No products in the cart.
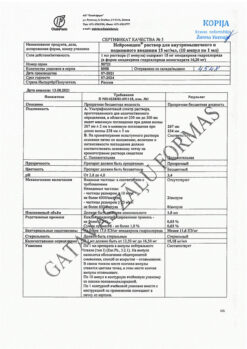
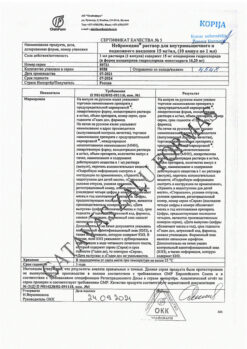
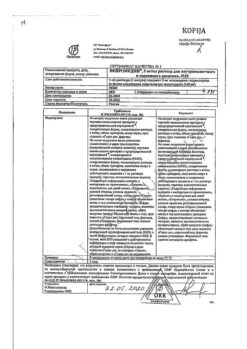
Excitalopram-ALSI, 10 mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group:antidepressant
ATX code: N06AB10
Pharmacological Properties.
Pharmacodynamics:
Escitalopram is an antidepressant, a selective serotonin reuptake inhibitor (SSRI) with high affinity for the primary active center. Escitalopram also binds to the allosteric center of the serotonin transporter protein with an affinity 1000 times lower. Allosteric modulation of the transporter protein enhances the binding of escitalopram at the primary binding site, resulting in a more complete inhibition of serotonin reuptake.
Escitalopram has no or very weak ability to bind to a number of receptors, including: Serotonin 5-HT1A, 5-HT2 receptors, dopamine D1 and D2 receptors, α1-, α2-, β-adrenergic receptors, histamine H1, muscarinic cholinergic, benzodiazepine and opiate receptors.
The inhibition of 5-NT reuptake is the only possible mechanism of action that explains the pharmacological and clinical effects of escitalopram.
Escitalopram is the S-enantiomer of racemic citalopram with intrinsic therapeutic activity. The R-enantiomer has been shown not to be inert but to counteract the serotonergic properties and corresponding pharmacological effects of the S-enantiomer‑.
Pharmacokinetics:
Eabsorption
The absolute bioavailability of escitalopram is 80% and is independent of food intake. The maximum concentration (Cmax) in plasma is reached on average 4 hours after multiple administration.
Distribution
The estimated volume of distribution after oral administration is 12 to 26 L/kg. The binding of escitalopram to human plasma proteins is not more than 80% (on average about 56%). It penetrates into the breast milk.
Metabolism
Escitalopram is metabolized in the liver to demethylated and didemethylated metabolites. They are both pharmacologically active. Nitrogen can be oxidized to the metabolite N-oxide. The main substance and its metabolites are partially excreted as glucuronides. After multiple uses, the average concentration of demethyl and didemethyl metabolites is usually 28-31% and less than 5%, respectively, of the concentration of escitalopram. The biotransformation of escitalopram to a demethylated metabolite occurs primarily via the CYP2C19 isoenzyme. Some involvement of CYP3A4 and CYP2D6 isoenzymes is possible.
Elimation
The half-life (T1/2) of escitalopram after multiple uses is about 30 hours. Total clearance with oral administration is about 0.6 l/min. The main metabolites of escitalopram have a longer elimination half-life.
Escitalopram and its metabolites are excreted both via the liver (metabolic route) and the kidneys, with most of the administered dose excreted as metabolites in the urine.
Linearity of pharmacokinetics
The pharmacokinetics of escitalopram are linear dose-dependent. The equilibrium plasma concentration (Css) is established after approximately 1 week of therapy. An average equilibrium concentration of 50 nmol/L (range 20 to 125 nmol/L) is reached at a daily dose of 10 mg.
Patients over 65 years of age
The elderly (over 65 years) have a longer half-life and lower clearance values compared to younger patients. The amount of escitalopram in the systemic bloodstream, calculated using the area under the curve (AUC) pharmacokinetic index, is 50% greater in the elderly than in young healthy volunteers.
Patients with impaired liver function
In patients with mild to moderate hepatic impairment (Child-Pugh class A and B), T1/2 escitalopram is approximately twice as long and the AUC is 60% longer than in patients with normal liver function.
Patients with impaired renal function
. When racemic citalopram is used in patients with renal impairment (creatinine clearance 10-53 ml/min), there is a prolongation of T1/2 and a slight increase in AUC. Plasma concentrations of metabolites have not been studied, but they may be elevated.
Patients with low isoenzyme activity CYP2C19
Persons with weak CYP2C19 activity have twice the concentration of escitalopram as those with high activity of this isoenzyme. No significant changes in drug concentrations were found in cases with weak CYP2D6 isoenzyme activity.
Indications
Indications
Depressive episodes of any severity.
Panic disorders with/without agoraphobia.
Obsessive-compulsive disorder.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antidepressant
ATX code: N06AB10
PHARMACOLOGICAL PROPERTIES
Pharmacodynamics:
Escitalopram is an antidepressant, a selective serotonin reuptake inhibitor (SSRI) with high affinity for the primary active site. Escitalopram also binds to the allosteric site of the serotonin transporter protein with 1000-fold lower affinity. Allosteric modulation of the transporter protein enhances the binding of escitalopram at the primary binding site, resulting in more complete inhibition of serotonin reuptake.
Escitalopram has no or very weak ability to bind to a number of receptors, including: serotonin 5-HT1A, 5-HT2 receptors, dopamine D1 and D2 receptors, α1-, α2-, β-adrenergic receptors, histamine H1, muscarinic cholinergic, benzodiazepine and opiate receptors.
Inhibition of 5-HT reuptake is the only possible mechanism of action that explains the pharmacological and clinical effects of escitalopram.
Escitalopram is the S-enantiomer of racemic citalopram with its own therapeutic activity. The R-enantiomer has been shown not to be inert, but to counteract the serotonergic properties and corresponding pharmacological effects of the S-enantiomer.
Pharmacokinetics:
Suction
The absolute bioavailability of escitalopram is 80% and is independent of food intake. The maximum concentration (Cmax) in plasma is achieved on average 4 hours after repeated use.
Distribution
The apparent volume of distribution after oral administration ranges from 12 to 26 L/kg. The binding of escitalopram to human plasma proteins is no more than 80% (on average about 56%). Passes into breast milk.
Metabolism
Escitalopram is metabolized in the liver to demethylated and didemethylated metabolites. They are both pharmacologically active. Nitrogen can be oxidized to the N-oxide metabolite. The main substance and its metabolites are partially released in the form of glucuronides. After repeated use, the average concentration of demethyl and didemethyl metabolites is usually 28-31% and less than 5%, respectively, of the concentration of escitalopram. Biotransformation of escitalopram into a demethylated metabolite occurs mainly with the help of the CYP2C19 isoenzyme. Some participation of CYP3A4 and CYP2D6 isoenzymes is possible.
Removal
The half-life (T1/2) of escitalopram after repeated use is approximately 30 hours. The total clearance when administered orally is about 0.6 l/min. The main metabolites of escitalopram have a longer half-life.
Escitalopram and its metabolites are eliminated through both the liver (metabolic route) and the kidneys, with the majority of the administered dose being excreted as metabolites in the urine.
Linearity of pharmacokinetics
The pharmacokinetics of escitalopram is linear and dose-dependent. Steady-state plasma concentration (Css) is established after approximately 1 week of therapy. A mean steady-state concentration of 50 nmol/L (range 20 to 125 nmol/L) is achieved with a daily dose of 10 mg.
Patients over 65 years of age
Elderly patients (over 65 years of age) have a longer half-life and lower clearance values compared to younger patients. The amount of escitalopram in the systemic circulation, calculated using the pharmacokinetic indicator “area under the curve” (AUC), is 50% greater in the elderly than in young healthy volunteers.
Patients with liver dysfunction
In patients with mild or moderate hepatic impairment (Child-Pugh class A and B), the T1/2 half of escitalopram is approximately 2 times longer and the AUC is 60% greater than in patients with normal liver function.
Patients with impaired renal function
When racemic citalopram is used in patients with renal failure (creatinine clearance 10-53 ml/min), a prolongation of T1/2 and a slight increase in AUC are observed. Plasma concentrations of metabolites have not been studied, but they may be increased.
Patients with low CYP2C19 isoenzyme activity
In individuals with weak CYP2C19 activity, the concentration of escitalopram is twice as high as in cases with high activity of this isoenzyme. No significant changes in the concentration of the drug were found in cases with weak activity of the CYP2D6 isoenzyme.
Special instructions
Special instructions
When using drugs belonging to the SSRI therapeutic group, including escitalopram, the following should be considered:
Use in children and adolescents under 18 years of age
Antidepressants should not be prescribed to children and adolescents under 18 years of age due to an increased risk of suicidal behavior (suicide attempts and suicidal thoughts), hostility (with a predominance of aggressive behavior, confrontational behavior and irritation). If a decision is made to initiate antidepressant therapy based on clinical assessment, the patient should be closely monitored. In addition, there is insufficient data on long-term safety in children and adolescents regarding growth, maturation, cognitive and behavioral development.
Paradoxical anxiety
Some patients with panic disorder may experience increased anxiety when starting antidepressant treatment. This paradoxical reaction usually disappears within the first two weeks of treatment. To reduce the likelihood of an anxiogenic effect, it is recommended to use low initial doses.
Convulsions
Escitalopram should be discontinued in the event of the primary development of convulsive seizures or in the event of an increase in their frequency (in patients with previously diagnosed epilepsy). SSRIs should not be used in patients with unstable epilepsy; Controlled seizures require careful monitoring.
Mania
Escitalopram should be used with caution in patients with a history of mania/hypomania. If a manic state develops, escitalopram should be discontinued.
Diabetes mellitus
In patients with diabetes mellitus, treatment with escitalopram may change blood glucose concentrations. Therefore, dose adjustments of insulin and/or oral hypoglycemic drugs may be required.
Suicide/suicidal ideation or clinical worsening
Depression is associated with an increased risk of suicidal ideation, self-harm, and suicide (suicidal events). This risk persists until significant remission occurs. Since improvement may not be observed during the first few weeks of therapy or even longer, patients should be closely monitored until their condition improves.
General clinical practice shows that in the early stages of recovery the risk of suicide may increase.
Other psychiatric conditions for which escitalopram is prescribed may also be associated with an increased risk of suicidal events and events. In addition, these conditions may be a comorbidity in relation to a depressive episode. When treating patients with other mental disorders, the same precautions should be taken as when treating patients with a depressive episode.
Patients with a history of suicidal behavior or patients with a significant level of suicidal thoughts before treatment are at greater risk for suicidal ideation or suicide attempts and should be closely monitored during treatment.
A meta-analysis of placebo-controlled clinical trials of antidepressants in adult patients with mental disorders found that there is an increased risk of suicidal behavior in patients under 25 years of age when taking antidepressants compared with placebo. Drug treatment of these patients, and in particular those at high risk for suicide, should be accompanied by careful monitoring, especially early in treatment and during dose changes.
Patients (and caregivers) should be warned to monitor for any signs of clinical worsening, suicidal behavior or ideation, or unusual changes in behavior, and to seek immediate medical advice if these symptoms occur.
Akathisia/psychomotor agitation
SSRI/SNRI use is associated with the development of akathisia, characterized by the development of a subjectively unpleasant or distressing need for constant movement, often combined with an inability to sit or stand quietly. This most often occurs during the first few weeks of treatment. In patients with such symptoms, increasing the dose may lead to worsening.
Hyponatremia
Hyponatremia, possibly associated with impaired antidiuretic hormone (ADH) secretion, occurs rarely with SSRIs and usually disappears when therapy is discontinued. Caution should be exercised when using escitalopram and other SSRIs in persons at risk of developing hyponatremia: the elderly, patients with cirrhosis of the liver, and those taking drugs that can cause hyponatremia.
Bleeding
Cases of skin hemorrhages (ecchymosis and purpura) have been reported when taking SSRIs. Escitalopram should be used with caution in patients taking oral anticoagulants and medications that affect blood clotting, as well as in patients with a tendency to bleed.
Electroconvulsive therapy
Because clinical experience with the concomitant use of SSRIs and electroconvulsive therapy (ECT) is limited, caution should be used when escitalopram and ECT are used concomitantly.
Serotonin syndrome
The simultaneous use of escitalopram and MAO A inhibitors is contraindicated due to the risk of developing serotonin syndrome.
Escitalopram should be used with caution concomitantly with drugs that have serotonergic effects, such as sumatriptan or other triptans, tramadol and tryptophan. Patients taking escitalopram and other SSRIs concomitantly with serotonergic drugs have rarely developed serotonin syndrome. Its development may be indicated by a combination of symptoms such as agitation, tremor, myoclonus and hyperthermia. If this occurs, concomitant treatment with SSRIs and serotonergic drugs should be discontinued immediately and symptomatic treatment initiated.
Withdrawal syndrome after cessation of therapy
When stopping treatment, withdrawal syndrome is common, especially if treatment is stopped abruptly. In clinical studies, adverse events at treatment discontinuation occurred in approximately 25% of patients receiving escitalopram and in 15% of patients receiving placebo.
The risk of withdrawal syndrome may depend on several factors, including the duration of therapy and the dose of the drug, as well as the rate of dose reduction. The most commonly reported reactions were dizziness, sensory disturbances (including paresthesia and electric shock), sleep disturbances (including insomnia and intense dreams), agitation or anxiety, nausea and/or vomiting, tremor, confusion, increased sweating, headache, diarrhea, palpitations, emotional instability, irritability and visual disturbances. These symptoms are usually mild to moderate, but may be severe in some patients. Symptoms usually occur within the first few days after stopping treatment, but such symptoms have been extremely rarely reported in patients who accidentally missed taking the drug.
As a rule, these symptoms resolve on their own, usually within 2 weeks, although in some patients they can be prolonged (2-3 months or more). Therefore, when stopping treatment, it is recommended to gradually reduce the dose over several weeks or months in accordance with the patient’s condition.
Coronary heart disease (CHD)
Due to limited experience with use in patients with coronary artery disease, caution is recommended when using the drug.
QT prolongation
Escitalopram has been found to cause a dose-dependent prolongation of the QT interval. Cases of QT prolongation and ventricular arrhythmias, including torsade de pointes (TdP), have been reported post-marketing, predominantly in female patients with hypokalemia or pre-existing QT prolongation, or other cardiac disease.
Caution is required when using the drug in patients with severe bradycardia or in patients with recent acute myocardial infarction or decompensated heart failure.
Electrolyte imbalances, such as hypokalemia and hypomagnesemia, increase the risk of developing malignant arrhythmias; these disturbances must be corrected before starting treatment with escitalopram.
In patients with chronic heart disease, an ECG should be performed before starting treatment.
If signs of cardiac arrhythmia occur during treatment with escitalopram, it is necessary to stop therapy and perform an ECG.
Angle-closure glaucoma
SSRIs, including escitalopram, may affect pupil size, leading to mydriasis. This pupil dilation effect has the potential to narrow the anterior chamber angle, leading to increased intraocular pressure and the development of angle-closure glaucoma, especially in patients with a predisposition to this disease. Therefore, in patients with angle-closure glaucoma or a history of glaucoma, caution should be exercised when using escitalopram.
Sexual dysfunction
SSRIs/SNRIs may cause symptoms of sexual dysfunction. There have been reports of long-term sexual dysfunction where symptoms continued despite discontinuation of SSRIs/SNRIs.
Alcohol
Escitalopram does not interact pharmacodynamically or pharmacokinetically with alcohol. However, as with other psychotropic drugs, the simultaneous use of escitalopram and alcohol is not recommended.
Impact on the ability to drive vehicles and machinery
During treatment with Escitalopram, patients are not recommended to drive a car or operate machinery. The patient should be informed of the potential danger of escitalopram’s effect on the ability to drive vehicles and operate machinery.
Active ingredient
Active ingredient
Escitalopram
Composition
Composition
active ingredient: escitalopram oxalate – 12.78 mg (in terms of escitalopram 10.00 mg);
excipients: microcrystalline cellulose – 96.02 mg, pregelatinized starch – 48.00 mg, colloidal silicon dioxide (aerosil) – 1.60 mg, magnesium stearate – 1.60 mg;
film coating: Opadry II white (31F28678) (lactose monohydrate – 2.30 mg, hypromellose – 1.80 mg, titanium dioxide – 1.66 mg, macrogol 3000 – 0.64 mg) – 6.40 mg.
Pregnancy
Pregnancy
Pregnancy
There are limited data on the use of escitalopram during pregnancy.
Animal studies of escitalopram have demonstrated reproductive toxicity.
Escitalopram should only be taken during pregnancy when absolutely necessary and after a careful benefit/risk assessment.
If escitalopram was continued during late pregnancy, especially in the third trimester, the newborn should be monitored. If escitalopram was continued until delivery or was stopped shortly before delivery, the newborn may develop withdrawal symptoms.
If the mother takes SSRIs/SNRIs (selective serotonin and norepinephrine reuptake inhibitors) in late pregnancy, the newborn may develop the following side effects: respiratory depression, cyanosis, apnea, convulsive disorders, temperature fluctuations, feeding difficulties, vomiting, hypoglycemia, hypertension, muscular hypotonia, hyperreflexia, tremor, increased neuro-reflex excitability, irritability, lethargic sleep, constant crying, drowsiness, poor sleep. These symptoms may occur due to the development of withdrawal syndrome or serotonergic effects. In most cases, complications occur within 24 hours of birth.
Evidence from epidemiological studies suggests that use of SSRIs during pregnancy, especially later in pregnancy, may increase the risk of developing persistent pulmonary hypertension of the newborn (PPHN). The observed risk was about 5 cases per 1000 pregnancies. In the general population, there are 1-2 cases of PPHN per 1000 pregnancies.
Breastfeeding period
Escitalopram is expected to be excreted in breast milk, therefore breastfeeding is contraindicated during treatment with escitalopram. If it is necessary to use escitalopram, breastfeeding should be discontinued.
Fertility
Evidence from animal studies has shown that some SSRIs may affect sperm quality. There are no animal studies on this aspect for escitalopram. Reports of the use of some SSRIs in humans have shown that the effects of these drugs on sperm quality are reversible. To date, no effect of escitalopram on human fertility has been observed.
Contraindications
Contraindications
Hypersensitivity to escitalopram or to any of the excipients included in this drug.
Simultaneous use of non-selective irreversible monoamine oxidase inhibitors (MAO), simultaneous use of reversible MAO A inhibitors (moclobemide), reversible non-selective MAO inhibitors (linezolid).
History of QT prolongation, including congenital long QT syndrome.
Concomitant use of drugs that prolong the QT interval (for example, class IA and III antiarrhythmic drugs, tricyclic antidepressants, macrolides).
Concomitant use of pimozide.
Children and adolescents under 18 years of age (the effectiveness and safety of use have not been studied).
Pregnancy, breastfeeding period.
Lactose intolerance, lactase deficiency, glucose-galactose malabsorption.
WITH CAUTION
Severe renal failure (creatinine clearance less than 30 ml/min), manic disorders (including history), pharmacologically uncontrolled epilepsy, severe suicidal behavior, coronary heart disease, diabetes mellitus, electroconvulsive therapy; old age (over 65 years), cirrhosis of the liver, tendency to bleeding; simultaneous use with drugs that reduce the threshold of convulsive readiness, tryptophan, drugs containing St. John’s wort, lithium; with drugs that cause hyponatremia, oral anticoagulants and other drugs that affect blood clotting; with drugs metabolized with the participation of the CYP2C19 isoenzyme, ethanol, simultaneous use with an MAO B inhibitor (selegiline), serotonergic drugs.
Side Effects
Side Effects
Adverse reactions associated with the use of escitalopram are observed during the first one to two weeks of treatment and usually significantly subside as therapy continues and the patient’s condition improves.
Frequency of undesirable side reactions (according to WHO classification): very often – ≥ 10%; often – ≥ 1%, but < 10%; uncommon – ≥ 0.1%, but < 1%; rarely - ≥ 0.01%, but < 0.1%; very rare - <0.01%, unknown - currently there are no data on the prevalence of adverse reactions.
The following adverse reactions may occur:
Blood and lymphatic system disorders
Frequency unknown: thrombocytopenia.
Immune system disorders
Rarely: anaphylactic reactions.
Endocrine system disorders
Not known: insufficient secretion of antidiuretic hormone (ADH).
Metabolic and nutritional disorders
Often: decreased appetite, increased appetite, weight gain;
Uncommon: weight loss;
Frequency unknown: hyponatremia, anorexia1.
Mental disorders
Common: anxiety, restlessness, unusual dreams, decreased libido,
anorgasmia (in women);
Uncommon: bruxism, agitation, nervousness, panic attacks, confusion;
Rarely: aggression, depersonalization, hallucinations;
Frequency unknown: mania, suicidal ideation, suicidal behavior2.
Nervous system disorders
Very common: headache;
Common: insomnia, drowsiness, dizziness, paresthesia, tremor;
Uncommon: taste disturbances, sleep disturbances, syncope (fainting);
Rarely: serotonin syndrome;
Frequency unknown: dyskinesia, movement disorders, seizure disorders, psychomotor agitation/akathisia1.
Visual disorders
Uncommon: mydriasis (pupil dilation), visual impairment.
Hearing and labyrinth disorders
Uncommon: tinnitus (tinnitus).
Heart disorders
Uncommon: tachycardia;
Rarely: bradycardia;
Frequency unknown: prolongation of the QT interval on the electrocardiogram, ventricular arrhythmia, including torsade de pointes (TdP).
Vascular disorders
Frequency unknown: orthostatic hypotension.
Respiratory, thoracic and mediastinal disorders
Common: sinusitis, yawning;
Uncommon: nosebleeds.
Gastrointestinal disorders
Very common: nausea;
Common: diarrhea, constipation, vomiting, dry mouth;
Uncommon: gastrointestinal bleeding (including rectal bleeding).
Disorders of the liver and biliary tract
Frequency unknown: hepatitis, liver function abnormalities.
Skin and subcutaneous tissue disorders
Common: increased sweating;
Uncommon: urticaria, alopecia, rash, itching;
Frequency unknown: ecchymosis, angioedema.
Musculoskeletal and connective tissue disorders
Common: arthralgia, myalgia.
Renal and urinary tract disorders
Frequency unknown: urinary retention.
Disorders of the genital organs and breast
Common: impotence, ejaculation disorders;
Uncommon: metrorrhagia (uterine bleeding), menorrhagia;
Frequency unknown: galactorrhea, priapism.
General and administration site disorders
Often: weakness, hyperthermia;
Uncommon: swelling.
1Adverse events recorded with the use of drugs of the SSRI class.
2Cases of suicidal thoughts and behavior have been reported while taking escitalopram and immediately after discontinuation of therapy.
During the post-marketing period, cases of QT prolongation and ventricular arrhythmias, including torsade de pointes (TdP), have been reported, predominantly in female patients with hypokalemia or pre-existing QT prolongation or other cardiovascular disease. In double-blind, placebo-controlled ECG studies in healthy volunteers, the change from baseline QTc (correction using the Fridericia formula) was 4.3 msec at a dose of 10 mg/day. and 10.7 msec – at 30 mg/day.
Class effect
In epidemiological studies involving patients 50 years of age or older, an increased risk of bone fractures has been reported in patients receiving SSRIs and tricyclic antidepressants. The mechanism leading to this risk is unknown.
Withdrawal symptoms after finishing treatment
Stopping SSRIs/SNRIs (selective norepinephrine and serotonin reuptake inhibitors) (especially abruptly) usually results in withdrawal symptoms. The most commonly observed symptoms are dizziness, sensory disturbances (including paresthesia and electric current sensations), sleep disturbances (including insomnia and vivid dreams), agitation or anxiety, nausea and/or vomiting, tremors, confusion, increased sweating, headache, diarrhea, rapid heartbeat, emotional instability, irritability and visual disturbances. As a rule, these phenomena are mild or moderate in severity and resolve on their own, but in some patients they can become severe and last longer. It is recommended to gradually discontinue the drug by reducing its dose.
Interaction
Interaction
Pharmacodynamic interactions:
Concomitant use is contraindicated:
With irreversible non-selective MAO inhibitors
Serious adverse reactions have been reported with concomitant use of SSRIs and irreversible non-selective MAO inhibitors, as well as when starting MAO inhibitors in patients who have recently stopped SSRI therapy and started therapy with such MAO inhibitors. In some cases, patients developed serotonin syndrome.
The use of escitalopram simultaneously with non-selective irreversible MAO inhibitors is contraindicated.
Escitalopram can be prescribed 14 days after stopping treatment with irreversible non-selective MAO inhibitors. At least 7 days must pass after stopping escitalopram before treatment with irreversible non-selective MAO inhibitors can be prescribed.
With reversible selective MAO type A inhibitors (moclobemide)
Due to the risk of developing serotonin syndrome, the combined use of escitalopram with reversible selective MAO inhibitors, such as moclobemide, is contraindicated. If there is a justified need for the use of such a combination, treatment should begin with the minimum recommended dose under enhanced clinical supervision.
Escitalopram can be started at least one day after discontinuation of the reversible MAO A inhibitor moclobemide.
With reversible non-selective MAO inhibitors (linezolid)
The antibiotic linezolid is a reversible, non-selective MAO inhibitor and should not be used in patients receiving escitalopram therapy. If there is a justified need for the use of such a combination, treatment should begin with minimal doses under close clinical supervision.
With irreversible selective MAO type B inhibitors (selegiline)
Caution is required in the case of concomitant use of escitalopram and the irreversible selective MAO type B inhibitor selegiline due to the risk of developing serotonin syndrome. Selegiline in doses up to 10 mg per day has been used successfully with racemic citalopram.
With drugs that prolong the QT interval
Pharmacokinetic and pharmacodynamic studies of the use of escitalonram in combination with other drugs that prolong the QT interval have not been conducted. An additive effect of escitalopram and these drugs cannot be excluded. Therefore, the simultaneous use of escitalopram and drugs that prolong the QT interval, such as antiarrhythmics (procainamide, amiodarone, etc.), antipsychotics/neuroleptics (for example, pimozide, phenothiazine derivatives (chlorpromazine, trifluoperazine, thioridazine, etc.), butyrophenone derivatives (haloperidol, droperidol and others) is contraindicated. etc.), tricyclic and tetracyclic antidepressants (amitriptyline, imipramine, maprotiline, etc.), SSRIs and similar antidepressants (for example, fluoxetine, venlafaxine, etc.), antimicrobial drugs (macrolide antibiotics and their analogues, for example, erythromycin, clarithromycin; quinolone and fluoroquinolone derivatives: sparfloxacin, moxifloxacin; pentamidine), azole antifungals (ketoconazole, fluconazole), domperidone, ondansetron, drugs for the treatment of malaria, especially halofantrine, some antihistamines (astemizole, mizolastine), since escitalopram in doses exceeding 20 mg per day can cause abnormal changes in the electrical activity of the heart (prolongation). QT interval on the ECG) and lead to heart rhythm disturbances (incl. development of arrhythmias of the “pirouette” type), which can be fatal.
Concomitant use of Escitalopram should be done with caution when used:
Medicines that lower the seizure threshold
Escitalopram may lower the seizure threshold. Caution is required when taking other drugs that lower the seizure threshold (tricyclic antidepressants, SSRIs, antipsychotics – phenothiazine derivatives, thioxanthene and butyrophenone; mefloquine and tramadol, bupropion).
Serotonergic drugs
It is advisable not to combine Escitalopram-ALSI with serotonergic drugs such as sumatriptan or other triptans, as well as tramadol, as this may lead to the development of serotonin syndrome.
Lithium, tryptophan
When used simultaneously with tryptophan or with lithium preparations, cases of increased effect of escitalopram have been reported.
Therefore, caution should be exercised when prescribing escitalopram and these drugs simultaneously.
St. John’s wort
The simultaneous use of escitalopram and drugs containing St. John’s wort (Hypericum perforatum) may lead to increased side effects.
Anticoagulants and agents affecting blood clotting
With simultaneous use of escitalopram with indirect anticoagulants and other drugs that affect blood coagulation (for example, atypical antipsychotics and phenothiazine derivatives, most tricyclic antidepressants, acetylsalicylic acid and non-steroidal anti-inflammatory drugs, ticlopidine and dipyridamole), a blood clotting disorder may occur. In such cases, regular monitoring of blood clotting is necessary when starting or ending therapy with escitalopram.
There was no interaction between escitalopram and alcohol. However, as with other antidepressants, you should avoid drinking alcohol during the entire period of treatment with the drug.
Concomitant use with non-steroidal anti-inflammatory drugs may lead to an increase in the number of bleedings.
Drugs that cause hypokalemia/hypomagnesemia
Caution is required when simultaneous use of drugs that cause the development of hypokalemia/hypomagnesemia, since these conditions increase the risk of developing malignant arrhythmias.
Pharmacokinetic interactions:
Effect of other drugs on the pharmacokinetics of escitalopram
Escitalopram is metabolized mainly by the enzyme CYP2C19. CYP3A4 and CYP2D6 may also be involved in metabolism, although to a lesser extent. Metabolism of the main metabolite, S-DCT (demethylated escitalopram), is partially catalyzed by CYP2D6.
Co-administration of escitalopram and omeprazole 30 mg once daily (CYP2C19 inhibitor) resulted in a moderate (approximately 50%) increase in escitalopram plasma concentrations.
Co-administration of escitalopram and cimetidine 400 mg twice daily (a general, moderately potent enzyme inhibitor) resulted in a moderate (approximately 70%) increase in escitalopram plasma concentrations. Escitalopram should be combined with cimetidine with caution. Dose adjustment may be required.
Therefore, the drug should be combined with caution with CYP2C19 inhibitors (such as omeprazole, esomeprazole, fluvoxamine, lansoprazole, ticlopidine) or cimetidine. When taking escitalopram and the above drugs simultaneously, a dose reduction of escitalopram may be necessary based on clinical assessment.
Effect of escitalopram on the pharmacokinetics of other drugs
Escitalopram is an inhibitor of the CYP2D6 enzyme. Caution should be exercised when coadministering escitalopram with drugs with a narrow therapeutic index that are primarily metabolized by this enzyme, such as flecainide, propafenone, and metoprolol (for use in heart failure), or certain drugs that act on the central nervous system that are primarily metabolized by CYP2D6, such as antidepressants such as desipramine, clomipramine, and nortriptyline. antipsychotics such as risperidone, thioridazine and haloperidol. In these cases, dose adjustment may be required.
Concomitant use of the drug with desipramine or metoprolol led to a twofold increase in the concentration of these CYP2D6 substrates in the blood plasma.
In vitro studies have shown that escitalopram may also be a weak inhibitor of CYP2C19. It is recommended to use the drug with caution simultaneously with drugs metabolized by CYP2C19.
Overdose
Overdose
Data on overdose with escitalopram are limited, and many such cases have involved overdose with other drugs. In most cases, symptoms of overdose do not appear or are mild. Cases of overdose of escitalopram (without taking other drugs) with a fatal outcome are rare, in most cases there is also an overdose of other drugs. When taking escitalopram in the dose range from 400 mg to 800 mg in monotherapy, no clinically significant symptoms of overdose occurred.
Symptoms
In case of an overdose of escitalopram, symptoms mainly occur from the central nervous system (from dizziness, tremor and agitation to rare cases of serotonin syndrome, convulsive disorders and coma), from the gastrointestinal tract (nausea/vomiting), from the cardiovascular system (hypotension, tachycardia, prolongation of the QT interval and arrhythmia) and electrolyte imbalance (hypokalemia, hyponatremia).
Treatment
There is no specific antidote. Normal airway patency, oxygenation and ventilation of the lungs should be ensured. Gastric lavage should be performed and activated charcoal should be prescribed. Gastric lavage should be performed as soon as possible after taking the drug. It is recommended to monitor the performance of the heart and other vital organs and provide symptomatic and supportive therapy.
Storage conditions
Storage conditions
At a temperature not exceeding 25ºС in original packaging.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after the expiration date stated on the package.
Manufacturer
Manufacturer
ALSI Pharma, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date stated on the package. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25ºC in the original package. Keep out of reach of children. |
| Manufacturer | ALSI Pharma, Russia |
| Medication form | pills |
| Brand | ALSI Pharma |
Other forms…
Related products
Buy Excitalopram-ALSI, 10 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.