No products in the cart.
Amitriptyline, tablets 25 mg 50 pcs
€3696.00 €3.08
Out of stock
(E-mail when Stock is available)
Description
Enuresis, Migraine, Anxiety, Pain, Depression, Depressed mood
Depression (especially with anxiety, agitation and sleep disorders, including in childhood, endogenous, involutional, reactive, neurotic, drug-induced, with organic brain lesions).
. As a part of complex therapy it is used for mixed emotional disorders, psychosis in schizophrenia, alcohol withdrawal, behavior disorders (activity and attention), nocturnal enuresis in children (except for patients with bladder hypotension), bulimia nervosa, chronic pain syndrome (chronic pain in cancer patients, migraine, rheumatic diseases, atypical pain in the face, postherpetic neuralgia, posttraumatic neuropathy, diabetic or others. peripheral neuropathy), headache, migraine (prevention), gastric and 12 duodenal ulcer.
Indications
Indications
Depression (especially with anxiety, agitation and sleep disorders, including in childhood, endogenous, involutional, reactive, neurotic, drug-induced, with organic brain damage).
As part of complex therapy, it is used for mixed emotional disorders, psychosis in schizophrenia, alcohol withdrawal, behavioral disorders (activity and attention), nocturnal enuresis in children (except for patients with bladder hypotension), bulimia nervosa, chronic pain syndrome (chronic pain in cancer patients, migraine, rheumatic diseases, atypical pain in the face, postherpetic neuralgia, posttraumatic neuropathy, diabetic or other peripheral neuropathy), headaches, migraines (prevention), gastric and duodenal ulcers.
Pharmacological effect
Pharmacological effect
Antidepressant
Special instructions
Special instructions
Before starting treatment, blood pressure monitoring is necessary (in patients with low or labile blood pressure, it may decrease even more); during the treatment period – control of peripheral blood (in some cases, agranulocytosis may develop, and therefore it is recommended to monitor the blood picture, especially with an increase in body temperature, development of flu-like symptoms and sore throat), during long-term therapy – control of the functions of the cardiovascular system and liver. In the elderly and patients with cardiovascular diseases, monitoring of heart rate (HR), blood pressure, and ECG is indicated. Clinically insignificant changes may appear on the ECG (smoothing of the T wave, depression of the S-T segment, widening of the QRS complex).
Caution is required when suddenly moving to a vertical position from a lying or sitting position.
During the treatment period, the use of ethanol should be avoided.
Prescribed no earlier than 14 days after discontinuation of MAO inhibitors, starting with small doses.
If you suddenly stop taking it after long-term treatment, withdrawal syndrome may develop.
Amitriptyline in doses above 150 mg/day reduces the threshold of convulsive activity (the risk of epileptic seizures in predisposed patients should be taken into account, as well as in the presence of other factors predisposing to the occurrence of convulsive syndrome, for example, brain damage of any etiology, simultaneous use of antipsychotic drugs (neuroleptics), during the period of refusal of ethanol or withdrawal of drugs with anticonvulsant properties, for example benzodiazepines).
Severe depression is characterized by a risk of suicidal actions, which can persist until significant remission is achieved. In this regard, at the beginning of treatment, a combination with drugs from the group of benzodiazepines or neuroleptic drugs and constant medical supervision (entrusting the storage and dispensing of drugs to trusted persons) may be indicated.
In children, adolescents and young adults (under 24 years of age) with depression and other mental disorders, antidepressants, compared with placebo, increase the risk of suicidal thoughts and behavior. Therefore, when prescribing amitriptyline or any other antidepressants in this category of patients, the risk of suicide should be weighed against the benefits of their use. In short-term studies, the risk of suicide did not increase in people over 24 years of age, but it decreased slightly in people over 65 years of age. During treatment with antidepressants, all patients should be monitored for early detection of suicidal tendencies.
In patients with cyclic affective disorders during the depressive phase, manic or hypomanic states may develop during therapy (reducing the dose or discontinuing the drug and prescribing an antipsychotic drug are necessary). After relief of these conditions, if indicated, treatment in low doses can be resumed.
Due to possible cardiotoxic effects, caution is required when treating patients with thyrotoxicosis or patients receiving thyroid hormone preparations.
In combination with electroconvulsive therapy, it is prescribed only under the condition of careful medical supervision.
In predisposed patients and elderly patients, it can provoke the development of drug-induced psychoses, mainly at night (after discontinuation of the drug, they disappear within a few days).
May cause paralytic ileus, primarily in patients with chronic constipation, the elderly, or those forced to bed rest.
Before performing general or local anesthesia, the anesthesiologist should be warned that the patient is taking amitriptyline.
Due to the anticholinergic effect, there may be a decrease in tear production and a relative increase in the amount of mucus in the tear fluid, which can lead to damage to the corneal epithelium in patients using contact lenses.
With long-term use, an increase in the incidence of dental caries is observed. The need for riboflavin may be increased.
Animal reproduction studies have shown adverse effects on the fetus, and there are no adequate and well-controlled studies in pregnant women. In pregnant women, the drug should be used only if the expected benefit to the mother outweighs the potential risk to the fetus.
Passes into breast milk and may cause drowsiness in nursing infants.
To avoid the development of withdrawal syndrome in newborns (manifested by shortness of breath, drowsiness, intestinal colic, increased nervous excitability, increased or decreased blood pressure, tremors or spastic phenomena), amitriptyline is gradually discontinued at least 7 weeks before the expected birth.
Children are more sensitive to acute overdose, which should be considered dangerous and potentially fatal to them.
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Amitriptyline
Composition
Composition
1 tab. amitriptyline hydrochloride 28.3 mg, which corresponds to the content of amitriptyline 25 mg
Excipients: lactose monohydrate, corn starch, gelatin, calcium stearate, talc, colloidal silicon dioxide.
Shell composition: simethicone SE-2, macrogol, Sepifilm 3048 Yellow (hypromellose, microcrystalline cellulose, polyoxyl 40 stearate, titanium dioxide, quinoline yellow dye (E104).
Contraindications
Contraindications
Hypersensitivity,
use together with MAO inhibitors and 2 weeks before starting treatment,
myocardial infarction (acute and subacute periods),
acute alcohol intoxication,
acute intoxication with hypnotic, analgesic and psychoactive drugs,
angle-closure glaucoma,
severe disturbances of AV and intraventricular conduction (bundle branch block, AV block II degree),
lactation period,
children under 6 years of age.
Due to the content of lactose monohydrate (milk sugar), the drug should not be taken by patients with rare hereditary diseases such as galactose intolerance, lactase deficiency or glucose-galactose malabsorption.
With caution
Amitriptyline should be used with caution in persons with alcoholism, bronchial asthma, schizophrenia (possible activation of psychosis), bipolar disorder, epilepsy, suppression of bone marrow hematopoiesis, diseases of the cardiovascular system (CVS) (angina pectoris, arrhythmia, heart block, chronic heart failure, myocardial infarction, arterial hypertension), intraocular hypertension, stroke, decreased motor function of the gastrointestinal tract (GIT) (risk of paralytic ileus), liver and/or renal failure, thyrotoxicosis, prostatic hyperplasia, urinary retention, hypotension of the bladder, during pregnancy (especially the first trimester), in old age.
Side Effects
Side Effects
Mainly associated with the anticholinergic effect of the drug: accommodation paresis. Blurred vision, increased intraocular pressure, dry mouth, constipation, intestinal obstruction, urinary retention, increased body temperature. All these phenomena usually disappear after adaptation to the drug or dose reduction.
From the central nervous system: headache, ataxia, increased fatigue, weakness, irritability, dizziness, tinnitus, drowsiness or insomnia, impaired concentration, nightmares, dysarthria, confusion, hallucinations, motor agitation, disorientation, tremor, paresthesia, peripheral neuropathy, changes in the EEG. Rarely, extrapyramidal disorders, seizures, anxiety.
From the cardiovascular system: tachycardia, arrhythmia, conduction disturbances, blood pressure lability, widening of the QRS complex on the ECG (intraventricular conduction disturbance), symptoms of heart failure, fainting.
From the gastrointestinal tract: nausea, vomiting, heartburn, anorexia, stomatitis, taste disturbances, darkening of the tongue, feeling of discomfort in the epigastrium, gastralgia, increased activity of “liver” transaminases, rarely cholestatic jaundice, diarrhea.
From the endocrine system: an increase in the size of the mammary glands in men and women, galactorrhea, changes in the secretion of antidiuretic hormone (ADH), changes in libido, potency. Rarely: hypo- or hyperglycemia, glucosuria, impaired glucose tolerance, testicular swelling. Allergic reactions: skin rash, itching, photosensitivity, angioedema, urticaria.
Other: agranulocytosis, leukopenia, eosinophilia, thrombocytopenia, purpura and other blood changes, hair loss, swollen lymph nodes, weight gain with long-term use, sweating, pollakiuria. With long-term treatment, especially in high doses, with abrupt cessation of treatment, withdrawal syndrome may develop: headache, nausea, vomiting, diarrhea, as well as irritability, sleep disturbance with vivid, unusual dreams, increased excitability.
Interaction
Interaction
With the combined use of ethanol and drugs that depress the central nervous system (including other antidepressants, barbiturates, benzadiazepines and general anesthetics), a significant increase in the inhibitory effect on the central nervous system, respiratory depression and hypotensive effect is possible.
Increases sensitivity to drinks containing ethanol.
Increases the anticholinergic effect of drugs with anticholinergic activity (for example, phenothiazine derivatives, antiparkinsonian drugs, amantadine, atropine, biperiden, antihistamine drugs), which increases the risk of side effects (from the central nervous system, vision, intestines and bladder). When used together with anticholinergic blockers, phenothiazine derivatives and benzodiazepines, there is a mutual enhancement of the sedative and central anticholinergic effects and an increased risk of epileptic seizures (lowering the threshold of convulsive activity); Phenothiazine derivatives may also increase the risk of neuroleptic malignant syndrome.
When used together with anticonvulsants, it is possible to enhance the inhibitory effect on the central nervous system, reduce the threshold of convulsive activity (when used in high doses) and reduce the effectiveness of the latter.
When used together with antihistamines, clonidine – increased inhibitory effect on the central nervous system; with atropine – increases the risk of paralytic intestinal obstruction; with drugs that cause extrapyramidal reactions – an increase in the severity and frequency of extrapyramidal effects.
With the simultaneous use of amitriptyline and indirect anticoagulants (coumarin or indadione derivatives), the anticoagulant activity of the latter may increase.
Amitriptyline may enhance depression caused by glucocorticosteroids (GCS).
Drugs for the treatment of thyrotoxicosis increase the risk of developing agranulocytosis.
Reduces the effectiveness of phenytoin and alpha-blockers.
Inhibitors of microsomal oxidation (cimetidine) prolong T1/2, increase the risk of developing toxic effects of amitriptyline (a dose reduction of 20-30% may be required); inducers of microsomal liver enzymes (barbiturates, carbamazepine, phenytoin, nicotine and oral contraceptives) reduce plasma concentrations and reduce the effectiveness of amitriptyline.
Combined use with disulfiram and other acetaldehydrogenase inhibitors provokes delirium.
Fluoxetine and fluvoxamine increase plasma concentrations of amitriptyline (a 50% reduction in amitriptyline dose may be required).
Estrogen-containing oral contraceptives and estrogens may increase the bioavailability of amitriptyline.
With the simultaneous use of amitriptyline with clonidine, guanethidine, betanidine, reserpine and methyldopa – a decrease in the hypotensive effect of the latter; with cocaine – the risk of developing cardiac arrhythmias.
Antiarrhythmic drugs (such as quinidine) increase the risk of developing rhythm disturbances (possibly slowing down the metabolism of amitriptyline).
Pimozide and probucol may increase cardiac arrhythmias, which is manifested by prolongation of the QT interval on the ECG.
It enhances the effect of epinephrine, norepinephrine, isoprenaline, ephedrine and phenylephrine on the cardiovascular system (including when these drugs are part of local anesthetics) and increases the risk of developing heart rhythm disturbances, tachycardia, and severe arterial hypertension.
When co-administered with alpha-adrenergic agonists for intranasal administration or for use in ophthalmology (with significant systemic absorption), the vasoconstrictor effect of the latter may be enhanced.
When taken together with thyroid hormones, there is a mutual enhancement of the therapeutic effect and toxic effects (including cardiac arrhythmias and a stimulating effect on the central nervous system).
M-anticholinergic drugs and antipsychotic drugs (neuroleptics) increase the risk of developing hyperpyrexia (especially in hot weather).
When co-administered with other hematotoxic drugs, increased hematotoxicity is possible.
Incompatible with MAO inhibitors (increased frequency of periods of hyperpyrexia, severe convulsions, hypertensive crises and patient death are possible).
Overdose
Overdose
Symptoms: drowsiness, disorientation, confusion, dilated pupils, increased body temperature, shortness of breath, dysarthria, agitation, hallucinations, seizures, muscle rigidity, suppuration, coma, vomiting, arrhythmia, arterial hypotension, heart failure, respiratory depression.
Treatment: discontinuation of amitriptyline therapy, gastric lavage, fluid infusion, symptomatic therapy, maintenance of blood pressure and water-electrolyte balance. Monitoring of cardiovascular activity (ECG) is indicated for 5 days, because relapse may occur within 48 hours or later. Hemodialysis and forced diuresis are not very effective.
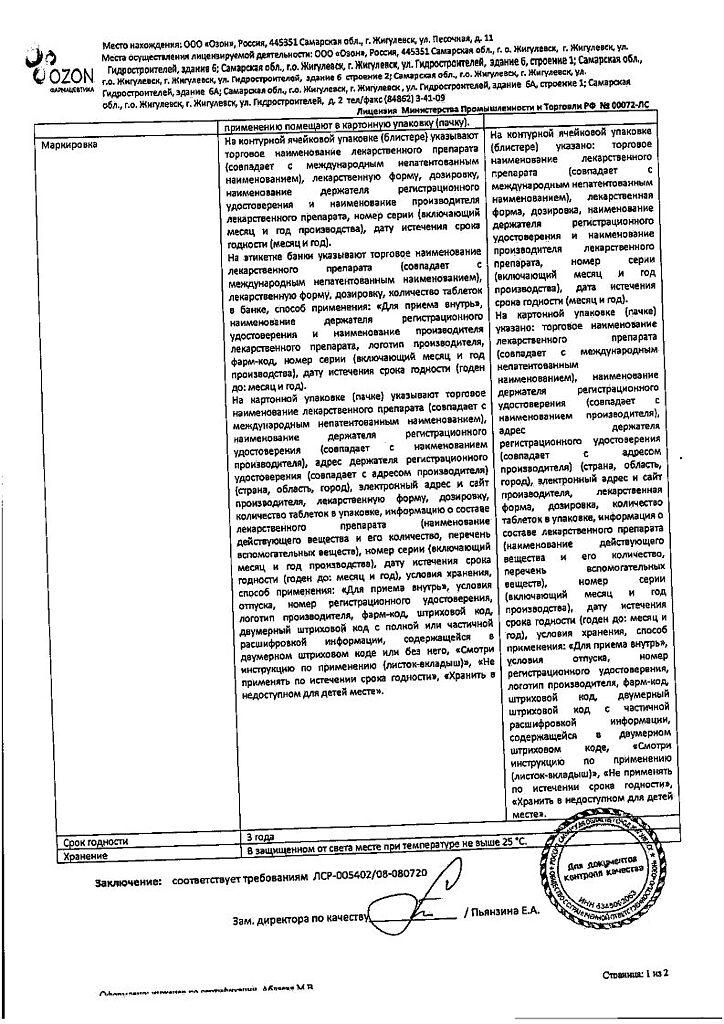
Storage conditions
Storage conditions
In a dry place, protected from light, out of reach of children, at a temperature of 15 to 25 ° C.
Shelf life
Shelf life
3 years.
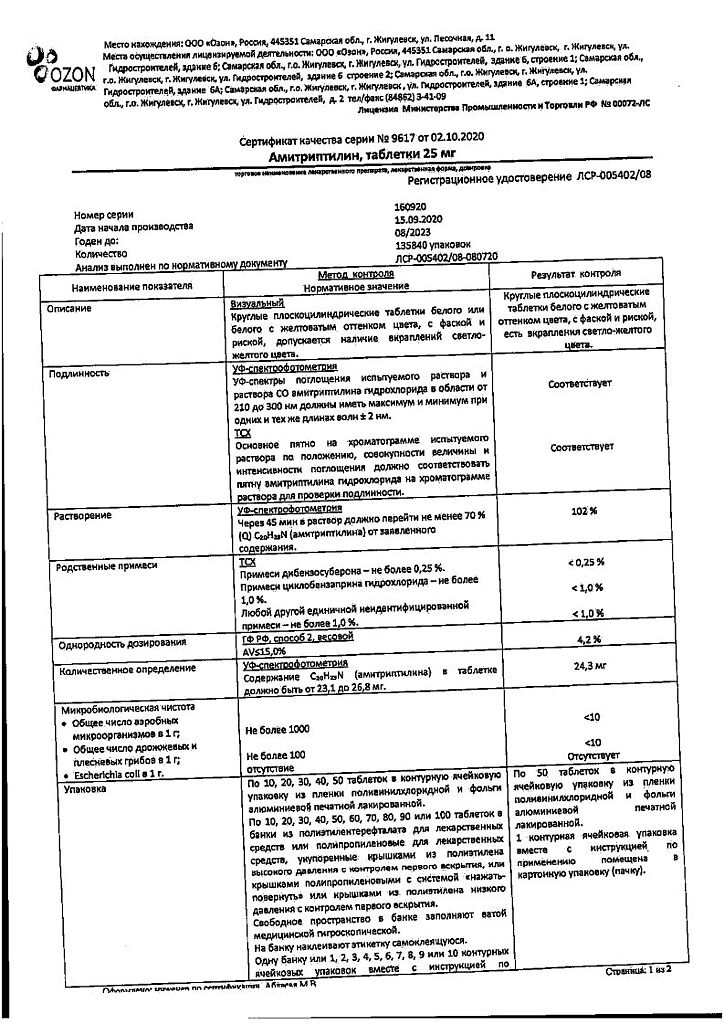
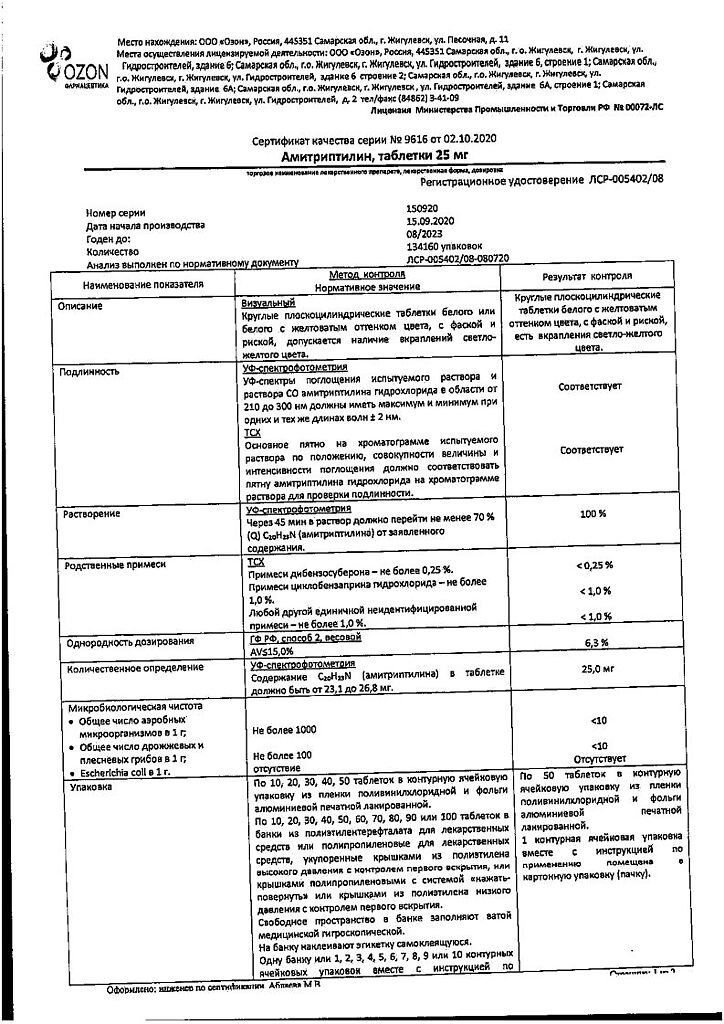
Manufacturer
Manufacturer
Ozon, Russia
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | In a dry, protected from light, out of the reach of children, at a temperature of 15 to 25oC. |
| Manufacturer | Ozon, Russia |
| Medication form | pills |
| Brand | Ozon |
Related products
Buy Amitriptyline, tablets 25 mg 50 pcs with delivery to USA, UK, Europe and over 120 other countries.