No products in the cart.
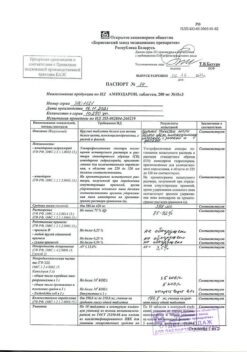
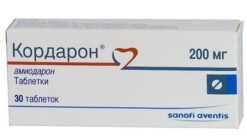
Amiodarone, tablets 200 mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Amiodarone has antiarrhythmic, coronary vasodilator and antianginal effects.
Amiodarone is the active ingredient, which is able to facilitate heart function without significantly changing cardiac output and myocardial contractility.
At the same time, the drug increases coronary blood flow by decreasing resistance in the arteries of the heart and decreases HR and BP due to a peripheral vasodilator effect.
This significantly decreases myocardial oxygen consumption and at the same time increases myocardial energy reserves by increasing creatine phosphate iglycogen.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
1 tablet contains:
The active ingredient:
amiodarone hydrochloride 0.2 g.
Auxiliary substances:
Milk sugar,
Polyvinylpyrrolidone medium molecular weight,
potato starch,
talc,
calcium stearate,
cellulose.
How to take, the dosage
How to take, the dosage
To be taken by mouth with or after a meal.
The whole tablet is taken with a small amount of liquid.
The dose of the drug should be adjusted according to the patient’s condition and determined by the physician.
The starting dose is 600-800 mg (up to 1200 mg) per day divided into 2-3 doses.
The course of treatment is 8-15 days.
If necessary, the dose can be increased to 1200 mg of amiodarone daily.
After signs of saturation are reached, maintenance therapy is switched to.
In maintenance treatment, the lowest effective dose is used, depending on the individual response of the patient, and is usually 100 to 400 mg daily in 1 to 2 doses.
Whenever possible, a two-day break is taken every 5 days.
In adults the average therapeutic single dose is 0.2 g, the average therapeutic daily dose is 0.4 g, the maximum single dose is 0.4 g, the maximum daily dose is 1.2 g.
Interaction
Interaction
The drug should not be used concomitantly with other antiarrhythmic agents, beta-adrenoblockers, some “slow” calcium channel blockers ( verapamil), MAO inhibitors, pentamine (intravenous), because this may lead to the development of polymorphic ventricular tachycardia (torsade de pointe).
Combination with phenothiazine derivatives, terfenadine and astemizole may cause ventricular arrhythmias.
It potentiates the effect of oral anticoagulants, nitrates, foxglove drugs, phenytoin and cyclosporine (the dose of the latter must be corrected).
Colestyramine decreases absorption, half-life and plasma concentration of amiodarone.
The concomitant administration of the drug and potassium-eluting diuretics, glucocorticosteroids, or amphotericin B (intravenous) may, due to the development of hypokalemia, cause additional prolongation of the QT interval, which increases the risk of ventricular arrhythmias.
The concomitant administration of amiodarone and cimetidine leads to slower metabolism of amiodarone, which causes increased serum concentrations.
Amiodarone may affect thyroid function tests, especially thyroxine and thyrotropic hormone (TSH) levels.
The cardiac glycosides increase the risk of bradycardia and atrioventricular conduction depression.
Photosensitizing drugs have additive photosensitizing effects.
Special Instructions
Special Instructions
Before starting therapy, a radiological examination of the lungs should be performed, and thyroid function (hormone content) and liver function (transaminases) should be evaluated.
The frequency and severity of adverse events depend on the dose of the drug, so minimal effective maintenance doses should be used.
Caution should be exercised when treating elderly patients because bradycardia may occur. The QT interval may be prolonged with the occurrence of the U wave.
The treatment should be discontinued if sinoauricular block, second- or third-degree atrioventricular node block, and Gis bundle vein block occur.
At the time of treatment, it is recommended that electrocardiographic monitoring be performed regularly (every 3 months), and also if there are new arrhythmias or signs of exacerbation of the underlying disease.
Progressive dyspnea and non-productive cough may be signs of lung damage.
A chest radiograph and pulmonary function tests are recommended (every 6 months and if clinical signs of lung disease develop).
Plasma electrolytes should be determined before starting therapy.
Liver enzyme activity is regularly monitored during treatment with amiodarone.
When therapy is begun, ECG (QRS complex width and QT interval length), transaminases (if they tripled or doubled in case of initially elevated activity, the dose is decreased until discontinuation of therapy) are performed periodically.
Periodic observation by an ophthalmologist is necessary (detection of significant corneal deposits or development of visual disturbances requires withdrawal of amiodarone).
When withdrawn, recurrence of rhythm disturbances is possible.
Pregnancy and lactation use is possible only in life-threatening rhythm disturbances with ineffectiveness of other antiarrhythmic therapy (causes fetal thyroid dysfunction).
After withdrawal, the pharmacodynamic effect persists for 10-30 days.
Amiodarone may cause thyroid dysfunction, so it is recommended that thyroid function be monitored before starting treatment, during treatment, and for several months after discontinuation.
Contains iodine (at 200 mg-75 mg iodine), so may affect the results of radioactive iodine accumulation tests in the thyroid gland.
When performing surgical interventions, make the anesthesiologist aware of taking the drug (possibility of acute respiratory distress syndrome in adults immediately after surgery).
Patients receiving this medication should avoid sun exposure because of the risk of photodermatosis.
Patients should use caution when using the drug during general anesthesia; there may be a risk of bradycardia, marked decrease in blood pressure, abnormal conduction, and decreased stroke volume.
Perhaps caution should be exercised during oxygen therapy in the postoperative period because of the risk of respiratory distress syndrome.
Pediatric use
The efficacy and safety of amiodarone in children have not been established.
Impact on ability to drive/operate machinery
In some patients, the drug may slow down psychomotor reactions, which should be taken into account when driving and operating machinery.
Contraindications
Contraindications
Side effects
Side effects
Cardiovascular system disorders: frequent – moderate bradycardia (dose-dependent); infrequent – sinoatrial blockade, AV blockade of various degrees, proarrhythmogenic effect (aggravation of existing arrhythmia or the emergence of new, including with cardiac arrest); very rare – severe bradycardia, sinus node arrest (in patients with sinus node dysfunction and older patients); frequency unknown – with long-term use – progression of chronic heart failure symptoms.
Digestive system disorders: very common – nausea, vomiting, decreased appetite, impaired taste, feeling of heaviness in the epigastrium, increased activity of “liver” transaminases (1.5-3 times higher than normal; often – acute toxic hepatitis with increased activity of “liver” transaminases and/or jaundice, including development of liver failure, including fatal; very rarely – chronic liver failure (pseudoalcoholic hepatitis, cirrhosis) including fatal.
Respiratory system disorders: frequent – alveolar or interstitial pneumonitis, obliterating bronchiolitis with pneumonia, including fatal, pleurisy, pulmonary fibrosis; very rare – bronchospasm in patients with severe respiratory failure (especially in patients with bronchial asthma), acute respiratory syndrome, including fatal; frequency unknown – pulmonary bleeding
Senses: very often – deposition of lipofuscin in the corneal epithelium (often there are no subjective complaints, but if the deposits are significant and partially fill the pupil, there may be complaints about the appearance of colored halos or blurred contours); very rarely – optic neuritis / optic neuropathy.
Endocrine system disorders: often – increase of T4 level with normal or insignificant decrease of T3 (if there are no clinical signs of thyroid dysfunction the treatment should not be discontinued). With long-term use hypothyroidism may occur, rarely hyperthyroidism (discontinuation of the drug is necessary); very rarely – ADH secretion disorder syndrome.
Dermatological reactions: very often – photosensitization; often – lead blue or bluish pigmentation of the skin (with long-term use); it slowly disappears within 10-14 days after discontinuing treatment; very rarely – erythema (with simultaneous radiation therapy), skin rash, exfoliative dermatitis (no association with taking the drug), vasculitis, alopecia.
Nervous system disorders: often – tremor and other extrapyramidal disorders, sleep disorders, including “nightmares” dreams; rarely – peripheral neuropathy (sensory, motor, mixed) and/or myopathy; very rarely – cerebellar ataxia, benign intracranial hypertension (brain pseudotumor), headache.
Laboratory indices: very rarely with long-term use – thrombocytopenia, hemolytic and aplastic anemia.
Others: very rare – epididymitis, decreased potency (relationship with taking the drug has not been established), vasculitis.
Overdose
Overdose
In case of signs of overdose, it is usually sufficient to reduce the dose of the drug or temporarily stop taking it.
If large amounts of the drug are taken at the same time, decreased blood pressure, bradycardia, arrhythmias, liver dysfunction, and atrioventricular block may occur.
Treatment: gastric lavage and administration of activated charcoal if the drug was taken recently. In other cases, symptomatic measures. There is no specific antidote, hemodialysis is ineffective. If bradycardia develops, atropine, beta 1-adrenomimetics may be prescribed, in severe cases – cardiostimulation.
Similarities
Similarities
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a place protected from light, at a temperature not exceeding 25°C. |
| Manufacturer | Organika, Russia |
| Medication form | pills |
| Brand | Organika |
Other forms…
Related products
Buy Amiodarone, tablets 200 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.