (neuroleptics): olanzapine;
antituberculosis drugs: isoniazid;
antivirals: HIV protease inhibitors (for example, ritonavir);
antiglaucoma agents (carbonic anhydrase inhibitors): acetazolamide;
antihypertensive drugs (blockers of “slow” calcium channels): verapamil, diltiazem;
antiulcer drugs (proton pump inhibitors, histamine H2 receptor blockers): omeprazole, possibly cimetidine;
muscle relaxants: oxybutynin, dantrolene;
antiplatelet agents: ticlopidine;
other medicines and foods: grapefruit juice, nicotinamide (only in high doses).
Since an increase in the concentration of carbamazepine in the blood plasma can lead to adverse reactions (for example, dizziness, drowsiness, ataxia, diplopia), in these situations the dose of the drug should be adjusted and/or the concentration of carbamazepine in the blood plasma should be regularly determined.
Drugs that may increase plasma concentrations of carbamazepine 10,11-epoxide: loxapine, quetiapine, primidone, progabide, valproic acid, valnoctamide and valpromide.
Since an increase in the concentration of carbamazepine-10,11-epoxide in the blood plasma can lead to adverse reactions (for example, dizziness, drowsiness, ataxia, diplopia), in these situations the dose of the drug should be adjusted and/or the concentration of carbamazepine-10,11-epoxide in the blood plasma should be regularly determined.
Drugs that may reduce plasma concentrations of carbamazepine:
antiepileptic drugs: felbamate, mesuximide, oxcarbazepine, phenobarbital, phensuximide, phenytoin (to avoid phenytoin intoxication and the occurrence of subtherapeutic concentrations of carbamazepine, the recommended plasma concentration of phenytoin should be no more than 13 mcg/ml before adding carbamazepine to therapy) and fosphenytoin, primidone, and, although the data are partially contradictory, possibly also clonazepam.
antitumor agents: cisplatin or doxorubicin;
antituberculosis drugs: rifampicin;
bronchodilators: theophylline, aminophylline;
acne treatment (retinoids): isotretinoin;
other medicines and food products: herbal preparations containing St. John’s wort.
When used simultaneously with the above drugs, a dose adjustment of carbamazepine may be required.
Effect of carbamazepine on plasma concentrations of drugs used as concomitant therapy
When used concomitantly with carbamazepine, plasma concentrations may decrease, the effect of some drugs may decrease, or even completely cease, and therefore the need to adjust the dose of the following drugs should be taken into account in accordance with clinical recommendations:
analgesic and non-steroidal anti-inflammatory drugs: buprenorphine, methadone, paracetamol (long-term use of carbamazepine and paracetamol (acetaminophen) can lead to the development of hepatotoxic effects), phenazone, tramadol;
antibiotics of the tetracycline group: doxycycline, rifabutin;
anticoagulants: oral anticoagulants (for example, warfarin, phenprocoumon, dicumarol and acenocoumarol, rivaroxaban, dabigatran, apixaban, edoxaban);
antidepressants: bupropion, citalopram, mianserin, nefazodone, sertraline, trazodone, tricyclic antidepressants (imipramine, amitriptyline, nortriptyline, clomipramine);
antiemetics: aprepitant;
antiepileptic drugs: clobazam, clonazepam, eslicarbazepine, ethosuximide, felbamate, lamotrigine, eslicarbazepine, oxcarbazepine, primidone, tiagabine, topiramate, valproic acid, zonisamide. To avoid phenytoin toxicity and the occurrence of subtherapeutic concentrations of carbamazepine, the recommended plasma concentration of phenytoin should be no more than 13 mcg/ml before adding carbamazepine to therapy. There are reports that while taking carbamazepine, the concentration of mephenytoin in the blood plasma may increase (in rare cases).
antifungals: itraconazole, voriconazole. Alternative anticonvulsants may be recommended in patients receiving voriconazole or itraconazole;
anthelmintics: praziquantel, albendazole;
antitumor agents: imatinib, cyclophosphamide, lapatinib, temsirolimus;
antipsychotics (neuroleptics): clozapine, haloperidol, bromperidol, olanzapine, quetiapine, risperidone, ziprasidone, aripiprazole, paliperidone;
antivirals: HIV protease inhibitors (indinavir, ritonavir, saquinavir);
anxiolytics: alprazolam, midazolam;
bronchodilators: theophylline;
contraceptives: hormonal contraceptives (selection of alternative methods of contraception is necessary);
drugs for the treatment of diseases of the cardiovascular system: blockers of “slow” calcium channels of the dihydropyridine group (felodipine); simvastatin, atorvastatin, lovastatin, cerivastatin, ivabradine;
cardiac glycosides: digoxin;
glucocorticosteroids: prednisolone, dexamethasone;
drugs for the treatment of erectile dysfunction: tadalafil;
immunosuppressive drugs: cyclosporine, everolimus, tacrolimus, sirolimus;
drugs for the treatment of thyroid diseases: levothyroxine;
other medicines and foods: preparations containing estrogens and/or progesterone.
Combinations to Consider
With the simultaneous use of carbamazepine with levetiracetam, in some cases an increase in the toxic effect of carbamazepine was observed.
There are reports of increased hepatotoxicity caused by isoniazid in cases where it was used concomitantly with carbamazepine.
The combined use of carbamazepine and lithium or metoclopramide, as well as carbamazepine and antipsychotic drugs (haloperidol, thioridazine) can lead to an increase in the frequency of adverse neurological reactions (in the case of the latter combination, even at therapeutic concentrations of active substances in the blood plasma).
The simultaneous use of carbamazepine with some diuretics (hydrochlorothiazide, furosemide) can lead to hyponatremia, accompanied by clinical manifestations.
Carbamazepine may antagonize the action of non-depolarizing muscle relaxants (eg, pancuronium bromide). If such a combination of drugs is used, it may be necessary to increase the dose of these muscle relaxants; Patients should be monitored carefully as the effects of muscle relaxants may cease more quickly than expected.
It has been reported that bleeding from the vagina may occur between menstrual periods when the drug is used simultaneously with hormonal contraceptives (breakthrough bleeding). The drug may reduce the effect of hormonal contraceptives due to the induction of microsomal enzymes.
Carbamazepine, like other psychotropic drugs, can reduce alcohol tolerance. In this regard, the patient is advised to stop drinking alcohol.
The simultaneous use of carbamazepine and direct oral anticoagulants (for example, rivaroxaban, dabigatran, apixaban, edoxaban) may lead to a decrease in the concentration of the direct oral anticoagulant in the blood plasma, which leads to the risk of thrombosis. Therefore, if concomitant use of these drugs is necessary, be alert for signs and symptoms of thrombosis.
Impact on serological studies
Carbamazepine may lead to a false-positive result in determining the concentration of perphenazine using high-performance liquid chromatography.
Carbamazepine and carbamazepine 10,11-epoxide may cause a false-positive result in determining tricyclic antidepressant concentrations by polarization fluorescence immunoassay.
Overdose
Overdose
An overdose is usually manifested by symptoms from the central nervous system, cardiovascular and respiratory systems, as well as the phenomena listed in the “Side Effects” section.
In case of overdose, the following symptoms and complaints are possible.
Central nervous system: depression of central nervous system functions; disturbance of consciousness, disorientation, drowsiness, agitation, hallucinations, coma; blurred vision, slurred speech, dysarthria, nystagmus, ataxia, dyskinesia, hyperreflexia (early), hyporeflexia (later); convulsions, psychomotor disorders, myoclonus, hypothermia, mydriasis.
Respiratory system: respiratory depression, pulmonary edema.
Cardiovascular system: tachycardia, arterial hypotension or, in some cases, arterial hypertension, conduction disturbances with widening of the QRS complex; cardiac arrest and fainting caused by cardiac arrest.
Digestive system: vomiting, delayed passage of food from the stomach, decreased colonic motility.
Urinary system: urinary retention, oliguria or anuria; fluid retention; water intoxication (dilution hyponatremia), caused by the effect of carbamazepine, similar to the effect of antidiuretic hormone.
Musculoskeletal system: There are reports of rhabdomyolysis associated with the use of carbamazepine.
Changes in laboratory parameters: hyponatremia, possible metabolic acidosis, possible hyperglycemia, increased activity of the muscle fraction of creatine phosphokinase.
Treatment
There is no specific antidote. Initial treatment should be based on the patient’s clinical condition; hospitalization is indicated. The concentration of carbamazepine in plasma is determined to confirm poisoning with this drug and assess the degree of overdose.
Evacuation of stomach contents, gastric lavage, and use of activated carbon are carried out. Late evacuation of gastric contents can lead to delayed absorption and reappearance of symptoms of intoxication during the recovery period. Symptomatic supportive treatment is used in the intensive care unit, monitoring of cardiac functions, and careful correction of water and electrolyte imbalances.
It is recommended to carry out hemosorption on carbon sorbents. Hemodialysis is an effective treatment for carbamazepine overdose. It is possible that the symptoms of overdose may re-intensify on the 2nd and 3rd day after its onset, which is due to the slow absorption of carbamazepine.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Manufacturer
Manufacturer
Teva Operations Poland Sp. z o.o., Poland
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | Store at the temperature not more than 25 °С. Keep out of reach of children. |
| Manufacturer | Teva Operations Poland Sp. z o.o., Poland |
| Medication form | pills |
| Brand | Teva Operations Poland Sp. z o.o. |
Related products
Buy Finlepsin, tablets 200 mg 50 pcs with delivery to USA, UK, Europe and over 120 other countries.