No products in the cart.
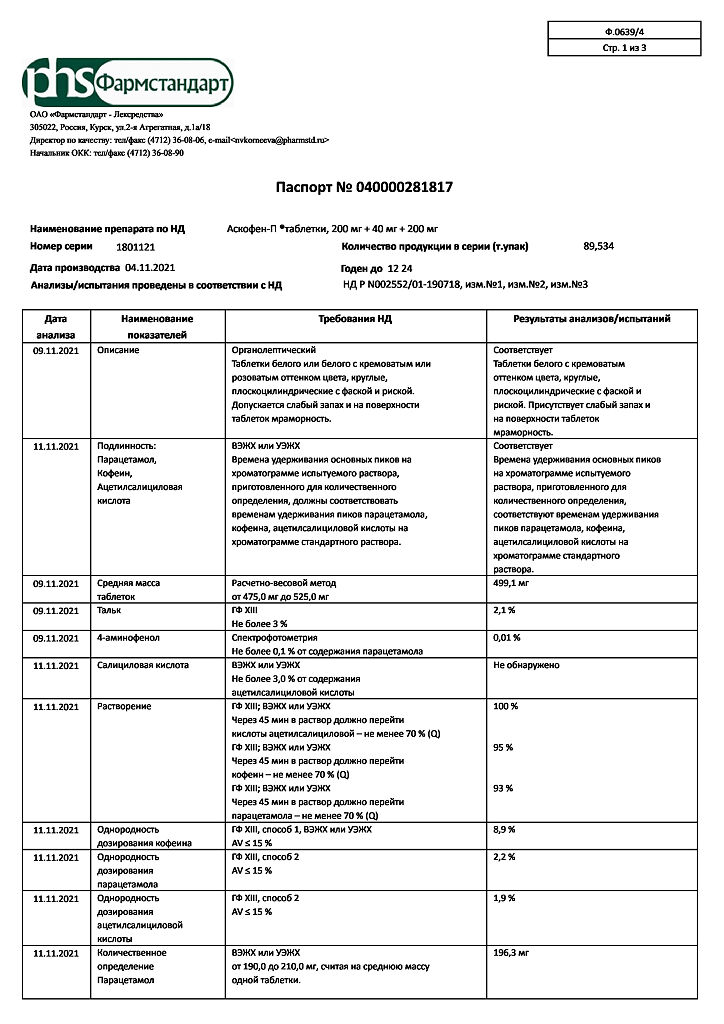
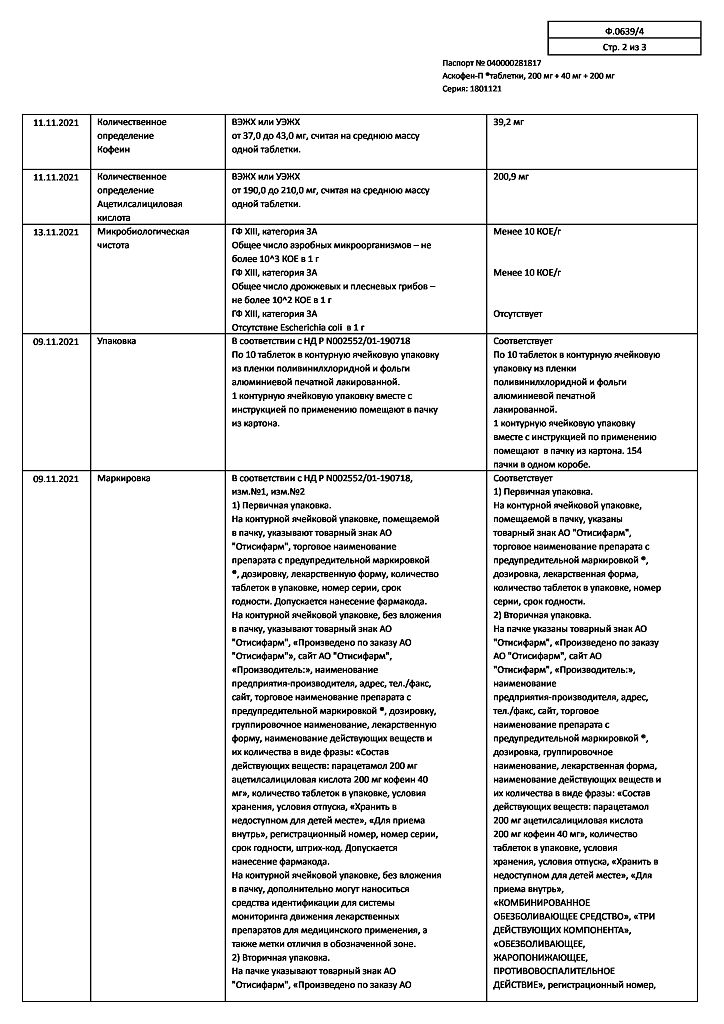
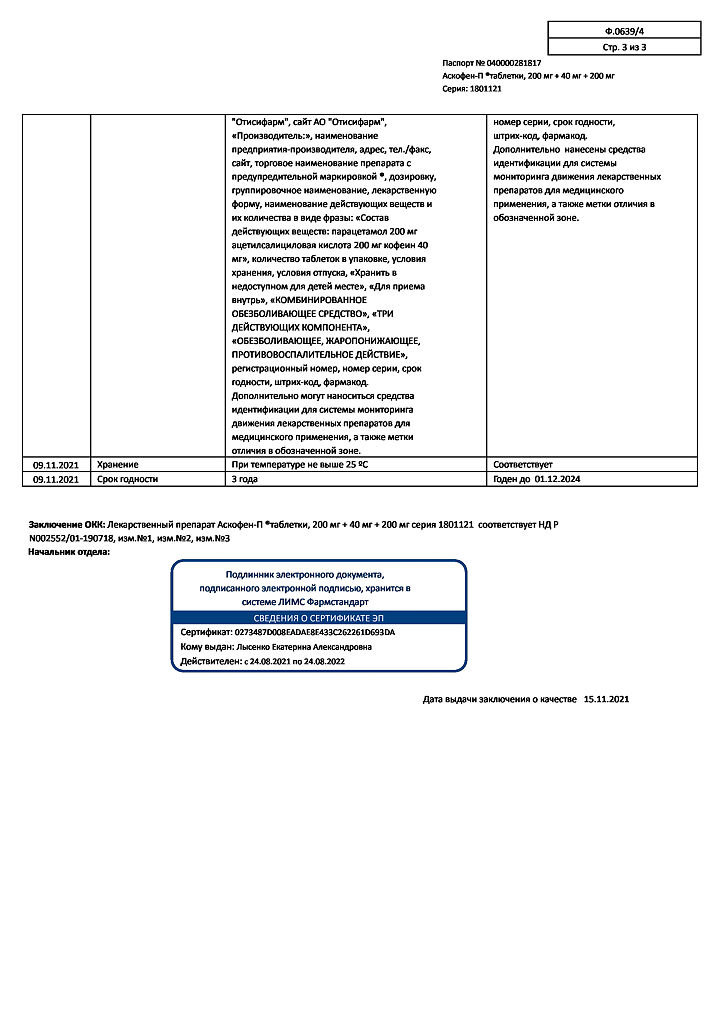
Ascophen-P, tablets 10 pcs
€3.28 €2.98
Description
Pharmacotherapeutic group: analgesic combined (non-steroidal anti-inflammatory agent + analgesic non-narcotic agent + psychostimulant)
ATX code: N02BA71
Pharmacological properties
Pharmacodynamics:
Askophen-P® is a combination drug, the action of which is determined by the components in its composition.
Acetylsalicylic acid (ASA) has antipyretic and anti-inflammatory effects, reduces pain, especially caused by inflammation, as well as inhibits thrombosis, improves microcirculation in the inflammation focus. The mechanism of action of ASA is associated with inhibition of cyclooxygenases 1 and 2, which regulate the synthesis of prostaglandins.
Caffeine increases reflex excitability of the spinal cord, excites respiratory and vasomotor centers, dilates blood vessels of skeletal muscles, brain, heart and kidneys, reduces platelet aggregation; it reduces sleepiness and feeling of fatigue and increases mental and physical performance.
In this combination, the low-dose caffeine has almost no simulative effect on the central nervous system, increases the tone of cerebral blood vessels and helps to accelerate blood flow.
Paracetamol has antipyretic, analgesic and weak anti-inflammatory effects, due to its effect on the thermoregulation center in the hypothalamus and a weak ability to inhibit the synthesis of prostaglandins in peripheral tissues.
Pharmacokinetics
Acetylsalicylic acid (ASA): absorption is complete when taken orally. During absorption it undergoes presystemic elimination in the intestinal wall and systemic elimination in the liver by deacetylation.
The resorbed part is rapidly hydrolyzed by cholinesterases and albumin esterase, so the half-life is not more than 15-20 minutes. Binding with plasma proteins (albumin) is 75-90%. Time to reach maximum concentration (Tmax) – 2 hours. It is metabolized mainly in liver and is eliminated by active secretion in renal tubules as salicylate (60%) and its metabolites.
The elimination rate depends on the dose: at low doses the elimination half-life is 2-3 hours, with increasing doses it can increase to 15-30 hours.
Paracetamol: absorption is high, Tmax is reached after 0.5-2 hours and is 5-20 mcg/ml, binding to plasma proteins is 15%. It penetrates through the blood-brain barrier. It is metabolized in liver (90-95%) with formation of active and inactive metabolites with glutathione and CYP2E1.
In case of glutathione deficiency these metabolites can block the enzyme systems of hepatocytes and cause their necrosis. The elimination half-life is 1-4 hours. It is excreted by kidneys as metabolites. Only 3% is eliminated unchanged. In elderly patients the drug clearance is decreased and the half-life is increased.
Caffeine: is completely and quickly absorbed in the gastrointestinal tract, Tmax is reached after 50-75 minutes and is 1.58-1.76 mg/l. It is rapidly distributed in all organs and tissues of the body, easily penetrates through the blood-brain barrier and the placenta. Binding with blood proteins is 25-36%.
More than 90% is metabolized in the liver. In adults about 80% of caffeine dose is metabolized to paraxanthine, about 10% to theobromine and about 4% to theophylline. The half-life in adults is 3.9-5.3 hours (sometimes up to 10 hours) Excretion of caffeine and its metabolites is done by kidneys (1-2% of adults excrete unchanged).
Indications
Indications
Pain syndrome of mild and moderate severity (of various origins): headache, migraine, toothache, neuralgia, myalgia, arthralgia, algodismenorrhea.
Feverish syndrome: for acute respiratory diseases, influenza.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: combined analgesic (non-steroidal anti-inflammatory drug + analgesic non-narcotic drug + psychostimulant)
ATX code: N02BA71
Pharmacological properties
Pharmacodynamics:
Askofen-P® is a combination drug, the effect of which is determined by the components included in its composition.
Acetylsalicylic acid (ASA) has an antipyretic and anti-inflammatory effect, relieves pain, especially caused by the inflammatory process, and also inhibits thrombus formation, improves microcirculation in the area of inflammation. The mechanism of action of ASA is associated with the suppression of cyclooxygenases 1 and 2, which regulate the synthesis of prostaglandins.
Caffeine increases the reflex excitability of the spinal cord, stimulates the respiratory and vasomotor centers, dilates the blood vessels of skeletal muscles, brain, heart, kidneys, reduces platelet aggregation; reduces drowsiness, fatigue, increases mental and physical performance.
In this combination, caffeine in a small dose has virtually no simulating effect on the central nervous system, increases the tone of cerebral vessels and helps accelerate blood flow.
Paracetamol has an antipyretic, analgesic effect and a weak anti-inflammatory effect, which is associated with its effect on the thermoregulation center in the hypothalamus and a weak ability to inhibit the synthesis of prostaglandins in peripheral tissues.
Pharmacokinetics
Acetylsalicylic acid (ASA): when taken orally, absorption is complete. During absorption, it undergoes presystemic elimination in the intestinal wall and systemic elimination in the liver by deacetylation.
The resorbed part is quickly hydrolyzed by cholinesterases and albuminesterase, so the half-life is no more than 15-20 minutes. Communication with plasma proteins (albumin) – 75-90%. The time to reach maximum concentration (Tmax) is 2 hours. Metabolized mainly in the liver. It is excreted by active secretion in the kidney tubules in the form of salicylate (60%) and its metabolites.
The rate of elimination depends on the dose: when taking small doses, the half-life is 2-3 hours, with increasing doses it can increase to 15-30 hours.
Paracetamol: absorption is high, Tmax is reached after 0.5-2 hours and is 5-20 mcg/ml, binding to plasma proteins is 15%. Penetrates the blood-brain barrier. Metabolized in the liver (90-95%) with the formation of active and inactive metabolites with the participation of glutathione, as well as CYP2E1.
With a lack of glutathione, these metabolites can block the enzyme systems of hepatocytes and cause their necrosis. The half-life is 1-4 hours. It is excreted by the kidneys in the form of metabolites. Only 3% is excreted unchanged. In elderly patients, the clearance of the drug decreases and the half-life increases.
Caffeine: completely and quickly absorbed from the gastrointestinal tract, Tmax is reached after 50-75 minutes and is 1.58-1.76 mg/l. It is quickly distributed in all organs and tissues of the body, easily penetrates the blood-brain barrier and the placenta. Communication with blood proteins – 25-36%.
More than 90% is metabolized in the liver. In adults, about 80% of a caffeine dose is metabolized to paraxanthine, about 10% to theobromine, and about 4% to theophylline. The half-life in adults is 3.9-5.3 hours (sometimes up to 10 hours). Caffeine and its metabolites are excreted by the kidneys (1-2% are excreted unchanged in adults).
Special instructions
Special instructions
General
This medicine should not be taken at the same time as medicines containing ASA or paracetamol.
As with other migraine treatments, caution should be exercised to rule out other potentially serious neurological disorders before initiating treatment for suspected migraine in patients who have not previously been diagnosed with migraine or in those whose migraine presents with atypical symptoms.
If patients vomit during >20% of migraine attacks or require bed rest during >50% of migraine attacks, the drug should not be used.
If the migraine does not stop after taking the first two tablets of the drug, you should seek medical help.
The drug should not be used if the patient has had more than 10 headache attacks per month for at least the last three months. In this case, headache due to excessive use of drugs should be suspected and treatment should be discontinued. Additionally, patients should seek medical attention. Caution should be used in patients with risk factors for dehydration, such as vomiting, diarrhea, or before or after major surgery.
Due to its pharmacodynamic properties, the drug can mask the signs and symptoms of infection.
Due to the content of acetylsalicylic acid in the drug
The drug should be used with caution in patients with gout, impaired renal or hepatic function, dehydration, uncontrolled hypertension, glucose-6-phosphate dehydrogenase deficiency and diabetes mellitus.
Due to ASA inhibition of platelet aggregation, the drug may lead to an increase in bleeding time during and after surgical interventions (including minor ones, such as tooth extraction).
The drug should not be used simultaneously with anticoagulants and other drugs that interfere with blood clotting, without medical supervision (see section “Interaction with other drugs”). Patients with bleeding disorders should be closely monitored. Caution should be exercised in case of metro- or menorrhagia.
If a patient develops bleeding or ulceration of the gastrointestinal tract while taking the drug, it must be discontinued immediately. Potentially fatal bleeding, ulceration, and perforation of the gastrointestinal tract may occur at any time during treatment with any NSAID, with or without a history of precursors and severe gastrointestinal complications.
These complications tend to be more severe in older patients. Alcohol, glucocorticosteroids and NSAIDs may increase the risk of gastrointestinal bleeding (see section “Interaction with other drugs”). The drug may contribute to the development of bronchospasm and the occurrence of exacerbation of bronchial asthma (including bronchial asthma caused by intolerance to analgesics) or other hypersensitivity reactions.
Risk factors include bronchial asthma, seasonal allergic rhinitis, nasal polyposis, chronic obstructive pulmonary disease, chronic respiratory tract infections (especially those associated with symptoms characteristic of allergic rhinitis). Such effects may also occur in patients with allergic reactions (eg, skin reactions, including itching and urticaria) to other substances.
Particular caution is recommended in such patients.
Children under 18 years of age should not be prescribed medications containing acetylsalicylic acid as an antipyretic, since in the case of a viral infection they can increase the risk of Reye’s syndrome.
Symptoms of Reye’s syndrome are hyperpyrexia, prolonged vomiting, metabolic acidosis, nervous system and mental disorders, hepatomegaly and liver dysfunction, acute encephalopathy, respiratory failure, convulsions, coma.
ASA may distort the results of laboratory tests of thyroid function due to false-positive low concentrations of levothyroxine (T4) and triiodothyronine (T3) (see section “Interaction with other drugs”).
Due to the content of paracetamol in the preparation
Caution should be exercised when prescribing the drug to patients with impaired renal or hepatic function or alcohol dependence.
The risk of paracetamol poisoning is increased in patients taking other potentially hepatotoxic drugs or drugs that induce liver microsomal enzymes (eg, rifampicin, isoniazid, chloramphenicol, hypnotics and anticonvulsants including phenobarbital, phenytoin and carbamazepine).
Patients with a history of alcoholism are at particular risk for liver damage (see section “Interaction with other drugs”).
When using the drug, serious skin reactions may develop, such as acute generalized exanthematous pustulosis, Stevens-Johnson syndrome, toxic epidermal necrolysis, which can be fatal.
Patients should be informed of the signs of serious skin reactions. The drug should be discontinued at the first manifestation of skin reactions or any other signs of hypersensitivity.
Due to the caffeine content of the product
The drug should be prescribed with caution to patients with gout, hyperthyroidism and arrhythmia.
When using the drug, you should limit your consumption of products containing caffeine, since excess caffeine intake can lead to nervousness, irritability, insomnia and, in some cases, increased heart rate.
Effect on laboratory tests
High doses of ASA can distort the results of a number of clinical and biochemical laboratory studies.
The use of paracetamol may affect the results of the determination of uric acid using the phosphotungstic acid method and the glycemic glucose oxidase/peroxidase method.
Caffeine may reverse the effects of dipyridamole on myocardial blood flow, thereby confounding the results of this study. During the study, it is necessary to refrain from taking caffeine for 8-12 hours.
Impact on the ability to drive vehicles and machinery
While using the drug, you should refrain from driving vehicles and operating other mechanisms, because Caffeine, which is part of the drug, can cause problems with concentration and reaction speed, and acetylsalicylic acid, also included in the drug, can in rare cases cause dizziness.
Active ingredient
Active ingredient
Acetylsalicylic acid, Caffeine, Paracetamol
Composition
Composition
Active ingredients:
paracetamol – 200.00 mg,
acetylsalicylic acid – 200.00 mg,
anhydrous caffeine, calculated as dry matter – 40.00 mg;
excipients: potato starch – 45.60 mg, povidone K-17 (low molecular weight medical polyvinylpyrrolidone) – 2.40 mg, stearic acid – 2.50 mg, talc – 6.40 mg, calcium stearate – 1.10 mg, silicone emulsion CE 10-12 – 1.25 mg, vaseline oil – 0.75 mg.
Pregnancy
Pregnancy
The use of Askofen-P® is contraindicated during pregnancy and breastfeeding.
Contraindications
Contraindications
· Peptic ulcer of the stomach and duodenum in the acute phase;
· Gastrointestinal bleeding or perforation, history of peptic ulcer;
· Severe renal or liver failure;
· Hemorrhagic diathesis, hypocoagulation (including hemophilia, hypoprothrombinemia);
· Surgical interventions accompanied by heavy bleeding;
· Pregnancy, breastfeeding period;
· Glucose-6-phosphate dehydrogenase deficiency;
· Glaucoma;
· Hypersensitivity to the components of the drug;
· Complete and incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to ASA or other non-steroidal anti-inflammatory drugs (including a history);
· Children up to 15 years of age as an anesthetic, for febrile syndrome – up to 18 years of age;
· Increased excitability, sleep disturbances;
· Organic diseases of the cardiovascular system (including acute myocardial infarction, atherosclerosis);
· Severe arterial hypertension;
· Portal hypertension;
· Chronic heart failure of III-IV functional class according to NYHA;
· Concomitant use of methotrexate more than 15 mg per week;
· Vitamin deficiency K;
· Hypoproteinemia.
With caution
Gout, hyperuricemia, gastric and duodenal ulcers, chronic obstructive pulmonary disease, hay fever, nasal polyposis, drug allergies, concomitant use of methotrexate at a dose of less than 15 mg/week, concomitant therapy with anticoagulants, non-steroidal anti-inflammatory drugs, glucocorticosteroids, antiplatelet agents, selective inhibitors serotonin reuptake.
Mild to moderate renal failure, mild to moderate liver failure with increased transaminase levels, benign hyperbilirubinemia (including Gilbert’s syndrome, alcoholic liver damage), alcoholism, epilepsy and a tendency to seizures, old age, gout, arterial hypertension, chronic heart failure of functional class I-II according to NYHA, coronary heart disease, cerebrovascular diseases, peripheral arterial diseases, smoking.
If you have one of the listed diseases/conditions, be sure to consult your doctor before taking the drug.
Side Effects
Side Effects
The frequency of adverse drug reactions is classified according to the recommendations of the World Health Organization:
very common (≥ 1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), very rare (< 1/10,000), frequency unknown (frequency cannot be estimated from available data).
Infections and infestations:
rarely – pharyngitis.
Metabolic and nutritional disorders:
rarely – anorexia (decreased appetite).
Mental disorders:
often – nervousness;
infrequently – insomnia;
rarely – anxiety, euphoric mood, internal tension.
Nervous system disorders:
often – dizziness;
uncommon – tremor, paresthesia, headache;
rarely – taste disorder, attention disorder, amnesia, impaired coordination of movement, hyperesthesia, pain in the paranasal sinuses.
Blood disorders:
rarely – decreased platelet aggregation, hypocoagulation, hemorrhagic syndrome (nosebleeds, bleeding gums, purpura, etc.).
Immune system disorders:
frequency unknown – allergic reactions: skin rash, Quincke’s edema, bronchospasm, exudative erythema multiforme (including Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell’s syndrome), Reye’s syndrome in children (metabolic acidosis, nervous system and mental disorders, vomiting, liver dysfunction).
Visual disorders:
rarely – visual impairment.
Hearing disorders:
uncommon – tinnitus;
frequency unknown – deafness.
Cardiac disorders:
uncommon – tachycardia, arrhythmia.
Disorders of the respiratory system, chest and mediastinal organs:
rarely – nosebleeds, hypoventilation, rhinorrhea.
Digestive system disorders:
often – nausea, abdominal discomfort;
uncommon – dry mouth, vomiting, diarrhea, erosive and ulcerative lesions of the gastrointestinal tract;
rarely – belching, flatulence, dysphagia, paresthesia in the mouth, increased salivation;
frequency unknown – gastralgia, gastrointestinal bleeding.
Disorders of the liver and biliary tract:
uncommon – hepatotoxicity;
frequency unknown – liver failure.
Disorders of the skin and subcutaneous tissues:
rarely – hyperhidrosis, itching, urticaria.
Musculoskeletal and connective tissue disorders:
rarely – musculoskeletal stiffness, neck pain, back pain, muscle spasms.
Renal and urinary tract disorders:
uncommon – nephrotoxicity;
frequency unknown – renal failure, kidney damage with papillary necrosis.
General disorders and disorders at the injection site:
infrequently – fatigue, increased excitability;
rarely – asthenia, heaviness in the chest.
There is no data on an increase or expansion of the range of adverse effects of individual components when used as part of a combination in accordance with the instructions for medical use.
If you experience the side effects listed in the instructions, or they get worse, or you notice any other side effects not listed in the instructions, tell your doctor.
Interaction
Interaction
Acetylsalicylic acid
Other non-steroidal anti-inflammatory drugs: Increased damaging effect on the mucous membrane of the gastrointestinal tract (GIT), increasing the risk of developing gastrointestinal bleeding. If simultaneous use is necessary, it is recommended to use gastroprotectors for the prevention of NSAID-induced gastrointestinal ulcers, therefore simultaneous use is not recommended.
Glucocorticosteroids: Increased damaging effect on the gastrointestinal mucosa, increasing the risk of gastrointestinal bleeding. If simultaneous use is necessary, it is recommended to use gastroprotectors, especially in persons over 65 years of age, therefore simultaneous use is not recommended.
Oral anticoagulants (for example, coumarin derivatives): Acetylsalicylic acid (ASA) may potentiate the effect of anticoagulants. Clinical and laboratory monitoring of bleeding time and prothrombin time is necessary. Simultaneous use is not recommended.
Thrombolytics: Increased risk of bleeding. The use of ASA in patients within the first 24 hours after an acute stroke is not recommended. Simultaneous use is not recommended.
Heparin: Increased risk of bleeding. Clinical and laboratory monitoring of bleeding time is required. Simultaneous use is not recommended.
Platelet aggregation inhibitors (ticlopidine, paracetamol, clopidogrel, cilostazol): Increased risk of bleeding. Clinical and laboratory monitoring of bleeding time is required. Simultaneous use is not recommended.
Selective serotonin reuptake inhibitors (SSRIs): Concomitant use may affect blood clotting or platelet function, resulting in an increased risk of bleeding in general, and gastrointestinal bleeding in particular, and concomitant use is not recommended.
Phenytoin: ASA increases plasma concentrations of phenytoin, which requires monitoring.
Valproic acid: ASA interferes with plasma protein binding and may therefore increase its toxicity. Monitoring of plasma concentrations of valproic acid is necessary.
Aldosterone antagonists (spironolactone, canrenoate): ASA may reduce their activity due to impaired sodium excretion; proper blood pressure control is necessary.
Loop diuretics (eg, furosemide): ASA may reduce their activity due to impaired glomerular filtration due to inhibition of prostaglandin synthesis in the kidneys. Concomitant use of nonsteroidal anti-inflammatory drugs (NSAIDs) may lead to acute renal failure, especially in dehydrated patients. If diuretics are used concomitantly with ASA, ensure the patient is adequately rehydrated and monitor renal function and blood pressure, especially when diuretic treatment is initiated.
Antihypertensive drugs (ACE inhibitors, angiotensin II receptor antagonists, blockers of “slow” calcium channels): ASA can reduce their activity due to inhibition of prostaglandin synthesis in the kidneys.
Concomitant use may lead to acute renal failure in elderly or dehydrated patients. If diuretics are used concomitantly with ASA, it is necessary to ensure adequate rehydration of the patient and monitor renal function and blood pressure. When used concomitantly with verapamil, bleeding time should be monitored.
Uricosurics (eg, probenecid, sulfinpyrazone): ASA may reduce their activity by inhibiting tubular reabsorption, leading to high plasma concentrations of ASA.
Methotrexate ≤ 15 mg/week: ASA, like all NSAIDs, reduces the tubular secretion of methotrexate, increasing its plasma concentration and thus toxicity. In this regard, the simultaneous use of NSAIDs in patients receiving high doses of methotrexate is not recommended (see section “Contraindications”).
In patients taking low doses of methotrexate, the risk of interaction between methotrexate and NSAIDs should also be considered, especially if renal function is impaired. If combination therapy is necessary, it is necessary to monitor a general blood count, liver and kidney function, especially in the first days of treatment.
Sulfonylurea derivatives and insulin: ASA enhances their hypoglycemic effect, therefore, when taking a high dose of salicylates, a reduction in the dose of hypoglycemic drugs may be necessary. It is recommended to monitor blood glucose levels more often.
Alcohol: Increases the risk of gastrointestinal bleeding; concomitant use should be avoided.
Paracetamol
Inducers of liver microsomal enzymes or potentially hepatotoxic substances (for example, alcohol, rifampicin, isoniazid, hypnotics and antiepileptic drugs, including phenobarbital, phenytoin and carbamazepine): Increased toxicity of paracetamol, which can lead to liver damage even at non-toxic doses of paracetamol, so liver function should be monitored. Simultaneous use is not recommended.
Chloramphenicol: Paracetamol may increase the risk of increased chloramphenicol concentrations. Simultaneous use is not recommended.
Zidovudine: Paracetamol may increase the tendency to develop neutropenia, and therefore hematological parameters should be monitored. Simultaneous use is possible only with the permission of a doctor.
Probenecid: Probenecid reduces the clearance of paracetamol, which requires a reduction in the dose of paracetamol. Simultaneous use is not recommended.
Indirect anticoagulants: Repeated use of paracetamol for more than one week increases the anticoagulant effect. Occasional use of paracetamol has no significant effect.
Propantheline and other drugs that slow gastric emptying: Reduce the rate of absorption of paracetamol, which may delay or reduce rapid pain relief.
Metoclopramide and other drugs that accelerate gastric emptying: Increases the rate of absorption of paracetamol and, accordingly, the effectiveness and onset of analgesic action.
Cholestyramine: Reduces the rate of absorption of paracetamol, therefore, if maximum analgesia is needed, cholestyramine is taken no earlier than 1 hour after taking paracetamol.
Caffeine
Hypnotics (eg, benzodiazepines, barbiturates, H1-blockers): Concomitant use may reduce the hypnotic effect or reduce the anticonvulsant effect of barbiturates, so concomitant use is not recommended. If simultaneous use is necessary, it is advisable to take the combination in the morning.
Lithium: Caffeine withdrawal may increase plasma lithium concentrations because caffeine increases the renal clearance of lithium, so a lithium dose reduction may be necessary when caffeine is withdrawn. Simultaneous use is not recommended.
Disulfiram: Patients being treated with disulfiram should be warned to avoid caffeine to avoid the risk of worsening alcohol withdrawal syndrome due to the stimulating effects of caffeine on the cardiovascular and central nervous systems.
Ephedrine-like substances: Increased risk of developing drug dependence. Simultaneous use is not recommended.
Sympathomimetics or levothyroxine: Due to mutual potentiation, they can enhance the chronotropic effect. Simultaneous use is not recommended.
Theophylline: Concomitant use reduces the excretion of theophylline.
Antibacterial drugs from the quinolone group, enoxacin and pipemidic acid, terbinafine, cimetidine, fluvoxamine and oral contraceptives: Increased half-life of caffeine due to inhibition of liver cytochrome P450, so patients with impaired liver function, cardiac arrhythmias and latent epilepsy should avoid caffeine.
Nicotine, phenytoin and phenylpropanolamine: Reduce the terminal half-life of caffeine.
Clozapine: Caffeine increases clozapine serum concentrations, likely through both pharmacokinetic and pharmacodynamic mechanisms. Monitoring of serum concentrations of clozapine is necessary. Simultaneous use is not recommended.
Overdose
Overdose
Acetylsalicylic acid
For mild intoxications – dizziness, tinnitus, deafness, increased sweating, nausea, vomiting, headache and confusion. Occurs at plasma concentrations of 150-300 mcg/ml. Treatment is dose reduction or discontinuation of therapy.
At concentrations above 300 mcg/ml, more severe intoxication occurs, manifested by hyperventilation, fever, anxiety, ketoacidosis, respiratory alkalosis and metabolic acidosis. Central nervous system depression can lead to coma, and cardiovascular collapse and respiratory failure may also occur.
The greatest risk of developing chronic intoxication is observed in children and the elderly when taking more than 100 mg/kg/day for several days.
Treatment
If there is a suspicion that more than 120 mg/kg of salicylates has been ingested, activated charcoal is administered orally several times during the last hour.
When taking more than 120 mg/kg of salicylates, their plasma concentration should be determined, although it is impossible to predict its severity based on this indicator alone; clinical and biochemical parameters must also be taken into account.
If plasma concentrations exceed 500 mcg/mL (350 mcg/mL for children <5 years), intravenous sodium bicarbonate is effective in removing salicylates from plasma. If plasma concentrations exceed 700 mcg/mL (lower concentrations in children and the elderly) or in severe metabolic acidosis, hemodialysis or hemoperfusion is the treatment of choice.
Paracetamol overdose
In case of overdose, intoxication is possible, especially in elderly patients, children, patients with liver diseases (caused by chronic alcoholism), in patients with nutritional disorders, as well as in patients taking inducers of microsomal liver enzymes, in which fulminant hepatitis, liver failure, cholestatic hepatitis, cytolytic hepatitis can develop, in the above cases – sometimes with a fatal outcome.
The clinical picture of acute overdose develops within 24 hours after taking paracetamol.
Symptoms: gastrointestinal disorders (nausea, vomiting, loss of appetite, abdominal discomfort and (or) abdominal pain), pale skin. When simultaneous administration of 7.5 g or more to adults or more than 140 mg/kg to children, cytolysis of hepatocytes occurs with complete and irreversible liver necrosis, the development of liver failure, metabolic acidosis and encephalopathy, which can lead to coma and death.
12-48 hours after the administration of paracetamol, there is an increase in the activity of microsomal liver enzymes, lactate dehydrogenase, bilirubin concentration and a decrease in prothrombin content. Clinical symptoms of liver damage appear 2 days after an overdose of the drug and reach a maximum on days 4-6.
Treatment
Immediate hospitalization.
Determination of the quantitative content of paracetamol in blood plasma before starting treatment as early as possible after an overdose; The introduction of SH-group donors and precursors for glutathione synthesis – methionine and acetylcysteine - is most effective in the first 8 hours.
The need for additional therapeutic measures (further administration of methionine, intravenous administration of acetylcysteine) is determined depending on the concentration of paracetamol in the blood, as well as the time elapsed after its administration.
Symptomatic treatment.
Laboratory studies of the activity of microsomal liver enzymes should be performed at the beginning of treatment and then every 24 hours.
In most cases, the activity of microsomal liver enzymes returns to normal within 1-2 weeks. In very severe cases, a liver transplant may be required.
Caffeine
Common symptoms include gastralgia, agitation, delirium, anxiety, nervousness, restlessness, insomnia, mental agitation, muscle twitching, confusion, convulsions, dehydration, frequent urination, pyrexia, headache, increased sensitivity to touch or pain, nausea and vomiting (sometimes with blood), tinnitus.
In case of severe overdose, hyperglycemia may occur. Cardiac disorders are manifested by tachycardia and arrhythmia.
Treatment is to reduce the dose or stop caffeine.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 °C
Shelf life
Shelf life
3 years. Do not use after expiration date
expiration date indicated on the packaging.
Manufacturer
Manufacturer
Pharmstandard-Leksredstva, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date printed on the package. |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C |
| Manufacturer | Pharmstandard-Leksredstva, Russia |
| Medication form | pills |
| Brand | Pharmstandard-Leksredstva |
Other forms…
Related products
Buy Ascophen-P, tablets 10 pcs with delivery to USA, UK, Europe and over 120 other countries.