No products in the cart.
Brufen SR, 800 mg 14 pcs
€6.22 €5.53
Description Non-steroidal anti-inflammatory drug (NSAID) Pharmacodynamics:
ATX: M.01.A.E.01 Ibuprofen
Ibuprofen is a propionic acid derivative, a nonsteroidal anti-inflammatory drug (NSAID) that has analgesic, anti-inflammatory and antipyretic effects. The therapeutic effect of the drug is due to inhibition of cyclooxygenase enzyme, which leads to a significant decrease in the synthesis of prostaglandins. These properties provide elimination of symptoms of inflammation, pain and fever.
Experimental data show that concomitant use of ibuprofen may inhibit the effect of low doses of acetylsalicylic acid on platelet aggregation. In a single study, a single dose of ibuprofen 400 mg for 8 hours before or within 30 minutes of immediate-release acetylsalicylic acid (81 mg) was observed to reduce the effect of acetylsalicylic acid on thromboxane formation or platelet aggregation.
Because of the limitations of these data and the imprecision in extrapolating ex vivo data to the clinical situation, however, reliable conclusions regarding the continued use of ibuprofen cannot be drawn. The development of clinically significant effects is considered unlikely with episodic use of ibuprofen.
Pharmacokinetics:
Ibuprofen is a racemic mixture of [+]S- and [-]R-enantiomers. Studies have shown that food intake has no significant effect on overall bioavailability.
Absorption
Ibuprofen is rapidly absorbed in the gastrointestinal tract, bioavailability is 80 – 90%, time to maximum concentration (TSmax) in plasma when using the drug form of immediate release – 1-2 hours. Prolonged dosage form of ibuprofen 800 mg tablets provides a gradual release of the active substance, with a slower release rate compared to the dosage form of immediate release and a decrease in the value of maximum concentration (Cmax) in blood plasma, which is reached approximately 3 hours after the use of ibuprofen. As a result of the prolonged absorption phase, plasma concentrations of ibuprofen are maintained longer in the systemic bloodstream.
Thus, ibuprofen 800 mg tablets with prolonged action only once a day. A comparison of the pharmacokinetic profile of two 800 mg sustained-release ibuprofen tablets and 400 mg immediate-release ibuprofen tablets taken four times daily showed that the sustained-release dosage form provided a reduced range of differences between Cmax and threshold concentrations of immediate-release tablets and maintained higher mean plasma concentrations after 5, 10, 15 and 24 hours. The area under the curve “concentration – time” (AUC) was similar for immediate release tablets and prolonged release tablets.
Distribution
Ibuprofen is intensively bound to blood plasma proteins (99%). The volume of distribution (Vd) of ibuprofen is small and is approximately 0.12 – 0.2 L/kg in adults.
Metabolism
Ibuprofen is rapidly metabolized in the liver with the participation of cytochrome P450 isoenzymes, primarily CYP2C9, to form two major inactive metabolites – 2-hydroxyibuprofen and 3-carboxyibuprofen. When ibuprofen is administered orally, slightly less than 90% of the ingested dose of ibuprofen may be detected in the urine as oxidative metabolites and their glucuron conjugates. A small amount of ibuprofen is excreted unchanged in the urine.
Excretion
Excretion of ibuprofen through the kidneys is fast and complete. The elimination half-life (T1/2) of immediately-released forms is about two hours. Ibuprofen is almost completely eliminated from the body 24 hours after the last dose.
Special patient groups
Patients of the elderly
In elderly patients in the absence of renal failure only small, clinically insignificant differences in the pharmacokinetic profile and urinary excretion compared to younger patients are observed. Renal failure
In patients with moderate renal failure, elevated plasma (S)-ibuprofen levels, elevated AUC (S)-ibuprofen values and elevated enantiomeric AUC (S/R) ratio values were observed compared to healthy control patients. In patients with end-stage renal failure who were on dialysis, the mean free fraction of ibuprofen was about 3% compared to 1% in healthy volunteers. Serious renal dysfunction can lead to accumulation of ibuprofen metabolites. The significance of this effect is unknown. Metabolites may be excreted by hemodialysis.
Liver failure
The presence of alcoholic liver disease in mild to moderate liver failure had no significant effect on pharmacokinetic parameters.
Patients with cirrhosis and moderate liver failure (6-10 Child-Pugh scores) treated with racemic ibuprofen showed a 2-fold increase in T1/2, on average, and the enantiomeric AUC (S/R) value was significantly lower compared to healthy control group patients, indicating impaired metabolic transformation of (R)-ibuprofen to the active (S)-enantiomer.
Indications
Indications
Inflammatory and degenerative diseases: rheumatoid arthritis, including juvenile rheumatoid arthritis or Still’s syndrome, osteoarthritis, articular syndrome with exacerbation of gout, psoriatic arthritis, ankylosing spondylitis, spondylosis.
Diseases of periarticular tissues, including rheumatic ones: glenohumeral periarthritis (capsulitis), bursitis, tendinitis, tenosynovitis, tendovaginitis, lower back pain, sciatica.
Damage to soft tissues: traumatic inflammation of soft tissues and the musculoskeletal system, dislocations and sprains, hematomas.
Relief of mild or moderate pain syndrome with: headache, toothache, primary dysmenorrhea, postoperative pain, migraine, panniculitis, neuralgia, myalgia.
Inflammatory processes in the pelvis: adnexitis, algodismenorrhea.
Pharmacological effect
Pharmacological effect
Non-steroidal anti-inflammatory drug (NSAID)
ATC: M.01.A.E.01 Ibuprofen
Pharmacodynamics:
Ibuprofen is a derivative of propionic acid, a non-steroidal anti-inflammatory drug (NSAID), which has analgesic, anti-inflammatory and antipyretic effects. The therapeutic effect of the drug is due to inhibition of the enzyme cyclooxygenase, which leads to a significant decrease in the synthesis of prostaglandins. These properties provide relief from symptoms of inflammation, pain and fever.
Experimental data indicate that concomitant use of ibuprofen may inhibit the effect of low doses of acetylsalicylic acid on platelet aggregation. In a single study, a decrease in the effect of acetylsalicylic acid on thromboxane formation or platelet aggregation was observed when a single dose of ibuprofen 400 mg was administered within 8 hours before or within 30 minutes after immediate-release acetylsalicylic acid (81 mg).
However, due to the limitations of these data and the uncertainty in extrapolating ex vivo data to the clinical situation, reliable conclusions regarding chronic ibuprofen use cannot be drawn. The development of clinically significant effects is considered unlikely with occasional use of ibuprofen.
Pharmacokinetics:
Ibuprofen is a racemic mixture of [+]S- and [-]R-enantiomers. Studies have shown that food intake has no significant effect on overall bioavailability.
Suction
Ibuprofen is rapidly absorbed in the gastrointestinal tract, bioavailability is 80 – 90%, the time to reach the maximum concentration (TCmax) in the blood plasma when using the immediate release dosage form is 1-2 hours. The extended dosage form of ibuprofen tablets 800 mg provides gradual release of the active substance, with a slower release rate compared to immediate release dosage forms and a decrease in the maximum concentration (Cmax) in blood plasma, which is achieved approximately 3 hours after ibuprofen administration. As a result of the prolonged absorption phase in the systemic circulation, plasma concentrations of ibuprofen are maintained longer.
Thus, it is enough to take ibuprofen 800 mg extended-release tablets only once a day. Comparison of the pharmacokinetic profile of two extended-release ibuprofen tablets at a dose of 800 mg and ibuprofen immediate-release tablets at a dose of 400 mg taken four times daily showed that the extended-release dosage form provided a reduction in the range of differences between Cmax and threshold concentrations of the immediate-release tablets and maintained higher mean plasma concentrations after 5. 10, 15 and 24 hours. The area under the concentration-time curve (AUC) was similar for immediate-release tablets and extended-release tablets.
Distribution
Ibuprofen is intensely bound to plasma proteins (99%). The volume of distribution (Vd) of ibuprofen is small and is approximately 0.12 – 0.2 l/kg in adults.
Metabolism
Ibuprofen is rapidly metabolized in the liver with the participation of cytochrome P450 isoenzymes, mainly the CYP2C9 isoenzyme, with the formation of two main inactive metabolites – 2-hydroxyibuprofen and 3-carboxyibuprofen. When ibuprofen is administered orally, slightly less than 90% of the ibuprofen dose taken may be found in the urine in the form of oxidative metabolites and their glucuronic conjugates. A small amount of ibuprofen is excreted unchanged in the urine.
Removal
Excretion of ibuprofen through the kidneys is rapid and complete. The half-life (T1/2) of immediate-release dosage forms is approximately two hours. Ibuprofen is almost completely eliminated from the body 24 hours after taking the last dose.
Special patient groups
Elderly patients
In elderly patients in the absence of renal failure, only small, clinically insignificant differences in the pharmacokinetic profile and urinary excretion are observed compared with young patients. Kidney failure
Increased (S)-ibuprofen plasma levels, increased (S)-ibuprofen AUC values, and increased AUC enantiomeric ratio (S/R) values were observed in patients with moderate renal impairment compared to healthy controls. In patients with end-stage renal disease on dialysis, the average free fraction of ibuprofen was about 3%, compared with 1% in healthy volunteers. Severe renal impairment may lead to accumulation of ibuprofen metabolites. The significance of this effect is unknown. Metabolites can be removed by hemodialysis.
Liver failure
The presence of alcoholic liver disease with mild or moderate liver failure did not have a significant effect on pharmacokinetic parameters.
In patients with liver cirrhosis and moderate liver failure (Child-Pugh score 6-10) treated with racemic ibuprofen, an average 2-fold increase in T1/2 was observed, and the enantiomeric ratio AUC (S/R) was significantly lower compared to healthy control patients, indicating an impairment in the metabolic transformation of (R)-ibuprofen into the active (S)-enantiomer.
Special instructions
Special instructions
Gastrointestinal bleeding, ulceration and perforation
Brufen CP should be used with caution in patients with a history of pentic ulcers and other gastrointestinal diseases, as exacerbation of these conditions is possible.
Cases of gastrointestinal bleeding, ulceration or perforation have been reported with all NSAIDs during any treatment period. These adverse events can be life-threatening and occur in the presence/absence of warning symptoms or a history of serious gastrointestinal diseases. The risk of gastrointestinal bleeding, ulceration or perforation increases with increasing doses of Brufen CP in patients with peptic ulcer disease, especially complicated by a history of bleeding or perforation, and in elderly patients. In these patients, treatment should begin with the lowest dose.
In this group of patients, as well as in patients requiring concomitant therapy with low-dose acetylsalicylic acid or other drugs that may increase the risk of gastrointestinal disease, combination therapy with gastroprotectants (for example, misoprostol or proton pump inhibitors) should be considered.
Concomitant use of Brufen CP and other NSAIDs, including selective cyclooxygenase-2 (COX-2) inhibitors, should be avoided due to an increased risk of ulceration or bleeding.
During the initial phase of treatment, patients with a history of gastrointestinal disease, especially older patients, should report any unusual abdominal symptoms (especially gastrointestinal bleeding).
Brufen CP should be used with caution in patients concomitantly receiving medications that may increase the risk of ulceration or bleeding, such as oral corticosteroids, anticoagulants (including warfarin), selective serotonin reuptake inhibitors or antiplatelet drugs, including acetylsalicylic acid.
If gastrointestinal bleeding or ulceration occurs, therapy with Brufen CP should be discontinued.
Respiratory disorders
Caution should be exercised when using Brufen CP in patients with bronchial asthma, chronic rhinitis or allergic diseases, including a history, as cases of bronchospasm, urticaria or angioedema have been reported when using Brufen CP in this group of patients.
Heart failure, renal and liver failure
Caution should be exercised when using Brufen CP in patients with renal, hepatic or heart failure, as taking NSAIDs may lead to deterioration of renal function. Concomitant therapy with multiple analgesics further increases this risk. In patients with renal, hepatic or cardiac insufficiency, use the minimum effective dose for the shortest possible period of time and monitor renal function, especially during long-term treatment.
Cardiovascular and cerebrovascular disorders
Brufen CP should be used with caution in patients with a history of heart failure or hypertension, as edema has been reported with the use of ibuprofen.
Data from epidemiological studies suggest that high dose ibuprofen (2400 mg per day) and long-term treatment may be associated with a small increase in the risk of arterial thrombotic complications, including myocardial infarction or stroke. Epidemiological studies have not shown that low dose ibuprofen (< 1200 mg per day) is associated with an increased risk of arterial thrombotic complications, particularly myocardial infarction.Treatment with Brufen CP in patients with uncontrolled hypertension, heart failure, coronary artery disease, peripheral arterial disease and/or cerebrovascular disease should only be undertaken after a careful benefit/risk assessment. A similar assessment should also be carried out before prescribing long-term treatment for patients with risk factors for developing cardiovascular diseases (such as arterial hypertension, hyperlipidemia, diabetes mellitus, smoking).Dermatological disordersVery rare cases of serious and life-threatening skin reactions, including exfoliative dermatitis, Stevens-Johnson syndrome and toxic epidermal necrolysis, have been reported with the use of NSAIDs. During the initial phase of therapy, patients are at greatest risk of developing these reactions. In most cases, the reaction develops during the first month of treatment. At the first appearance of skin rash, mucosal lesions or any other signs of hypersensitivity, use of Brufen CP should be discontinued.Renal dysfunctionCaution should be exercised when initiating Brufen CP therapy in patients with significant dehydration. There is a risk of developing kidney failure, especially in children and adolescents who are dehydrated.Long-term use of ibuprofen, like other NSAIDs, has led to the development of medullary necrosis of the kidney and other pathological changes in the kidneys. Renal toxicity has also been observed in patients in whom renal prostaglandins play a compensatory role in maintaining renal perfusion. The use of NSAIDs in this group of patients may lead to a dose-dependent decrease in prostaglandin production and, secondarily, renal blood flow, which can cause renal failure.Patients with impaired renal function, heart failure, impaired liver function, taking diuretics, ACE inhibitors, as well as elderly patients are at increased risk of this reaction. After discontinuation of NSAIDs, as a rule, the condition before the start of treatment is restored.Hematological disordersBrufen CP, like other NSAIDs, may inhibit platelet aggregation and increase bleeding time in healthy patients.Aseptic meningitisAseptic meningitis has been observed in rare cases in patients receiving ibuprofen therapy. Although aseptic meningitis is most likely to occur in patients with systemic lupus erythematosus and related connective tissue diseases, cases of aseptic meningitis have been reported in patients without this chronic disease.Elderly patientsIn elderly patients, the use of NSAIDs may be associated with an increased incidence of adverse reactions, especially perforation and gastrointestinal bleeding, which can be life-threatening.Impact on the ability to drive vehicles. Wed and fur.:May affect reaction speed. During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Ibuprofen
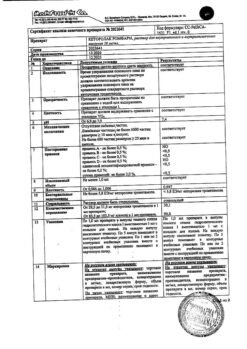
Composition
Composition
Active substance:
ibuprofen – 800 mg.
Excipients:
xanthan gum – 196.8 mg;
povidone – 25.9 mg;
stearic acid – 10.3 mg;
colloidal silicon dioxide – 3.0 mg,
hypromellose – 16.0 mg;
Opadry white M-1-7111B – 5.0 mg;
talc – 3.0 mg;
brown ink Opacode S-1-9460HV – traces.
Pregnancy
Pregnancy
Reproductive function, pregnancy and childbirth
In the first and second trimesters of pregnancy, Brufen CP can be taken only if strictly necessary, if the potential benefit to the mother outweighs the potential risk to the fetus and child. The use of Brufen CP in the third trimester of pregnancy is contraindicated and, as with the use of all prostaglandin synthesis inhibitors, carries the following risks for the fetus:
– cardiopulmonary toxicity (premature closure of the ductus arteriosus and arterial hypertension);
– impaired renal function, with a further possibility of developing renal failure and a decrease in the volume of amniotic fluid.
During childbirth, ibuprofen, like all prostaglandin synthesis inhibitors, exposes mother and newborn to the following risks:
– increased bleeding time;
– inhibition of contractile activity of the uterus, which can lead to a delay or increase in the duration of labor.
In this regard, it is not recommended to take ibuprofen during labor. The use of ibuprofen may adversely affect female fertility and is not recommended for women planning pregnancy.
If ibuprofen is prescribed to women planning pregnancy, as well as in the first or second trimesters of pregnancy, the dose should be reduced as far as possible and the duration of ibuprofen therapy should be shortened. In women experiencing difficulty conceiving or undergoing evaluation for infertility, discontinuation of ibuprofen therapy should be considered.
Breastfeeding period
Due to limited data available on the penetration of ibuprofen into breast milk in very low concentrations, the use of Brufen CP during breastfeeding is not recommended.
Contraindications
Contraindications
– hypersensitivity to the active substance or to any of the excipients;
– complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid (ASA) or other NSAIDs (including a history);
– severe heart failure;
– severe liver failure;
– active liver disease;
– severe renal failure (creatinine clearance less than 30 ml/min);
– progressive kidney diseases;
– hemophilia and other bleeding disorders (including hypocoagulation), hemorrhagic diathesis;
– history of gastrointestinal bleeding or perforation associated with previous use of NSAIDs;
– ulcerative colitis, Crohn’s disease, recurrent peptic ulcer or gastrointestinal bleeding (defined by two or more separate episodes of confirmed ulcer or bleeding), including a history;
– condition after coronary artery bypass surgery;
– confirmed hyperkalemia;
– inflammatory bowel diseases;
– intracranial hemorrhage;
– pregnancy (III trimester);
– period of breastfeeding;
– children’s age up to 12 years.
With caution:
A single episode of erosive and ulcerative disease of the gastrointestinal tract in the anamnesis (including peptic ulcer of the stomach and duodenum); simultaneous use of oral corticosteroids (including prednisolone), anticoagulants (including warfarin), antiplatelet agents (including clopidogrel), selective serotonin reuptake inhibitors (including citalopram, fluoxetine, paroxetine, sertraline); long-term use of NSAIDs; bronchial asthma, chronic rhinitis or allergic diseases (including a history); liver failure and/or chronic renal failure (creatinine clearance 30-60 ml/min); heart failure; arterial hypertension; coronary heart disease; cerebrovascular diseases; dyslipidemia/hyperlipidemia; diabetes mellitus; peripheral arterial disease; smoking; presence of H. pylori infection; frequent drinking of alcohol; severe somatic diseases; systemic lupus erythematosus or other autoimmune connective tissue diseases (increased risk of developing aseptic meningitis); blood diseases of unknown etiology (leukopenia and anemia); liver cirrhosis with portal hypertension; nephrotic syndrome; hyperbilirubinemia; gastritis; enteritis; colitis; state of dehydration; pregnancy (I-II trimester), old age.
Side Effects
Side Effects
The side effects observed with ibuprofen are common to the entire class of NSAIDs. Adverse effects can be minimized by using the minimum effective dose for the short period of time needed to relieve symptoms.
All adverse reactions considered to be at least possibly related to the use of ibuprofen are presented by organ system and frequency of occurrence: very common (≥1/10), common (≥1/100 to <1/10), uncommon (≥1/1000 to <1/100), rare (≥1/10000 to <1/100). 1/1000), very rare (< 1/10000) and frequency unknown (frequency cannot be estimated from available data).
Organ system
Frequency
Undesirable effect
Infectious diseases1
Uncommon
Rhinitis
Rarely
Aseptic meningitis
Blood and lymphatic system disorders
Rarely
Anemia (including hemolytic, aplastic)
Thrombocytopenia
Neutropenia
Agranulocytosis
Leukopenia
Immune system disorders
Rarely
Anaphylactic reaction
Mental disorders
Uncommon
Insomnia
Anxiety
Rarely
Depression
Confusion
Frequency unknown
Hallucinations
Nervous system disorders
Often
Headache
Dizziness
Uncommon
Paresthesia
Drowsiness
Rarely
Optic neuritis
Visual disorders
Uncommon
Visual impairment
Rarely
Toxic optic neuropathy
Hearing and labyrinth disorders
Uncommon
Hearing impairment
Ringing or tinnitus
Vertigo
Heart disorders
Very rarely
Worsening heart failure
Myocardial infarction
Vascular disorders3
Very rarely
Increased blood pressure
Respiratory, thoracic and mediastinal disorders
Uncommon
Worsening of bronchial asthma
Bronchospasm
Dyspnea
Gastrointestinal (GIT) disorders
Often
Dyspepsia
Diarrhea
Nausea
Vomiting (including bloody)
Abdominal pain
Flatulence
Constipation
Melena
Gastrointestinal bleeding
Uncommon
Gastritis
Stomach and/or duodenal ulcer
Ulceration of the oral mucosa
Perforation of the gastrointestinal mucosa
Very rarely
Pancreatitis
Frequency unknown
Exacerbation of colitis and Crohn’s disease
Aphthous stomatitis
Disorders of the liver and biliary tract
Uncommon
Hepatitis
Jaundice
Liver dysfunction
Very rarely
Liver failure
Disorders of the skin and subcutaneous tissues2
Often
Skin rash
Uncommon
Hives
Itchy skin
Hemorrhagic rash Angioedema Photosensitivity
Very rarely
Exudative erythema multiforme Bullous dermatosis (including Stevens-Johnson syndrome)
Toxic epidermal necrolysis (Lyell’s syndrome)
Renal and urinary tract disorders
Uncommon
Tubulointerstitial nephritis (including allergic nephritis)
Nephrotic syndrome
Kidney failure
General disorders
Often
Increased fatigue
Rarely
Edema
1 – when using NSAIDs, cases of exacerbation of inflammation caused by infections (for example, the development of necrotizing fasciitis) have been described. If a patient develops signs of infection or the infection worsens while taking ibuprofen, they should contact their doctor immediately.
2 – in exceptional cases, serious skin infection and soft tissue disorders may occur due to chickenpox infection.
3 – data from clinical and epidemiological studies indicate that the use of ibuprofen (in a high dose – 2400 mg per day) and with long-term treatment may be associated with a slight increase in the risk of arterial thrombotic complications, including myocardial infarction or stroke.
Interaction
Interaction
Due to reports of drug interactions in some patients, Brufen CP should be used with caution in patients taking any of the following medications:
Concomitant use of ibuprofen with the following drugs:
Possible effects
Other NSAIDs, including selective cyclooxygenase-2 inhibitors
Concomitant use with other NSAIDs, including selective cyclooxygenase-2 inhibitors, should be avoided due to possible additive effects.
Cardiac glycosides
NSAIDs can worsen the course of heart failure, reduce the glomerular filtration rate and increase the concentration of cardiac glycosides in the blood plasma.
Glucocorticosteroids
When using NSAIDs, the risk of developing gastrointestinal ulcers or bleeding increases.
Anticoagulants
NSAIDs may enhance the effect of anticoagulants such as warfarin or heparin. In case of simultaneous use, monitoring of blood coagulation parameters is recommended.
Probenecid
Medicines containing probenecid may delay the elimination of ibuprofen.
Antiplatelet agents and selective serotonin reuptake inhibitors (SSRIs) (eg, clopidogrel, ticlopidine)
When using NSAIDs, the risk of gastrointestinal bleeding increases.
Acetylsalicylic acid
As with the use of other drugs containing NSAIDs, the simultaneous use of ibuprofen and acetylsalicylic acid is not recommended, as the likelihood of unwanted effects increases.
Experimental data indicate that concomitant use of ibuprofen may inhibit the effect of low doses of acetylsalicylic acid on platelet aggregation. However, due to the limitations of these data and the uncertainty in extrapolating ex vivo data to the clinical situation, reliable conclusions regarding chronic ibuprofen use cannot be drawn. The development of clinically significant effects is considered unlikely with occasional use of ibuprofen.
Lithium preparations
NSAIDs may decrease lithium excretion.
Antihypertensives, beta-blockers and diuretics
NSAIDs may reduce the antihypertensive effect of antihypertensive agents, including ACE inhibitors, angiotensin II receptor antagonists, beta blockers and diuretics.
Diuretics may also increase the risk of nephrotoxicity from NSAIDs.
Methotrexate
NSAIDs may inhibit tubular secretion of methotrexate and reduce the clearance of methotrexate.
Cyclosporine
The use of NSAIDs increases the risk of nephrotoxicity.
Tacrolimus
Concomitant use of NSAIDs and tacrolimus may increase the risk of nephrotoxicity.
Zidovudine
The concomitant use of NSAIDs and zidovudine increases the risk of hematological toxicity. There is evidence of an increased risk of hemarthrosis and hematomas in HIV-positive hemophilia patients receiving concomitant treatment with zidovudine and ibuprofen.
Quinolone antibiotics
Data from animal studies suggest that NSAIDs may increase the risk of seizures associated with quinolone antibiotic use. Patients taking NSAIDs and quinolones may be at increased risk of developing seizures.
CYP2C9 isoenzyme inhibitors
Concomitant use of ibuprofen and inhibitors of the CYP2C9 isoenzyme may enhance the effect of ibuprofen (a substrate of the CYP2C9 isoenzyme). A study using voriconazole and fluconazole (CYP2C9 inhibitors) showed an increase in 8(+)-ibuprofen levels in the body by approximately 80-100%. When used concomitantly with inhibitors of the CYP2C9 isoenzyme, consider reducing the dose of ibuprofen, in particular when using high doses of ibuprofen with voriconazole or fluconazole.
Sulfonylureas
NSAIDs may enhance the effect of sulfonylureas. Rare cases of hypoglycemia have been reported in patients taking sulfonylureas and ibuprofen simultaneously.
Cholestyramine
Concomitant use of ibuprofen and cholestyramine may reduce the absorption of ibuprofen from the gastrointestinal tract. However, the clinical significance of this phenomenon is unknown.
Aminoglycosides
NSAIDs may reduce the excretion of aminoglycosides.
Herbal extracts
Concomitant use of NSAIDs and ginkgo biloba extract may increase the risk of bleeding.
Mifepristone
Due to the antiprostaglandin properties of NSAIDs, including acetylsalicylic acid, it is theoretically possible to reduce the effectiveness of the drug. Limited data suggest that concomitant use of NSAIDs on the day of prostaglandin administration does not adversely affect the efficacy of mifepristone or the effect of prostaglandins on the cervix or uterine contractions, and does not reduce the clinical effectiveness of medical termination of pregnancy.
Overdose
Overdose
Toxicity: In children and adults taking ibuprofen in doses less than 100 mg/kg, there are usually no signs or symptoms of toxicity. However, in some cases, symptomatic therapy may be required. In children, the onset of toxicity symptoms was observed after taking ibuprofen in doses of 400 mg/kg or more. In most patients who overdose on ibuprofen, symptoms appear 4-6 hours after ingestion.
Symptoms: The most commonly reported symptoms of overdose were nausea, vomiting, abdominal pain, lethargy and drowsiness. Central nervous system (CNS) disorders include headache, tinnitus, dizziness, depression, seizures and loss of consciousness. Nystagmus, metabolic acidosis, hypothermia, renal dysfunction, gastrointestinal bleeding, coma, respiratory arrest, and suppression of the central nervous system and respiratory system have also been rarely reported.
Cases of cardiovascular toxicity, including hypotension, bradycardia and tachycardia, have been reported. In cases of significant overdose, acute renal failure and liver damage may develop. Overdose with large doses of Brufen CP is usually well tolerated unless other drugs are taken at the same time.
Treatment: There is no specific antidote. In case of overdose, gastric lavage (within the first hour after administration) and maintenance therapy are recommended. If there are symptoms from the gastrointestinal tract, use antacid medications. If arterial hypotension develops, intravenous infusions and, if required, inotropic support. Drinking, forced diuresis and symptomatic therapy (correction of CBS, electrolyte balance, blood pressure).
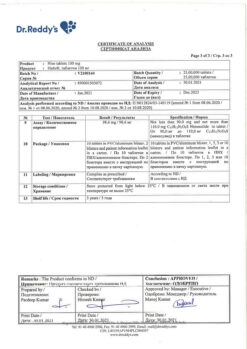
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C. Keep out of the reach of children.
Shelf life
Shelf life
3 years. Do not use the drug after the expiration date.
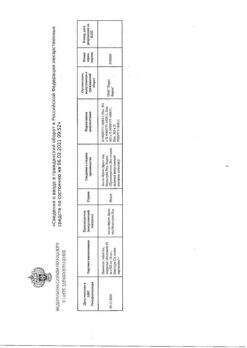
Manufacturer
Manufacturer
Famar A.V.E., Greece
Additional information
| Shelf life | 3 years. Do not use the drug after the expiration date. |
|---|---|
| Conditions of storage | At a temperature not higher than 25 ° C. Keep out of reach of children. |
| Manufacturer | Famar A.V.E., Greece |
| Medication form | sustained release tablets |
| Brand | Famar A.V.E. |
Other forms…
Related products
Buy Brufen SR, 800 mg 14 pcs with delivery to USA, UK, Europe and over 120 other countries.