No products in the cart.
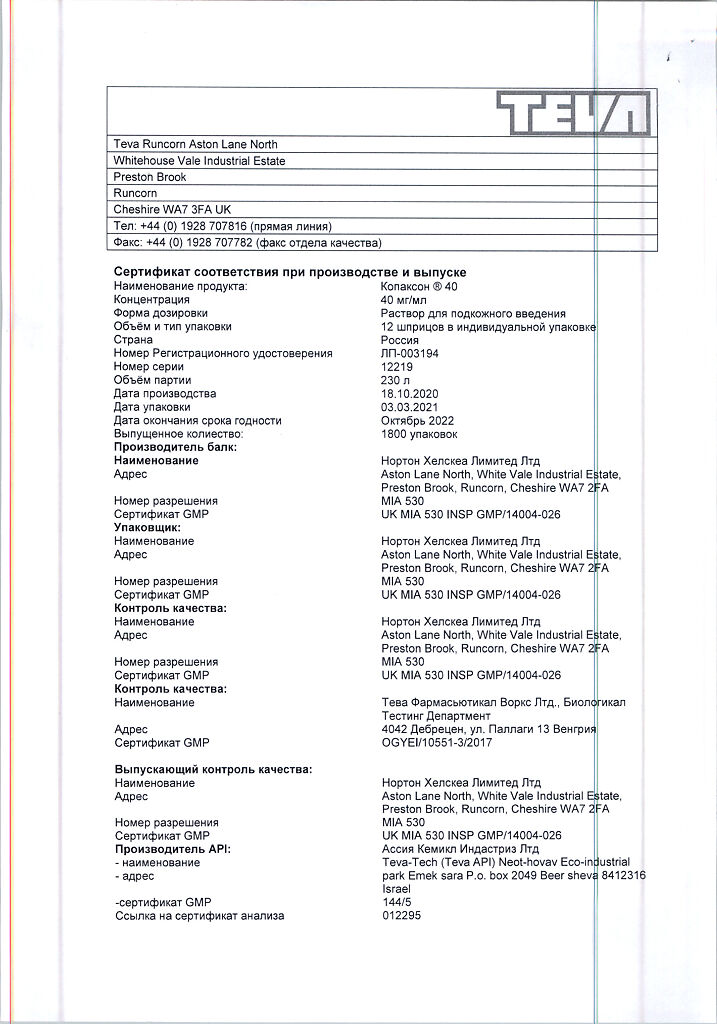
Copaxone 40,40 mg/ml 1 ml syringes 12 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Recurrent-remitting multiple sclerosis.
Indications
Indications
Relapsing-remitting multiple sclerosis.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group:
Special instructions
Special instructions
Initiation of treatment with Copaxone 40 should be carried out under the supervision of a neurologist and a physician with experience in the treatment of multiple sclerosis. The drug is not indicated for the treatment of primary or secondary progressive multiple sclerosis.
Patients should be informed about the possibility of adverse reactions, including those occurring immediately after injection of Copaxone 40. Most of these symptoms are short-lived and resolve spontaneously without consequences.
If serious adverse reactions develop, you should immediately stop therapy and consult your doctor or call an ambulance. The decision to use symptomatic therapy is made by the doctor.
There is no evidence that certain groups of patients are at greater risk of such reactions. However, patients with cardiovascular diseases should be under medical supervision throughout the entire treatment period.
Several cases of seizures and/or anaphylactoid or allergic reactions have been identified. Serious hypersensitivity reactions (bronchospasm, anaphylactic reaction or urticaria) may also rarely occur.
In case of severe reactions, appropriate treatment should be prescribed and the drug should be discontinued.
Antibodies to glatiramer acetate were detected in the patients’ blood serum. After a course of treatment with an average duration of 3-4 months, their maximum concentration was recorded, which subsequently decreased and stabilized at a level slightly above the baseline.
There is no evidence that antibodies to glatiramer acetate have a neutralizing effect or affect the clinical effectiveness of the drug.
Renal function should be monitored in patients with renal failure, although there is no convincing evidence that immune complex deposition affects glomerular filtration.
If the patient does not have the opportunity to store syringes with Copaxone 40 in the refrigerator, then storage at a temperature of 15-25 ° C is allowed, but not more than one month.
If the syringes with the drug have not been used within a month, and the blister packaging has not been opened, then these syringes should continue to be stored in the refrigerator (2-8 °C).
Impact on the ability to drive vehicles. Wed and fur.:
No studies have been conducted to study the effect on the ability to drive vehicles and machinery.
Active ingredient
Active ingredient
Glatiramer acetate
Composition
Composition
1 ml of solution contains:
active ingredient:
glatiramer acetate 40.0 mg;
excipients:
mannitol 40.0 mg,
water for injections up to 1 ml.
Pregnancy
Pregnancy
There is no data on the use of Copaxone 40 during pregnancy. the possible risk of use during pregnancy has not been established.
Animal studies are insufficient to establish the effect of the drug on pregnancy, embryo/fetal development, childbirth and postnatal development. Copaxone 40 is contraindicated during pregnancy. During treatment it is necessary to use reliable methods of contraception.
It is not known whether glatiramer acetate is excreted in breast milk, therefore, if it is necessary to use Copaxone 40 during lactation, the expected benefit of therapy for the mother and the potential risk for the child should be assessed.
Contraindications
Contraindications
Hypersensitivity to glatiramer acetate or mannitol;
children under 18 years of age (efficacy and safety have not been studied):
pregnancy.
With caution:
Predisposition to the development of allergic reactions, cardiovascular diseases, impaired renal function.
Side Effects
Side Effects
Most of the data on the safety of the drug Copaxone 40 have been accumulated based on the use of the drug Copaxone-Teva 20 mg/ml in the form of daily injections.
This section presents data accumulated during the conduct of 4 placebo-controlled clinical studies on the use of the drug Copaxone-Teva in the form of subcutaneous injections at a dose of 20 mg/ml 1 time per day and 1 placebo-controlled study on the use of the drug Copaxone 40 in the form of subcutaneous injections at a dose of 40 mg/ml 3 times a week.
Copaxone-Teva 20 mg/ml (used daily)
The most common reactions observed during clinical trials of Copaxone-Teva were reactions at the injection site.
Placebo-controlled studies have shown that the proportion of patients reporting these adverse events at least once was 70% for Copaxone-Teva and 37% for placebo. Redness was most often observed. pain. Induration, itching, swelling, inflammation and hypersensitivity.
A reaction associated with at least one or more symptoms (vasodilation, chest pain, shortness of breath, rapid heart rate or tachycardia) that occurs within a few minutes after injection is called an immediate post-injection reaction.
At least one symptom of this reaction occurred at least once in 31% of patients receiving Copaxone-Teva, compared with 13% of patients receiving placebo.
All the adverse reactions most often observed in Nazis receiving Copaxone-Teva compared to the placebo group are presented below.
These data were obtained from four registrational, double-blind, placebo-controlled studies involving 512 patients treated with Copax-Teva daily and 509 patients treated with placebo for 36 months.
The three studies included 269 patients diagnosed with relapsing-remitting multiple sclerosis who received Copaxone-Teva daily for 35 months and 271 patients in the placebo group.
The fourth study included 243 patients (Copaxone-Teva group) with the first clinical diagnosis of the disease who were found to be at high risk of developing clinically confirmed multiple sclerosis and 238 patients receiving placebo. The duration of the study was 36 months.
The incidence of adverse reactions is classified as follows: very often (≥1/10); common (≥1/100, but <1/10): uncommon (≥1/1000, but <1/100): rare (≥1/10000, but <1/11000).
Infections and infestations: very often – infections, influenza; often – bronchitis, gastroenteritis, otitis media, Herpes simplex, rhinitis, periodontal abscess, vaginal candidiasis*; uncommon – abscess, inflammation of subcutaneous fat, furunculosis, pyelonephritis, Herpes zoster.
Neoplasms, including polyps and cysts: often – benign skin neoplasms, neoplasms: infrequently – skin cancer.
From the hematopoietic and lymphatic systems: often – lymphadenopathy*; uncommon – leukocytosis, leukopenia, splenomegaly, thrombocytopenia, changes in lymphocyte morphology.
From the immune system: often – hypersensitivity reactions.
From the endocrine system: infrequently – goiter, hyperthyroidism.
Metabolism and nutrition: often – anorexia, weight gain*; uncommon – alcohol intolerance, gout, hyperlipidemia, hypernatremia, decreased serum ferritin concentration.
Mental disorders: very often – anxiety*, depression; often – nervousness; uncommon – unusual dreams, psychosis, euphoria, hallucinations, aggressiveness, mania, personality disorders, suicide attempts.
From the nervous system: very often – headache; often – taste perversion, muscle hypertonicity, migraine, speech impairment, fainting, tremor*; uncommon – carpal tunnel syndrome, cognitive disorders, seizures, dysgraphia, dyslexia, dystonia, motor dysfunction, myoclonus, neuritis, neuromuscular blockade, nystagmus, paralysis, peroneal nerve palsy, stupor, visual field defect.
From the organs of vision: often – diplopia, visual impairment*; uncommon – cataract, corneal damage, dry sclera and cornea, hemorrhage in the eye, eyelid ptosis, mydriasis, optic nerve atrophy.
On the part of the organs of hearing and balance: often – hearing impairment.
From the cardiovascular system: very often – vasodilation*; often – palpitations*, tachycardia*; infrequently – extrasystole, sinus bradycardia, paroxysmal tachycardia, varicose veins.
From the respiratory system: very often – shortness of breath*; often – cough, seasonal rhinitis; uncommon – apnea, feeling of suffocation, nosebleeds, hyperventilation, laryngospasm, pulmonary disorders.
From the gastrointestinal tract: very often – nausea*; often – anorectal disorders, constipation, caries, dyspepsia, dysphagia, fecal incontinence, vomiting*; uncommon – colitis, enterocolitis, colon polyposis, belching, peptic ulcer of the esophagus, periodontitis, rectal bleeding, enlarged salivary glands.
From the liver and biliary tract: often – deviation of liver tests; infrequently – cholelithiasis, hepatomegaly.
From the skin and subcutaneous fat: very often – skin rash*; often – ecchymosis, hyperhidrosis, itching, skin diseases*, urticaria; uncommon – angioedema, contact dermatitis, erythema nodosum, skin nodules.
From the musculoskeletal system and connective tissue: very often – arthralgia, back pain*; often – neck pain; uncommon – arthritis, bursitis, flank pain, muscle atrophy, osteoarthritis.
From the kidneys and urinary system: often – imperative urges, pollakiuria. urinary retention; infrequently – hematuria, nephrolithiasis. diseases of the urinary tract, deviations from laboratory norms of urine analysis.
Pregnancy, postpartum and perinatal conditions: uncommon – spontaneous abortion.
From the genital organs and mammary gland: infrequently – engorgement of the mammary glands, erectile dysfunction, pelvic organ prolapse, priapism, prostate diseases, deviation of laboratory parameters in smears from the cervical canal, dysfunction of the testicles, vaginal bleeding, vulvovaginal disorders.
Other: very often – asthenia, chest pain*, reactions at the injection site* and
**, pain*; often – chills*, facial swelling*, atrophy at the injection site***, local reactions*, peripheral edema, edema, fever; uncommon – hypothermia, immediate post-injection reaction, inflammation, cyst, hangover syndrome, diseases of the mucous membranes, post-vaccinal syndrome, necrosis at the injection site.
* The likelihood of such cases occurring in patients taking Copaxone-Teva is more than 2% (>2/100) compared to the placebo group. An adverse reaction without the “*” sign indicates a difference less than or equal to 2%.
** “Injection site reactions” (various types) includes any adverse events occurring at the injection site, with the exception of atrophy and necrosis, which are listed separately.
***Refers to localized lipoatrophy at the injection site.
In the fourth clinical trial noted above, a placebo-controlled phase was followed by an open-label study phase that lasted 5 years. During this study, no changes were detected in the previously established safety profile of Copaxone-Teva.
In patients with multiple sclerosis who received Copaxone-Teva during uncontrolled clinical trials, as well as during post-marketing use, rare (≥1/10,000, but <1/1000) cases of anaphylactoid reactions were reported.
Copaxone 40 at a dosage of 40 mg/ml (used three times a week)
The 12-month, double-blind, placebo-controlled study assessed the safety of Copaxone 40 in 943 patients diagnosed with relapsing-remitting multiple sclerosis compared with a placebo group of 461 patients.
In general, in patients who took Copaxone 40 three times a week, adverse reactions at the injection site coincided with the rate that were noted with daily administration of Copaxone-Teva 20 mg/ml.
In particular, injection site reactions (ISRs) and immediate post-injection reactions (IPRs) were observed less frequently with Copaxone 40 administered three times a week than with daily injections of Copaxone-Teva (35.5% compared with 70% for IPR and 7.8% compared with 31% for NPIR, respectively).
RMI was observed in 36% of patients treated with Copaxone 40 compared with 5% of patients treated with placebo. 8% of patients receiving Copaxone 40 compared with 2% of patients receiving placebo experienced ADRs.
Several specific adverse reactions were noted:
in patients with multiple sclerosis receiving Copaxone-Teva 20 mg/ml pr], uncontrolled clinical studies, as well as post-marketing experience, an anaphylactic reaction was observed in rare cases (≥1/10,000, but <1/1000). In patients taking the drug Copaxone 40. Such cases were 0.3% (uncommon: ≥1/1000, but <1/100);
Not a single case of necrosis at the injection site was identified:
in 2.1% of patients receiving Copaxone 40 (common: ≥1/100, but <1/10). cases of redness of the skin and pain in the extremities were observed, which were not detected in the case of using the drug Copaxone-Teva 20 mg/ml:
in one patient (0.1%). receiving Copaxone 40 (uncommon: ≥1/1000, but <1/100). Drug-induced liver damage and toxic hepatitis were observed, which were also rare in patients with multiple sclerosis taking Copaxone-Teva 20 mg/ml during post-marketing surveillance.
Interaction
Interaction
The interaction between Copaxone 40 and other drugs has not been separately evaluated. There is no evidence of interaction with interferon beta.
An increase in cases of reactions at the injection site was detected with simultaneous administration of the drug Copaxone 40 with glucocorticosteroids.
An in vitro study suggested that glatiramer acetate is highly bound to plasma proteins and is not displaced from plasma protein binding on its own by phenytoin or carbamazepine.
Overdose
Overdose
Several reports of overdose (up to 300 mg of glatiramer acetate) have been received. No adverse reactions other than those listed in the Side Effects section were observed.
In case of overdose, careful observation, symptomatic and supportive treatment are indicated.
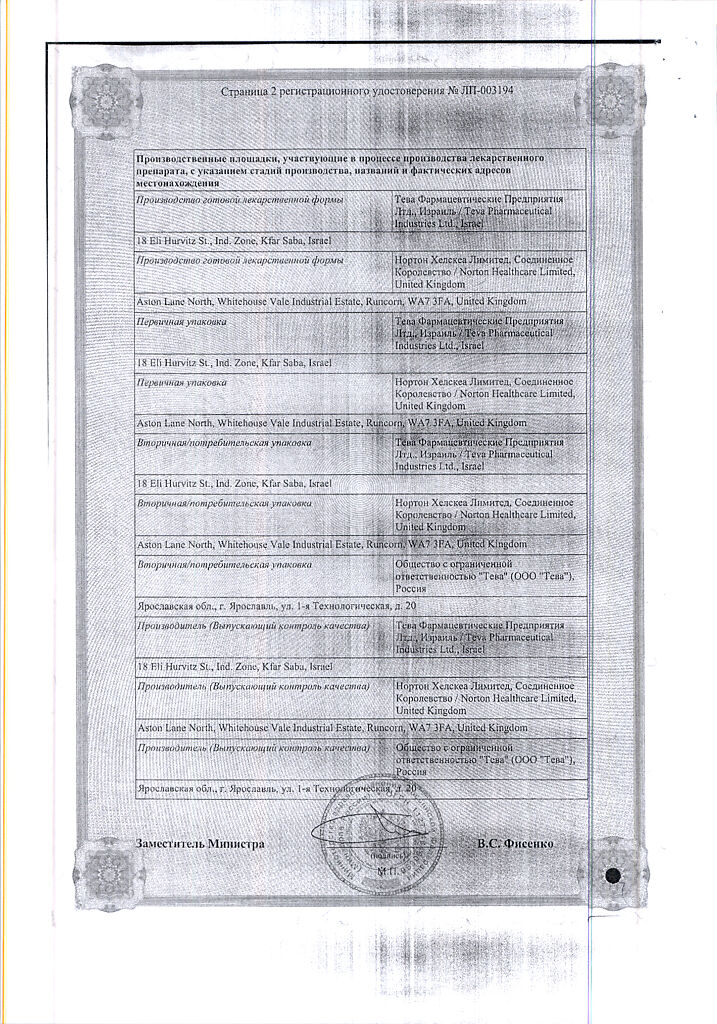
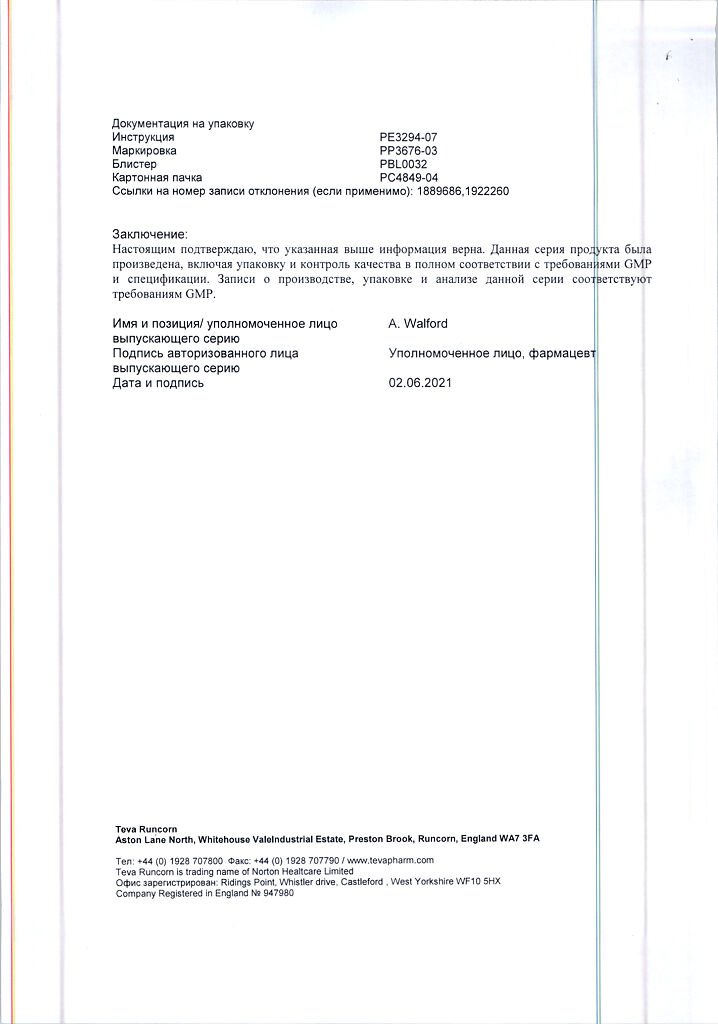
Manufacturer
Manufacturer
Teva Pharmaceutical Enterprises Ltd., Israel
Additional information
| Manufacturer | Teva Pharmaceutical Enterprises Ltd, Israel |
|---|---|
| Medication form | solution |
| Brand | Teva Pharmaceutical Enterprises Ltd |
Related products
Buy Copaxone 40,40 mg/ml 1 ml syringes 12 pcs with delivery to USA, UK, Europe and over 120 other countries.