No products in the cart.
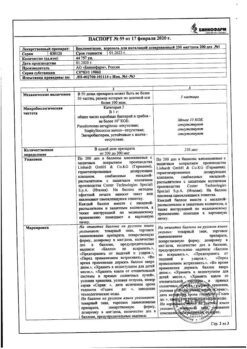
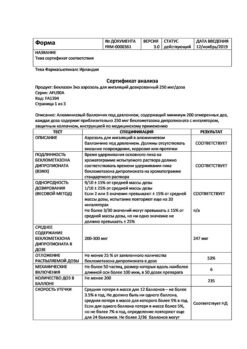
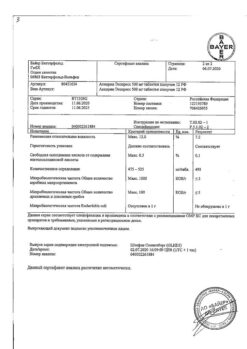
Beclomethasone, aerosol 100 mcg/dose 200 doses
€10.62 €9.29
EAN: 4610004580949
SKU: 294221
Categories: Bronchial asthma, Corticosteroid hormones, Medicine, Pain and fever
Description
Beclomethasone dipropionate is a prodrug and has weak tropicity to GCS receptors‑. ‑
It is converted under the action of esterases to the active metabolite – beclomethasone17-monopropionate ‑(B-17-MP), which has a pronounced local anti-inflammatory effect.
It reduces inflammation due to decrease in formation of chemotaxis substance (effect on “late” allergic reactions), inhibits development of “immediate” allergic reaction (conditioned by inhibition of production of arachidonic acid ‑metabolites and decrease in release of inflammatory mediators from mast cells) and improves mucociliary transport.
Beclomethasone decreases the number of mast cells in the bronchial mucosa, decreases edema of epithelium, mucus secretion by bronchial glands, bronchial hyperresponsiveness, edge accumulation of neutrophils, inflammatory exudate and lymphokine production, decreases the migration of macrophages and the intensity of infiltration and granulation.
It increases the number of active beta-adrenoreceptors, restores the patient’s response to bronchodilators and allows to reduce the frequency of their use. It has practically no resorptive action after inhalation administration.
It does not relieve bronchospasm; therapeutic effect develops gradually, usually after 5-7 days of course use of beclometasone dipropionate.
Indications
Indications
Basic therapy for various forms of bronchial asthma in adults and children over 4 years of age.
Pharmacological effect
Pharmacological effect
Beclomethasone dipropionate is a prodrug and has weak affinity for GCS receptors.
Under the influence of esterases, it is converted into an active metabolite – beclomethasone-17-monopropionate (B-17-MP), which has a pronounced local anti-inflammatory effect.
Reduces inflammation by reducing the formation of a chemotaxis substance (impact on “late” allergic reactions), inhibits the development of an “immediate” allergic reaction (due to inhibition of the production of arachidonic acid metabolites and a decrease in the release of inflammatory mediators from mast cells) and improves mucociliary transport.
Under the influence of beclomethasone, the number of mast cells in the bronchial mucosa decreases, epithelial edema, mucus secretion by bronchial glands, bronchial hyperreactivity, marginal accumulation of neutrophils, inflammatory exudate and the production of lymphokines are reduced, the migration of macrophages is inhibited, and the intensity of infiltration and granulation processes is reduced.
Increases the number of active beta-adrenergic receptors, restores the patient’s response to bronchodilators, and allows to reduce the frequency of their use. It has virtually no resorptive effect after inhalation administration.
It does not relieve bronchospasm; the therapeutic effect develops gradually, usually after 5–7 days of course use of beclomethasone dipropionate.
Special instructions
Special instructions
Before prescribing inhaled drugs, it is necessary to instruct the patient on the rules for their use, ensuring the most complete delivery of the drug to the desired areas of the lungs.
The development of oral candidiasis is most likely in patients with high levels of precipitating antibodies in the blood against the Candida fungus, which indicates a previous fungal infection. After inhalation, you should rinse your mouth and throat with water. To treat candidiasis, topical antifungal drugs can be used while continuing Beclomethasone therapy.
If patients take GCS orally, then Beclomethasone is prescribed while taking the previous dose of GCS, and the patients should be in a relatively stable condition. After about 1–2 weeks, the daily dose of oral corticosteroids begins to be gradually reduced. The dose reduction scheme depends on the duration of previous therapy and the size of the initial dose of GCS.
Regular use of inhaled corticosteroids allows, in most cases, to cancel oral corticosteroids (patients who need to take no more than 15 mg of prednisolone can be completely transferred to inhaled therapy).
However, in the first months after the transition, the patient’s condition should be carefully monitored until his pituitary-adrenal system has recovered sufficiently to ensure an adequate response to stressful situations (for example, injury, surgery or infection).
When transferring patients from taking systemic corticosteroids to inhalation therapy, allergic reactions (for example, allergic rhinitis, eczema) that were previously suppressed by systemic drugs may occur.
Patients with reduced adrenal cortex function who are transferred to inhalation treatment should have a supply of GCS and always carry a warning card with them, which should indicate that in stressful situations they need additional systemic administration of GCS (after eliminating the stressful situation, the dose of GCS can be reduced again).
A sudden and progressive worsening of asthma symptoms is a potentially dangerous condition, often life-threatening for the patient, and requires an increase in the dose of GCS. An indirect indicator of the ineffectiveness of therapy is the more frequent use of short-acting β2-agonists than before.
Beclomethasone dipropionate for inhalation is not intended for the relief of attacks, but for regular daily use. Short-acting β2-adrenergic agonists (for example, salbutamol) are used to relieve attacks.
In case of severe exacerbation of bronchial asthma or insufficient effectiveness of the therapy, the dose of inhaled beclomethasone dipropionate should be increased and, if necessary, a systemic corticosteroid and an antibiotic should be prescribed if the infection develops.
If paradoxical bronchospasm develops, you should immediately stop using Beclomethasone, assess the patient’s condition, conduct an examination and, if necessary, prescribe therapy with other drugs. With long-term use of any inhaled corticosteroids, especially in high doses, systemic effects may be observed (see “Side effects”), but the likelihood of their development is much lower than when taking corticosteroids orally.
Therefore, it is especially important that when a therapeutic effect is achieved, the dose of inhaled corticosteroids is reduced to the minimum effective dose that controls the course of the disease. At a dose of 1500 mcg/day, the drug does not cause significant suppression of adrenal function in most patients. Due to possible adrenal insufficiency, special care should be taken and regular monitoring of adrenal function indicators when transferring patients taking oral corticosteroids to treatment with beclomethasone.
It is recommended to regularly monitor the growth dynamics of children receiving inhaled corticosteroids for a long time.
Administration can be carried out using special dispensers (spacers), which improve the distribution of the drug in the lungs and reduce the risk of side effects.
Abrupt withdrawal of Beclomethasone aerosol is not recommended.
It is necessary to protect the eyes from contact with the drug. By washing after inhalation you can prevent damage to the skin of the eyelids and nose.
The Beclomethasone canister should not be pierced, disassembled or thrown into fire, even if it is empty. Like most other inhalation aerosol products, Beclomethasone may be less effective at low temperatures.
When cooling the cylinder, it is recommended to remove the inhaler nozzle from it and warm it with your hands for a few minutes.
Information about the possible effect of the drug on the ability to drive vehicles and machinery
No data available.
Active ingredient
Active ingredient
Beclomethasone
Composition
Composition
1 dose of the drug contains:
Active substance:
Beclomethasone dipropionate – 0.1 mg
(in terms of 100% substance)
Excipients:
Ethanol 96% 4.2 mg,
Norflurane (tetrafluoroethane) 84.0 mg.
Pregnancy
Pregnancy
Beclomethasone should be used during pregnancy and lactation and only if the potential benefit to the mother outweighs the possible risk to the fetus and child.
Contraindications
Contraindications
Hypersensitivity to any component of the drug.
Pulmonary tuberculosis.
Children up to 4 years old. Beclomethasone, containing 250 mcg per dose, is not intended for use in pediatrics (i.e. in children under 18 years of age).
With caution
Use for glaucoma, systemic infections (bacterial, viral, fungal, parasitic), osteoporosis, liver cirrhosis, hypothyroidism, pregnancy, and lactation.
Side Effects
Side Effects
Adverse reactions are listed depending on the anatomical and physiological classification and occurrence. The frequency of occurrence is defined as follows: very often ≥1/10, often ≥1/100 and <1/10, uncommon ≥1/1000 and <1/100, rarely ≥1/10000 and <1/1000 and very rarely <1/10000.
Infections: very often – candidiasis of the mouth and pharynx. Using a spacer and rinsing your mouth and throat with water after inhalation reduces the likelihood of these side effects.
From the immune system: uncommon – skin hypersensitivity reactions, including rash, urticaria, itching, redness and swelling of the eyes, face, lips and mucous membranes of the mouth and pharynx; very rarely – angioedema, anaphylactic reactions.
From the endocrine system: systemic effects are possible: very rarely – suppression of the function of the adrenal cortex, growth retardation in children and adolescents, cataracts, glaucoma.
From the respiratory system: often dysphonia (hoarseness of voice) or irritation of the pharyngeal mucosa, very rarely – paradoxical bronchospasm, which must be immediately relieved with an inhaled short-acting β2-adrenergic agonist. If paradoxical bronchospasm occurs, it is necessary to immediately stop using the drug in inhalations, assess the patient’s condition, conduct the necessary examination and prescribe the necessary treatment.
From the skin and subcutaneous fat: often – bruising, thinning of the skin.
Interaction
Interaction
Beclomethasone restores the patient’s response to beta-agonists, making it possible to reduce the frequency of their use.
When used together with inducers of microsomal oxidation (including phenobarbital, phenytoin, rifampicin, etc.), the effectiveness of beclomethasone may be reduced.
When used simultaneously with methandienone, estrogens, beta2-adrenergic agonists, theophylline, and systemic corticosteroids, the effectiveness of beclomethasone increases.
With simultaneous use, beclomethasone enhances the effect of beta-agonists.
Overdose
Overdose
An acute overdose of the drug can lead to a temporary decrease in the function of the adrenal cortex, which does not require emergency treatment, since the function of the adrenal cortex is restored within a few days, as confirmed by the concentration of cortisol in plasma.
In case of chronic overdose, persistent suppression of the function of the adrenal cortex can be observed. In such cases, it is recommended to monitor the reserve function of the adrenal cortex.
In case of overdose, treatment with beclomethasone dipropionate can be continued in doses sufficient to maintain the therapeutic effect.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25°C.
Keep away from heating systems and direct sunlight.
Keep out of the reach of children!
Protect from falls and impacts.
Shelf life
Shelf life
3 years. Do not use after the expiration date.
Manufacturer
Manufacturer
Binnopharm, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25°C. Store away from heating system and direct sunlight. Store out of the reach of children! Prevent dropping or knocking. |
| Manufacturer | Binnopharm, Russia |
| Medication form | metered aerosol for inhalation |
| Brand | Binnopharm |
Other forms…
Related products
Buy Beclomethasone, aerosol 100 mcg/dose 200 doses with delivery to USA, UK, Europe and over 120 other countries.