No products in the cart.
Amiodarone, 50 mg/ml concentrate 3 ml 10 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Myocardial infarction, Heart failure, Arrhythmia, Rapid heartbeat
Treatment with this medicine should be started in a hospital and under the supervision of a specialist. The drug is intended only for the treatment of severe rhythm disturbances which do not respond to other treatments, or when other treatments cannot be used.
Tachyarrhythmias associated with Wolff-Parkinson-White syndrome.
Tachyarrhythmias of all types, including supraventricular, nodal and ventricular tachycardia; atrial flutter and fibrillation, ventricular fibrillation; when other medications cannot be used.
The drug may be used when a rapid response to treatment is required or when oral administration is not possible.
Indications
Indications
Treatment with the drug should begin in a hospital setting and under the supervision of a specialist. The medicine is intended only for the treatment of severe rhythm disturbances that do not respond to other treatments, or when other treatments cannot be used.
Tachyarrhythmias associated with Wolff-Parkinson-White syndrome.
Tachyarrhythmias of all types, including supraventricular, nodal and ventricular tachycardia; atrial flutter and fibrillation, ventricular fibrillation; in cases where other drugs cannot be used.
The drug can be used when a rapid response to treatment is required or when oral administration is not possible.
Pharmacological effect
Pharmacological effect
Antianginal, antiarrhythmic.
Special instructions
Special instructions
– Electrolyte disturbances, especially hypokalemia: it is important to take into account situations that may be accompanied by hypokalemia as predisposing to proarrhythmic phenomena. Hypokalemia should be corrected before starting amiodarone
– Except in cases of emergency therapy, Amiodarone in the form of a solution for intravenous injection can only be used in a hospital and with constant monitoring (ECG, blood pressure).
Use with caution in chronic heart failure, liver failure, bronchial asthma, and in old age.
Active ingredient
Active ingredient
Amiodarone
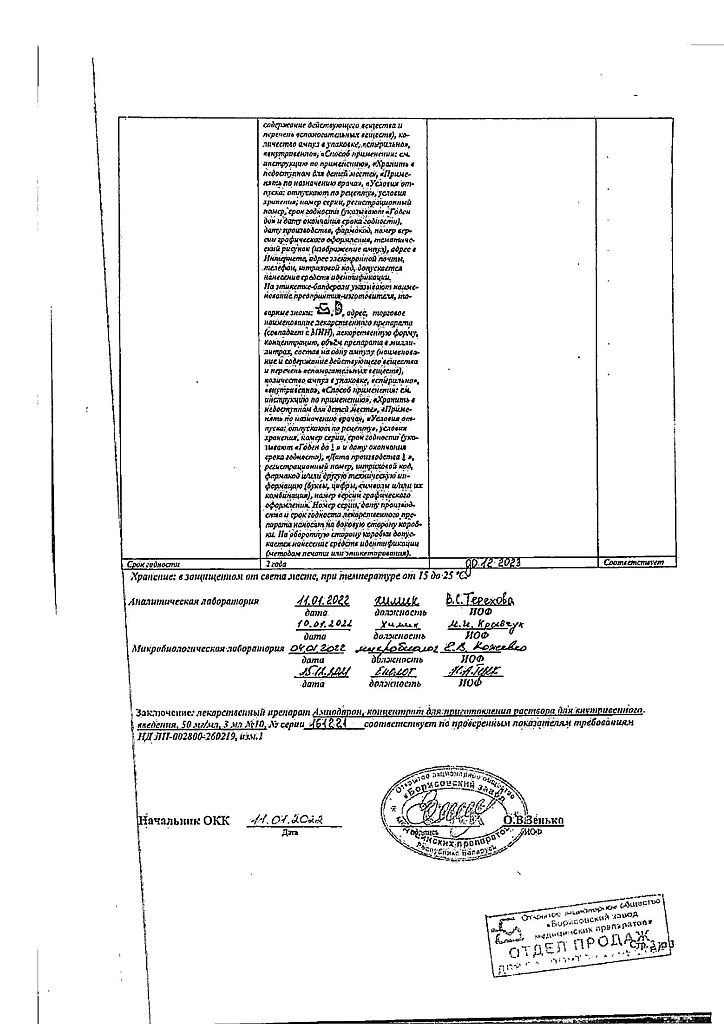
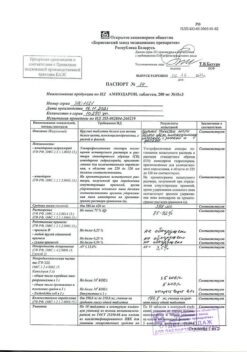
Composition
Composition
1 ampoule (3 ml solution) contains:
Contraindications
Contraindications
– sick sinus syndrome (SSNS), sinus bradycardia, sinoatrial block, except in cases of correction with an artificial pacemaker;
– atrioventricular block of II and III degrees, intraventricular conduction disorders (blockade of two and three branches of the His bundle); in these cases, the drug can be used in specialized departments under the guise of an artificial pacemaker (pacemaker);
– cardiogenic shock, collapse;
– severe arterial hypotension;
– simultaneous use with drugs that can cause polymorphic ventricular tachycardia of the “pirouette” type;
– thyroid dysfunction (hypothyroidism, hyperthyroidism);
– hypokalemia;
– pregnancy;
– breastfeeding;
– hypersensitivity to iodine and/or amiodarone;
– severe pulmonary dysfunction (interstitial lung disease);
– cardiomyopathy or decompensated heart failure (the patient’s condition may worsen).
Due to the presence of benzyl alcohol, Amiodarone is contraindicated in newborns, infants and children under 3 years of age.
Side Effects
Side Effects
From the cardiovascular system: often – bradycardia (usually a moderate decrease in heart rate); decrease in blood pressure, usually moderate and transient. Cases of severe arterial hypotension or collapse have been observed with overdose or too rapid administration of the drug. Very rarely – proarrhythmogenic effect (there are reports of the occurrence of new arrhythmias, including polymorphic ventricular tachycardia of the “pirouette” type, or aggravation of existing ones – in some cases with subsequent cardiac arrest). These effects are observed mainly when the drug is used in conjunction with drugs that prolong the period of repolarization of the ventricles of the heart (QTc interval) or in cases of electrolyte imbalance (see “Interaction”). In light of the available data, it is impossible to determine whether the occurrence of these arrhythmias is caused by amiodarone, or is related to the severity of the cardiac pathology, or is a consequence of treatment failure. Severe bradycardia or, in exceptional cases, sinus node arrest, which were observed in some patients (patients with sinus node dysfunction and elderly patients), flushing of the facial skin, progression of heart failure (possibly with intravenous jet administration).
From the respiratory system: very rarely – cough, shortness of breath, interstitial pneumonitis; bronchospasm and/or apnea in patients with severe respiratory failure, especially in patients with bronchial asthma; acute respiratory distress syndrome, sometimes fatal and sometimes immediately after surgery (potential for interaction with high concentrations of oxygen) (see “Special Instructions”).
From the digestive system: very often – nausea. Very rarely – an isolated increase in the activity of hepatic transaminases in the blood serum, usually moderate (1.5-3 times higher than normal values) and decreasing with decreasing dose or even spontaneously. Acute liver damage (within 24 hours after administration of amiodarone) with increased transaminases and/or jaundice, including the development of liver failure, sometimes fatal (see “Special Instructions”).
From the skin: very rarely – feeling of heat, increased sweating.
From the side of the central nervous system: very rarely – benign intracranial hypertension (pseudotumor cerebri), headache.
Immune system disorders: very rarely – anaphylactic shock. Unknown frequency – angioedema.
Reactions at the injection site: often – inflammatory reactions, such as superficial phlebitis, when administered directly into a peripheral vein. Reactions at the injection site, such as: pain, erythema, swelling, necrosis, extravasation, infiltration, inflammation, induration, thrombophlebitis, phlebitis, cellulitis, infection, pigmentation.
Method of preparation or use:
Amiodarone (injection form) is intended for use in cases where rapid achievement of an antiarrhythmic effect is required or oral administration of the drug is impossible.
With the exception of emergency clinical situations, the drug should be used only in a hospital in an intensive care unit under constant monitoring of ECG and blood pressure.
When administered intravenously, the drug should not be mixed with other drugs or simultaneously administered other drugs through the same venous access.
Use only in diluted form. For dilution, only 5% dextrose (glucose) solution should be used. Due to the characteristics of the dosage form of the drug, it is not recommended to use concentrations of the infusion solution that are less than those obtained with a dilution of 2 amps. in 500 ml 5% dextrose (glucose).
To avoid injection site reactions, amiodarone should be administered through a central venous catheter, except in cases of cardiac resuscitation for ventricular fibrillation refractory to cardioversion, when (in the absence of central venous access) peripheral veins (the largest peripheral vein with maximum blood flow) can be used to administer the drug.
Severe cardiac arrhythmias in cases where oral administration of the drug is not possible (except in cases of cardiac resuscitation for cardiac arrest caused by ventricular fibrillation resistant to cardioversion)
Interaction
Interaction
Medicines that can cause torsades de pointes are primarily class Ia and class III antiarrhythmic drugs and some antipsychotics. Hypokalemia is a predisposing factor, as is bradycardia or congenital or acquired prolongation of the QT interval.
Combinations with
– Drugs that can cause ventricular tachycardia of the “pirouette” type.
– Class Ia antiarrhythmic drugs (quinidine, hydroquinidine, isopyramide).
– Class III antiarrhythmic drugs (dofetilide, ibutilide, sotalol).
– Other drugs, such as bepridil, cisapride, difemanil, IV ritromycin, mizolastine, IV vincamine, moxifloxacin, IV spiramycin.
– Sultopride.
The risk of ventricular rhythm disturbances (pirouette-type tachycardia) increases.
These contraindications do not apply to the use of amiodarone for cardiopulmonary resuscitation in cardiac arrest refractory to electrical defibrillation.
Not recommended combinations with
Cyclosporine
There may be an increase in the level of cyclosporine in plasma, associated with a decrease in the metabolism of the drug in the liver, with possible nephrotoxic manifestations.
Determination of the level of cyclosporine in the blood, checking renal function and reviewing the dosage during treatment with amiodarone and after discontinuation of the drug.
Diltiazem for injection
Risk of bradycardia and atrioventricular block. If a combination is unavoidable, strict clinical and continuous ECG monitoring should be established.
Verapamil for injection
Risk of bradycardia and atrioventricular block. If a combination is unavoidable, strict clinical and continuous ECG monitoring should be established.
Antiparasitic drugs that can cause torsade de pointes (halofantrine, pentamidine, lumefantrine)
If the combination is unavoidable, preliminary control of the QT interval and ECG monitoring is necessary.
Neuroleptics that can cause ventricular tachycardia of the “pirouette” type:
Some phenothiazine antipsychotics (chlorpromazine, cyamemazine, levomepromazine, thioridazine, trifluoperazine), benzamides (amisulpride, sulpiride, tiapride, veralipride), butyrophenones (droperidol, haloperidol), other antipsychotics (pimozide).
The risk of ventricular rhythm disturbances (pirouette-type tachycardia) increases.
Methadone
The risk of ventricular rhythm disturbances (pirouette-type tachycardia) increases. Recommended: ECG and clinical observation.
Combinations requiring precautions when using Amiodarone with:
Oral anticoagulants:
Increased anticoagulation effect and risk of bleeding, due to increased concentrations of anticoagulants in plasma. The need for more frequent monitoring of the level of prothrombin in the blood and MHO (INR), as well as adaptation of doses of anticoagulants during treatment with amiodarone and after discontinuation of the drug.
Beta blockers, with the exception of sotalol (contraindicated combination) and esmolol (combination requiring caution when used)
Violations of contractility, automatism and conduction (suppression of compensatory sympathetic mechanisms). Clinical and ECG monitoring.
Beta blockers prescribed for heart failure (bisoprolol, carvedilol, metoprolol)
Impaired contractility and conduction (synergistic effect) with the risk of developing severe bradycardia. Increased risk of ventricular arrhythmias, especially torsade de pointes.
Regular clinical and electrocardiographic monitoring is necessary.
Cardiac glycosides
Disorders of automaticity (excessive bradycardia) and atrioventricular conduction (synergism of action). When using digoxin, its concentration in plasma increases (due to decreased clearance of the alkaloid).
It is necessary to carry out clinical and ECG monitoring, as well as determination of plasma digoxin levels); It may be necessary to change the dose of digoxin.
Diltiazem for oral administration
Risk of bradycardia and atrioventricular block, especially in the elderly. Clinical and ECG control.
Verapamil for oral administration
Risk of bradycardia and atrioventricular block, especially in the elderly. Clinical and ECG control.
Essex scraper
Violations of contractility, automatism and conduction (suppression of compensatory sympathetic mechanisms). Clinical and ECG monitoring.
Hypokalemic drugs: potassium-sparing diuretics (in monotherapy or combination), stimulant laxatives, amphotericin B (iv), glucocorticoids (systemic), tetracosactide.
The risk of ventricular rhythm disturbances increases, especially tachycardia of the “pirouette” type (hypokalemia is a predisposing factor). Clinical and ECG monitoring, laboratory tests.
Lidocaine
Risk of increased lidocaine plasma concentrations, with the possibility of neurological and cardiac side effects, due to amiodarone’s decreased metabolism of lidocaine in the liver. Clinical and ECG monitoring, if necessary, dose adjustment of lidocaine during treatment with amiodarone and after its discontinuation.
Orlistat
Risk of decreased plasma concentrations of amiodarone and its active metabolite. Clinical and, if necessary, ECG monitoring,
Phenytoin (and, by extrapolation, fosphenytoin)
An increase in the level of phenytoin in plasma with symptoms of overdose, especially of a neurological nature (decreased metabolism of phenytoin in the liver). Clinical monitoring and determination of plasma phenytoin levels; if possible, reduce the dose of phenytoin.
Simvastatin
Increased risk of side effects (depending on dose) such as rhabdomyolysis (decreased metabolism of simvastatin in the liver). The dose of simvastatin should not exceed 20 mg per day.
If a therapeutic effect is not achieved at this dose, you should switch to another statin that does not interact with this type of interaction.
Tacrolimus
An increase in the level of tacrolimus in the blood due to inhibition of its metabolism by amiodarone. Measurement of tacrolimus blood levels, monitoring of kidney function and leveling of tacrolimus levels should be carried out.
Drugs that cause bradycardia:
Many drugs can cause bradycardia. This is especially true for class Ia antiarrhythmic drugs, beta blockers, some class III antiarrhythmic drugs, some calcium channel blockers, digitalis, pilocarpine and anticholinesterase agents.
Risk of excessive bradycardia (cumulative effect).
Combinations to Consider
Drugs that cause bradycardia: calcium channel blockers with bradycardic effect (verapamil), beta blockers (except sotalol), clonidine, guanfacine, digitalis alkaloids, mefloquine, cholinesterase inhibitors (donezepil, galantamine, rivastigmine, tacrine, ambemonium, pyridostigmine, neostigmine), pilocarpine.
Risk of excessive bradycardia (cumulative effects).
Incompatibilities
When PVC material or medical equipment plasticized with 2-diethylhexyl phthalate (DEHP) is used in the presence of amiodarone injection solution, DEHP may be released. To minimize exposure to DEHP, it is recommended that the solution be final diluted before infusion in DEHP-free equipment.
Overdose
Overdose
Symptoms: sinus bradycardia, cardiac arrest, paroxysmal ventricular tachycardia, ventricular tachycardia of the “pirouette” type, circulatory disorders, liver dysfunction, decreased blood pressure.
Treatment: symptomatic therapy is carried out (for bradycardia – beta-adrenergic stimulants or installation of a pacemaker, for pirouette-type tachycardia – intravenous administration of magnesium salts, reducing pacemaker). Amiodarone and its metabolites are not removed by hemodialysis and peritoneal dialysis.
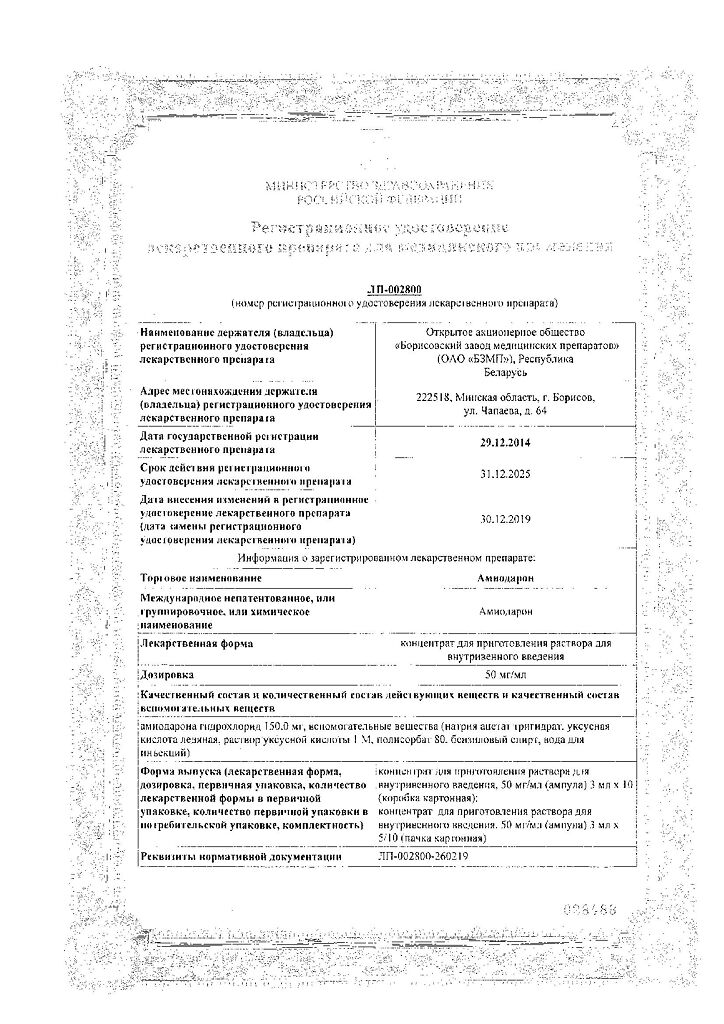
Manufacturer
Manufacturer
Borisov Medical Preparations Plant, Belarus
Additional information
| Manufacturer | Borisov Medical Preparations Plant, Belarus |
|---|---|
| Medication form | solution concentrate |
| Brand | Borisov Medical Preparations Plant |
Other forms…
Related products
Buy Amiodarone, 50 mg/ml concentrate 3 ml 10 pcs with delivery to USA, UK, Europe and over 120 other countries.