No products in the cart.
Azilet, tablets 1 mg 100 pcs
€480.76 €443.78
Description
Pharmacotherapeutic group: antiparkinsonian drug – MAOI inhibitor
ATCode: N04BD02
Pharmacological properties
Pharmacodynamics
Razagiline is a selective irreversible inhibitor of monoamine oxidase type B (MAO-B), the enzyme that determines 80% of monoamine oxidase activity in the brain and dopamine metabolism. It is 30-80 times more active against MAO-B than against another type of this enzyme, MAO-A. As a result of the drug’s inhibitory effect on MAO-B in the central nervous system, dopamine levels increase and the formation of toxic free radicals, excessive formation of which is observed in patients with Parkinson’s disease, is reduced. Razagiline also has a neuroprotective effect.
In contrast to non-selective MAO inhibitors, the drug in therapeutic doses does not block metabolism of biogenic amines from food (e.g., tyramine) and therefore does not cause tyramine-dependent hypertensive syndrome (“cheese effect”).
Pharmacokinetics
Rasagiline is rapidly absorbed after oral administration; its maximum plasma concentration (Cmax) is reached after 0.5 hours. Absolute bioavailability of the drug after a single administration is about 36%. Food has no effect on the time of reaching maximum blood concentration of Rasagilin, however, when fatty food is consumed, Cmax and area under the drug concentration curve (AUC) are reduced by 60% and 20% respectively. Pharmacokinetics of the drug is linear in the dose range of 0.5-2 mg. The binding to plasma proteins varies from 60 to 70%.
Razagiline is almost completely metabolized in the liver. Biotransformation occurs by N-dealkylation and/or hydroxylation to form the main biologically inactive metabolite, 1-aminoindan, and two other metabolites, 3-hydroxy-N-propargyl-1-aminoindan and 3-hydroxy-l-aminoindan. The drug is metabolized with the participation of the CYP1A2 isoform of the cytochrome P450 system.
Rasagiline is excreted mainly by the kidneys (more than 60%) and to a lesser extent through the intestine (more than 20%). Less than 1% of the administered dose of the drug is excreted unchanged. The elimination half-life is 0.6-2 hours.
Parameters of pharmacokinetics of rasagiline are practically unchanged in patients with mild and moderate renal insufficiency. In mild hepatic insufficiency there may be increase in AUC and Cmax parameters by 80% and 38%, and in patients with moderate hepatic impairment these parameters reach more than 500% and 80%, respectively.
Indications
Indications
Monotherapy or combination therapy for Parkinson’s disease (with levodopa).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antiparkinsonian drug – MAO inhibitor
ATX code: N04BD02
Pharmacological properties
Pharmacodynamics
Rasagiline is a selective irreversible inhibitor of monoamine oxidase type B (MAO-B), an enzyme responsible for 80% of monoamine oxidase activity in the brain and dopamine metabolism. It is 30-80 times more active against MAO-B than against another type of this enzyme, MAO-A. As a result of the inhibitory effect of the drug on MAO-B, the level of dopamine in the central nervous system increases and the formation of toxic free radicals, excessive formation of which is observed in patients with Parkinson’s disease, decreases. Rasagiline also has neuroprotective effects.
Unlike non-selective MAO inhibitors, the drug in therapeutic doses does not block the metabolism of biogenic amines (for example, tyramine) supplied with food, and therefore does not cause tyramine-induced hypertensive syndrome (“cheese effect”).
Pharmacokinetics
Rasagiline is rapidly absorbed after oral administration; its maximum concentration in blood plasma (Cmax) is reached after 0.5 hours. The absolute bioavailability of the drug after a single dose is about 36%. Food does not affect the time to reach the maximum concentration of rasagiline in the blood, however, when consuming a fatty meal, Cmax and area under the drug concentration curve (AUC) are reduced by 60% and 20%, respectively. The pharmacokinetics of the drug is linear in the dose range of 0.5-2 mg. The binding to plasma proteins ranges from 60 to 70%.
Rasagiline is almost completely metabolized in the liver. Biotransformation is carried out by N-dealkylation and/or hydroxylation with the formation of the main biologically inactive metabolite – 1-aminoindane, as well as two other metabolites – 3-hydroxy-N-propargyl-1 aminoindane and 3-hydroxy-l-aminoindane. Metabolism of the drug is carried out with the participation of the CYP1A2 isoform of the cytochrome P450 system.
Rasagiline is excreted primarily by the kidneys (more than 60%) and to a lesser extent through the intestines (more than 20%). Less than 1% of the administered dose of the drug is excreted unchanged. The half-life is 0.6-2 hours.
The pharmacokinetic parameters of rasagiline remain virtually unchanged in patients with mild to moderate renal impairment. In mild liver failure, an increase in AUC and Cmax values of 80% and 38% may be observed, and in patients with moderate liver dysfunction, these parameters reach more than 500% and 80%, respectively.
Special instructions
Special instructions
The simultaneous use of Azilect® and fluoxetine or fluvoxamine should be avoided (see section “Interaction with other drugs”). The interval between stopping fluoxetine and starting treatment with Azilect® should be 5 weeks, and between stopping the drug Azilect® and starting fluoxetine or fluvoxamine should be 14 days.
Cases of impulsive personality disorder have been reported in patients treated with dopamine receptor agonists and/or other dopaminomimetics. The same disorders were observed in the post-registration period in patients taking the drug Azilect® (see section “Side effects”). Patients should be monitored for the possibility of developing impulsive personality disorder. Patients and caregivers should be informed of the possibility of developing behavioral disturbances in patients taking Azilect®, including compulsive behavior, obsessions, gambling addiction, increased libido, hypersexuality, impulsive behavior and compulsive buying or acquiring.
The simultaneous use of Azilect® with dextromethorphan, with sympathomimetics or complex anti-cold medications for oral or nasal use containing ephedrine or pseudoephedrine is not recommended (see section “Interaction with other drugs”).
There is evidence that Parkinson’s disease, and not the use of any drug, including Azilect®, is a risk factor for the development of skin cancer, in particular melanoma (see section “Side effects”). It is necessary to warn the patient about the need to consult a doctor if any pathological changes in the skin appear.
It must be borne in mind that symptoms such as hallucinations and confusion that appear during treatment with Azilect® can be considered both as a manifestation of Parkinson’s disease and as undesirable reactions of the drug Azilect® (see section “Side effects”).
Azilect® should be used with caution in patients with mild liver failure. The use of Azilect® in patients with moderate liver dysfunction is not recommended. If the severity of liver failure changes from mild to moderate, use of the drug Azilect® must be discontinued (see section “Pharmacological properties” (“Pharmacokinetics”)).
Excessive daytime sleepiness and sudden sleep episodes
Rasagiline may cause excessive daytime sleepiness and sometimes, especially when used with dopaminergic drugs, episodes of sudden sleep onset. Patients should be informed about this.
Patients should also be warned of the possible additive effects of sedatives, alcohol, or other central nervous system depressants (eg, benzodiazepines, antipsychotics, antidepressants) when combined with rasagiline or when taking concomitant medications that increase rasagiline plasma levels (eg, ciprofloxacin).
Influence on the ability to drive vehicles and machinery
Given the possibility of significant side effects from the central nervous system during treatment with Azilect®, patients should be informed about the need to be careful when driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions. Patients with drowsiness or who have experienced sudden sleepiness should not drive or engage in potentially hazardous activities until they are sure that the drug does not have an adverse effect.
Active ingredient
Active ingredient
Rasagiline
Composition
Composition
Tablets are white or almost white, round, flat-cylindrical, chamfered, with “GIL 1” engraved on one side of the tablet.
1 tab. rasagiline mesylate 1.56 mg, which corresponds to the content of rasagiline 1 mg
Excipients:
mannitol – 159.24 mg,
colloidal silicon dioxide – 1.2 mg,
corn starch – 20 mg,
pregelatinized corn starch – 20 mg,
stearic acid – 4 mg,
talc – 4 mg.
Pregnancy
Pregnancy
There are no data on the use of rasagiline in pregnant women. Results from animal studies do not indicate any direct or indirect adverse effects on pregnancy, embryofetal development, childbirth or postnatal development. If it is necessary to use rasagiline in pregnant women, it is necessary to balance the expected benefit for the mother and the risk to the fetus.
Experimental evidence suggests that rasagiline inhibits prolactin secretion and may thus suppress lactation. There is no information about the penetration of rasagiline into breast milk.
If it is necessary to use rasagiline during breastfeeding, it is necessary to compare the expected benefits for the mother and child.
Contraindications
Contraindications
hypersensitivity to rasagiline or any of the components of the drug;
simultaneous use with other MAO inhibitors (including medications and nutritional supplements containing St. John’s wort), pethidine. The interval between discontinuation of rasagiline and initiation of therapy with these drugs should be at least 14 days;
moderate to severe liver failure (classes B and C on the Child-Pugh scale);
children under 18 years of age (no data on effectiveness and safety).
With caution: mild liver failure (class A on the Child-Pugh scale); simultaneous use with SSRIs (including fluoxetine, fluvoxamine), SNRIs, tricyclic and tetracyclic antidepressants, powerful inhibitors of the CYP1A2 isoenzyme.
Side Effects
Side Effects
In clinical studies, the following adverse reactions were most often identified: with monotherapy – headache, depression, dizziness, flu, rhinitis; during therapy as an adjunct to levodopa therapy – dyskinesia, orthostatic hypotension, falls, abdominal pain, nausea, vomiting, dry mouth; in both treatment regimens – musculoskeletal pain, back and neck pain, arthralgia.
The list below describes adverse reactions that were reported with increased frequency in placebo-controlled studies in patients receiving rasagiline 1 mg/day.
The frequency of occurrence of adverse reactions is defined as follows: very common (≥1/10), common (≥1/100 to <1/10), uncommon (≥1/1000 to <1/100), rare (≥1/10000 to <1/1000), very rare (<1/10000), unknown - the frequency of reactions cannot be determined based on the available data.
When used as monotherapy
Infectious and parasitic diseases: often – influenza.
Benign, malignant and unspecified neoplasms (including cysts and polyps): often – skin cancer.
Disorders of the blood and lymphatic system: often – leukopenia.
From the immune system: often – allergies.
From the side of metabolism and nutrition: infrequently – loss of appetite.
From the mental side: often – depression, hallucinations*; unknown – impulsive disorders*.
From the nervous system: very often – headache; infrequently – cerebrovascular accident; unknown – excessive daytime sleepiness, episodes of sudden sleep onset, serotonin syndrome*.
From the side of the organ of vision: often – conjunctivitis.
From the organ of hearing and labyrinthine disorders: often – vertigo.
From the side of the heart: often – angina pectoris; infrequently – myocardial infarction.
Vascular disorders: unknown – hypertension*.
From the gastrointestinal tract: often – bloating.
From the respiratory system: often – rhinitis.
From the skin and subcutaneous tissues: often – dermatitis; infrequently – vesicular-bullous rash.
From the musculoskeletal system and connective tissue: often – musculoskeletal pain, neck pain, arthritis.
From the kidneys and urinary tract: often – the urge to urinate.
General disorders and disorders at the injection site: often – fever, malaise.
When used as adjuvant therapy
Benign, malignant and unspecified neoplasms (including cysts and polyps): uncommon – cutaneous melanoma*.
Metabolic and nutritional disorders: often – loss of appetite.
From the psyche: often – hallucinations*, nightmares; infrequently – confusion, impulsive disorders*.
From the nervous system: very often – dyskinesia; often – dystonia, carpal tunnel syndrome, imbalance; infrequently – cerebrovascular accident; unknown – excessive daytime sleepiness, episodes of sudden sleep onset, serotonin syndrome*.
From the heart: infrequently – angina pectoris.
Vascular disorders: often – orthostatic hypotension*, unknown – hypertension*.
From the digestive system: often – abdominal pain, constipation, nausea and vomiting, dry mouth.
From the skin and subcutaneous tissues: often – rash.
From the musculoskeletal and connective tissue side: often – arthralgia, neck pain;
Research results: often – weight loss.
Injuries, poisoning and complications of procedures: often – falls.
Parkinson’s disease causes hallucinations and confusion. According to post-marketing experience, these symptoms were observed in patients with Parkinson’s disease receiving rasagiline.
* – See description of individual adverse reactions.
See also the section “Interaction with other drugs”.
Description of selected adverse reactions
Orthostatic hypotension
In blinded, placebo-controlled studies, severe orthostatic hypotension was reported in one patient (0.3%) in the rasagiline group (the drug was used as adjuvant therapy); none were observed in the placebo group. Clinical trial data also suggest that orthostatic hypotension occurs most frequently in the first two months of rasagiline treatment and decreases over time.
Hypertension
Increases in blood pressure (BP), including rare cases of hypertensive crises, have been reported with the use of rasagiline during the post-marketing period in patients consuming foods rich in tyramine in their diet.
In the post-registration period, a case of increased blood pressure was reported in a patient who used the ophthalmic vasoconstrictor tetrahydrozoline and was simultaneously treated with rasagiline.
Impulsive personality disorder
Cases of increased libido, hypersexuality, gambling addiction, compulsive need to buy or acquire, overeating and compulsive overeating, kleptomania, dermatillomania have been reported in patients treated with dopamine receptor agonists and/or other dopaminomimetics. A similar pattern of impulsive personality disorder was observed in the post-marketing period in patients taking rasagiline, which was characterized by compulsive and impulsive behavior and obsessions.
Excessive daytime sleepiness and sudden sleep episodes
Excessive daytime sleepiness may occur in patients taking dopamine agonists and/or other dopaminergic drugs. Cases of similar excessive daytime sleepiness have been reported during treatment with rasagiline.
Cases of sudden sleep onset during patients performing normal daily activities have also been reported when rasagiline was used with dopaminergic drugs. Some patients did not show any warning signs, such as excessive sleepiness, before falling asleep. In some cases, such events were reported more than 1 year after the start of treatment.
Hallucinations
Parkinson’s disease causes hallucinations and confusion. According to post-marketing experience, these symptoms were observed in patients with Parkinson’s disease receiving rasagiline.
Serotonin syndrome
In clinical studies of rasagiline, co-administration of rasagiline with fluoxetine or fluvoxamine was not permitted. However, the following antidepressants were approved at the indicated doses: amitriptyline not more than 50 mg/day, trazodone not more than 100 mg/day, citalopram not more than 20 mg/day, sertraline not more than 100 mg/day and paroxetine not more than 30 mg/day. Serious adverse reactions have been reported and caution should be exercised during concomitant use of SSRIs, SNRIs, tricyclic/tetracyclic antidepressants and MAO inhibitors.
During post-marketing surveillance, cases of the development of potentially life-threatening serotonin syndrome, manifested by agitation, confusion, rigidity, fever and myoclonus, have been reported in patients receiving antidepressants, meperidine (pethidine), tramadol, methadone or propoxyphene concomitantly with rasagiline.
Melanoma
The incidence of cutaneous malignant melanoma in placebo-controlled clinical trials was 2/380 (0.5%) in the rasagiline 1 mg group given as an adjuvant to levodopa therapy versus 1/388 (0.3%) incidence in the placebo group. Cases of melanoma have also been reported in the post-registration period (see also section “Special instructions”).
Interaction
Interaction
The simultaneous use of rasagiline with other MAO inhibitors, including medications and dietary supplements containing St. John’s wort, is contraindicated, because there is a risk of developing a severe hypertensive crisis due to non-selective MAO inhibition.
The development of serious adverse reactions has been reported with the simultaneous use of pethidine and MAO inhibitors, including selective MAO-B inhibitors. Concomitant use of rasagiline and pethidine is contraindicated.
Interactions between MAO inhibitors and sympathomimetic drugs have been reported when used concomitantly. Due to the MAO-inhibiting properties of rasagiline, concomitant use of rasagiline with sympathomimetics, such as decongestants or oral or nasal complex cold products containing ephedrine or pseudoephedrine, is not recommended.
Interactions between dextromethorphan and non-selective MAO inhibitors have been reported when used concomitantly. However, due to the MAO inhibitory properties of rasagiline, concomitant use of rasagiline with dextromethorphan and combination medicinal products containing it is not recommended.
The simultaneous use of rasagiline with fluoxetine or fluvoxamine should be avoided (see section “Special instructions”).
The development of serious adverse reactions has been reported with the simultaneous use of SSRIs, SNRIs, tricyclic and tetracyclic antidepressants with MAO inhibitors. Due to the property of rasagiline to inhibit MAO, caution must be exercised when used simultaneously with SSRIs, SNRIs, tricyclic and tetracyclic antidepressants.
In patients with Parkinson’s disease receiving rasagiline as an adjuvant to long-term levodopa therapy, levodopa had no significant effect on rasagiline clearance.
In vitro studies have shown that the main enzyme involved in the metabolism of rasagiline is the CYP1A2 isoenzyme. The simultaneous use of ciprofloxacin and rasagiline increases the AUC of the latter by 83%. The simultaneous use of rasagiline and theophylline (a substrate of the CYP1A2 isoenzyme) did not affect the pharmacokinetics of either of them. Thus, potent inhibitors of the CYP1A2 isoenzyme may alter the plasma concentrations of rasagiline and require careful simultaneous use.
There is a risk that due to the induction of the CYP1A2 isoenzyme in smoking patients, the concentration of rasagiline in the blood plasma may decrease.
In vitro studies have shown that rasagiline at a concentration of 1 mcg/mL (equivalent to a concentration of 160 times the mean Cmax (5.9-8.5 ng/mL) after repeated doses of 1 mg rasagiline in patients with Parkinson’s disease) does not inhibit CYP1A2, CYP2A6, CYP2C9, CYP2C19, CYP2D6, CYP2E1, CYP3A4 and CYP4A. This indicates that therapeutic concentrations of rasagiline are not likely to be affected clinically by substrates of these isoenzymes.
With simultaneous use of entacapone with rasagiline, the clearance of the latter increased by 28%.
Clinical studies of the interaction of tyramine and rasagiline in volunteers and patients with Parkinson’s disease (0.5-1 mg/day rasagiline or placebo as adjunctive therapy to levodopa for 6 months without restriction of tyramine intake) showed that there is no interaction between rasagiline and tyramine and rasagiline can be safely used without restriction of tyramine in the diet.
Overdose
Overdose
Symptoms of drug overdose are similar to those of overdose with non-selective MAO inhibitors (including arterial hypertension, postural hypotension).
Treatment: there is no specific antidote. Gastric lavage, intake of activated carbon, symptomatic therapy.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C
Shelf life
Shelf life
3 years
Manufacturer
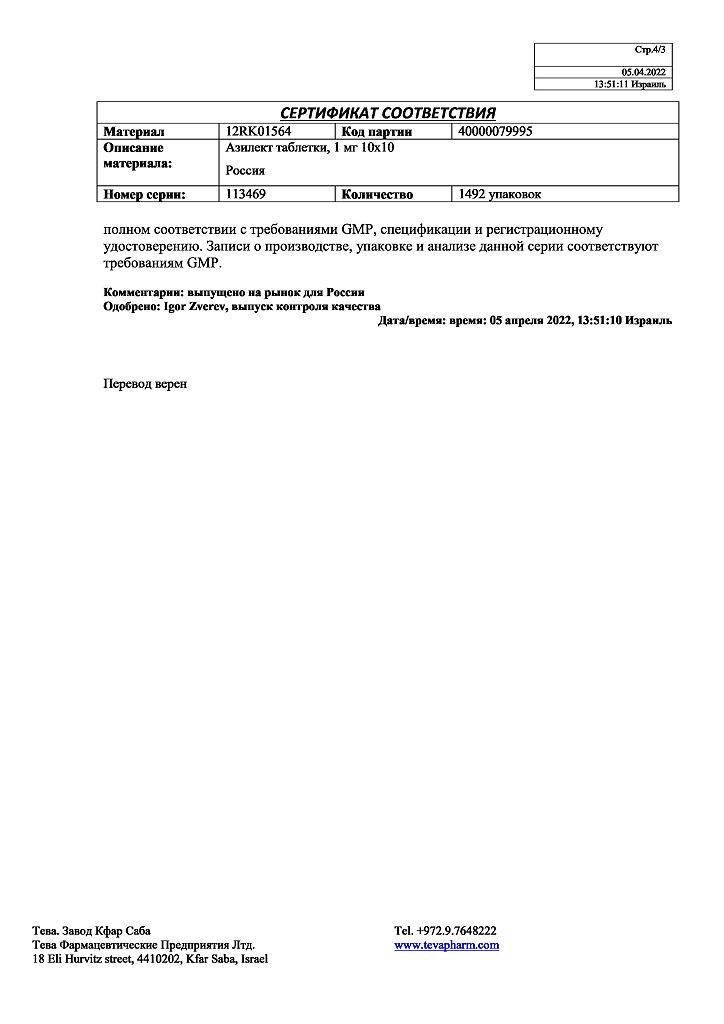
Manufacturer
Teva Pharmaceutical Enterprises Ltd., Israel
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | Teva Pharmaceutical Enterprises Ltd, Israel |
| Medication form | pills |
| Brand | Teva Pharmaceutical Enterprises Ltd |
Related products
Buy Azilet, tablets 1 mg 100 pcs with delivery to USA, UK, Europe and over 120 other countries.