No products in the cart.
Amelotex, tablets 15 mg 20 pcs
€10.56 €9.24
Description
Pharmgroup:
NSAIDs.
Pharmic action:
Amelotex is an NSAID with anti-inflammatory, antipyretic, analgesic effects. It belongs to the class of oxycams; a derivative of enolic acid.
Meloxicam is a non-steroidal anti-inflammatory drug with analgesic, anti-inflammatory and antipyretic effects.
The anti-inflammatory action is associated with inhibition of the enzymatic activity of cyclooxygenase-2 (COX-2), which is involved in the biosynthesis of prostaglandins in the area of inflammation.
To a lesser extent, meloxicam acts on cyclooxygenase-1 (COX-1), which is involved in the synthesis of prostaglandin, which protects the mucosa of the gastrointestinal tract and is involved in the regulation of blood flow in the kidneys.
Pharmacokinetics:
Amelotex is well absorbed from the gastrointestinal tract, the absolute bioavailability of meloxicam is 89%. Simultaneous intake of food does not change absorption. When using the drug Amelotex orally in doses of 7.5 and 15 mg, its concentrations are proportional to the doses. Equilibrium concentrations are reached within 3-5 days. With long-term use of the drug (more than 1 year), the concentrations are similar to those observed after the first achievement of equilibrium concentrations. Binding to plasma proteins is more than 99%. The range of differences between maximal and basal concentrations of the preparation after its once-daily use is relatively small, 0.4 – 1.0 µg/ml, and 0.8-2.0 µg/ml, when using 7.5 mg dosage, and 0.8-2.0 µg/ml, when using 15 mg dosage (Cmin and Cmax values are indicated, respectively). Meloxicam penetrates through histohematic barriers, the concentration in synovial fluid reaches 50% of the maximum concentration of the drug in plasma.
It is almost completely metabolized in the liver to form four pharmacologically inactive derivatives. The main metabolite, 5′-carboxymeloxicam (60% of the dose value), is formed by oxidation of the intermediate metabolite, 5′-hydroxymethylmeloxicam, which is also excreted, but to a lesser extent (9% of the dose value). In vitro studies have shown that CYP 2C9 isoenzyme plays an important role in this metabolic transformation, CYP 3A4 isoenzyme has additional importance. Peroxidase, the activity of which probably varies individually, is involved in the formation of the other two metabolites (which constitute, respectively, 16% and 4% of the value of the drug dose).
Extracted equally through the intestine and kidneys, mainly as metabolites. Less than 5% of daily dose is excreted unchanged in intestine, in urine the drug is excreted unchanged only in trace amounts. The half-life (T1/2) of meloxicam is 15-20 hours. Plasma clearance averages 8 ml/min. The drug clearance is decreased in elderly patients. The volume of distribution is low and averages 11 l. Hepatic or renal insufficiency of moderate severity has no significant effect on the pharmacokinetics of meloxicam.
Indications
Indications
osteoarthritis;
rheumatoid arthritis;
ankylosing spondylitis (ankylosing spondylitis);
Amelotex is intended for symptomatic therapy, reducing pain and inflammation at the time of use, and does not affect the progression of the disease.
Pharmacological effect
Pharmacological effect
Pharmaceutical group:
NSAIDs.
Pharmaceutical action:
Amelotex is an NSAID that has anti-inflammatory, antipyretic, and analgesic effects. Belongs to the class of oxicams; enolic acid derivative.
Meloxicam is a non-steroidal anti-inflammatory drug that has analgesic, anti-inflammatory and antipyretic effects.
The anti-inflammatory effect is associated with inhibition of the enzymatic activity of cyclooxygenase-2 (COX-2), which is involved in the biosynthesis of prostaglandins in the area of inflammation.
To a lesser extent, meloxicam acts on cyclooxygenase-1 (COX-1), which is involved in the synthesis of prostaglandin, which protects the mucous membrane of the gastrointestinal tract and takes part in the regulation of blood flow in the kidneys.
Pharmacokinetics:
Amelotex is well absorbed from the gastrointestinal tract, the absolute bioavailability of meloxicam is 89%. Concomitant food intake does not alter absorption. When using the drug Amelotex orally in doses of 7.5 and 15 mg, its concentrations are proportional to the doses. Equilibrium concentrations are achieved within 3-5 days. With long-term use of the drug (more than 1 year), concentrations are similar to those observed after the first achievement of equilibrium concentrations. Plasma protein binding is more than 99%. The range of differences between the maximum and basal concentrations of the drug after taking it once a day is relatively small and is 0.4 – 1.0 μg/ml when using a dose of 7.5 mg, and 0.8-2.0 μg/ml when using a dose of 15 mg (Cmin and Cmax values are given, respectively). Meloxicam penetrates histohematic barriers, the concentration in synovial fluid reaches 50% of the maximum concentration of the drug in plasma.
Almost completely metabolized in the liver to form four pharmacologically inactive derivatives. The main metabolite, 5′-carboxymeloxicam (60% of the dose), is formed by oxidation of the intermediate metabolite, 5′-hydroxymethylmeloxicam, which is also excreted, but to a lesser extent (9% of the dose). In vitro studies have shown that the CYP 2C9 isoenzyme plays an important role in this metabolic transformation; the CYP 3A4 isoenzyme is of additional importance. Peroxidase is involved in the formation of the other two metabolites (constituting, respectively, 16% and 4% of the drug dose), the activity of which probably varies individually.
It is excreted equally through the intestines and kidneys, mainly in the form of metabolites. Less than 5% of the daily dose is excreted unchanged through the intestines; the drug is found unchanged in urine only in trace amounts. The half-life (T1/2) of meloxicam is 15-20 hours. Plasma clearance averages 8 ml/min. In elderly people, drug clearance is reduced. The volume of distribution is low, averaging 11 liters. Moderate hepatic or renal impairment does not significantly affect the pharmacokinetics of meloxicam.
Special instructions
Special instructions
If peptic ulcers or gastrointestinal bleeding occur, or side effects on the skin and mucous membranes develop, the drug should be discontinued.
In patients with a decrease in circulating blood volume and reduced glomerular filtration (dehydration, chronic heart failure, surgery), clinically pronounced chronic renal failure may occur, which is completely reversible after discontinuation of the drug (in such patients, daily diuresis and renal function should be monitored at the beginning of treatment).
If there is a persistent and significant increase in transaminases and changes in other indicators of liver function, the drug should be discontinued and control tests performed. In patients with an increased risk of side effects, treatment begins with a dose of 7.5 mg.
In end-stage chronic renal failure in patients on dialysis, the dose should not exceed 7.5 mg/day.
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions (if dizziness and drowsiness occur).
Active ingredient
Active ingredient
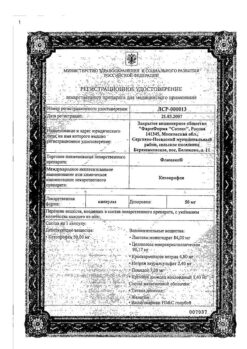
Meloxicam
Composition
Composition
1 tablet contains meloxicam 15 mg.
Pregnancy
Pregnancy
Contraindicated during pregnancy and breastfeeding.
Contraindications
Contraindications
Hypersensitivity to the active substance or auxiliary components;
Contraindicated in the period after coronary artery bypass grafting;
uncompensated heart failure;
Complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid and other non-steroidal anti-inflammatory drugs (including a history);
Erosive and ulcerative changes in the mucous membrane of the stomach or duodenum, active gastrointestinal bleeding;
Inflammatory bowel diseases (ulcerative colitis, Crohn’s disease);
Cerebrovascular bleeding or other bleeding;
Severe liver failure or active liver disease;
Severe renal failure in patients not undergoing dialysis (creatinine clearance less than 30 ml/min), progressive kidney disease, incl. confirmed hyperkalemia;
Pregnancy, breastfeeding period;
Children under 15 years of age.
With caution
To reduce the risk of adverse events, the minimum effective dose should be used in the shortest possible short course for coronary heart disease, cerebrovascular diseases, congestive heart failure, dyslipidemia/hyperlipidemia, diabetes mellitus, peripheral arterial disease, smoking, creatinine clearance less than 60 ml/min, anamnestic data on the development of ulcerative lesions of the gastrointestinal tract, in the presence of Helicobacter infection pylori, in old age, with long-term use of non-steroidal anti-inflammatory drugs, frequent alcohol consumption, severe somatic diseases, concomitant therapy with the following drugs: anticoagulants (for example, warfarin), antiplatelet agents (for example, acetylsalicylic acid, clopidogrel), oral glucocorticosteroids (for example, prednisolone), selective serotonin reuptake inhibitors (for example citalopram, fluoxetine, paroxetine, sertraline).
Side Effects
Side Effects
From the digestive system: nausea, vomiting, belching, abdominal pain, constipation or diarrhea, flatulence, increased activity of liver transaminases, hyperbilirubinemia, stomatitis, erosive and ulcerative lesions of the gastrointestinal tract, esophagitis, gastritis, colitis, perforation of the gastrointestinal tract, gastrointestinal bleeding (latent or obvious), hepatitis
From the nervous system: dizziness, vertigo, headache, tinnitus, confusion, drowsiness, disorientation, emotional lability.
From the respiratory system: bronchospasm.
From the hematopoietic organs: anemia, leukopenia, thrombocytopenia.
From the cardiovascular system: peripheral edema, increased blood pressure, “flushes” of blood to the skin of the face and upper chest, palpitations.
From the urinary system: edema, hypercreatininemia, increased concentration of urea in the blood serum. In rare cases – acute renal failure, interstitial nephritis, albuminuria, hematuria.
From the senses: conjunctivitis, visual impairment, incl. blurred vision.
From the skin: itching, skin rash, urticaria, photosensitivity, bullous rashes, erythema multiforme, toxic epidermal necrolysis.
Allergic reactions: angioedema, anaphylactoid, anaphylactic reactions.
Interaction
Interaction
When used simultaneously with other non-steroidal anti-inflammatory drugs (as well as acetylsalicylic acid), the risk of erosive and ulcerative lesions and bleeding from the gastrointestinal tract increases. When used simultaneously with antihypertensive drugs, the effectiveness of the latter may be reduced.
When used simultaneously with lithium preparations, the development of accumulation of lithium and an increase in its toxic effect is possible (monitoring the concentration of lithium in the blood is recommended).
When used simultaneously with methotrexate, the latter’s side effect on the hematopoietic system increases (the risk of anemia and leukopenia; periodic monitoring of a general blood test is indicated).
When used simultaneously with diuretics and cyclosporine, the risk of developing renal failure increases.
When used simultaneously with intrauterine contraceptives, the effectiveness of the latter may decrease.
When used simultaneously with anticoagulants (heparin, ticlopidine, warfarin), as well as with thrombolytic drugs (streptokinase, fibrinolysin), the risk of bleeding increases (periodic monitoring of blood clotting parameters is required).
When used simultaneously with cholestyramine, the binding of meloxicam increases its excretion through the gastrointestinal tract.
When used simultaneously with selective serotonin reuptake inhibitors, the risk of gastrointestinal bleeding increases.
Overdose
Overdose
Symptoms: impaired consciousness, nausea, vomiting, epigastric pain, gastrointestinal bleeding, acute renal failure, liver failure, respiratory arrest, asystole.
Treatment: there is no specific antidote; in case of an overdose of the drug, gastric lavage, taking activated charcoal (within the next hour), and symptomatic therapy should be performed. Cholestyramine accelerates the elimination of the drug from the body. Forced diuresis and hemodialysis are ineffective due to the high binding of the drug to blood proteins.
Storage conditions
Storage conditions
In a place protected from light at a temperature of 8 to 25 ° C
Shelf life
Shelf life
2 years.
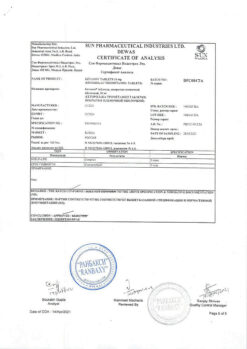
Manufacturer
Manufacturer
Replek Farm, Republic of North Macedonia
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | In a place protected from light at a temperature of 8 to 25 ° C |
| Manufacturer | Replek Farm, Republic of Northern Macedonia |
| Medication form | pills |
| Brand | Replek Farm |
Other forms…
Related products
Buy Amelotex, tablets 15 mg 20 pcs with delivery to USA, UK, Europe and over 120 other countries.