No products in the cart.
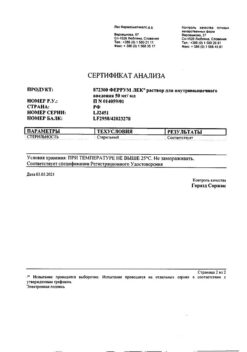
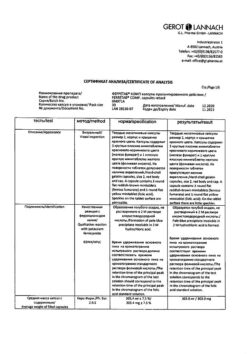
Actilyse®, 50 mg
€1.00
Out of stock
(E-mail when Stock is available)
Description
Trombolytic. Recombinant human tissue plasminogen activator, glycoprotein.
When administered intravenously, the drug is relatively inactive in the systemic bloodstream. It is activated after binding to fibrin, inducing transformation of plasminogen into plasmin, which leads to dissolution of fibrin clot.
Administration of Actilyse reduces the release of the enzyme alpha-hydroxybutyrate dehydrogenase.
Administration of Actilyse at a dose of 100 mg for 90 minutes in conjunction with intravenous heparin administration in more than 40,000 patients with acute myocardial infarction (GUSTO studies) resulted in reduced 30-day mortality (6.3%) compared with the use of streptokinase (1.5 million units for 60 min) simultaneously with p/c or intravenous heparin administration (7.3%). It was shown that after 60 min and 90 min of thrombolysis in patients treated with Actilyse, there was a higher rate of recovery of vascular patency in the infarct zone, compared with the use of streptokinase. No differences in the frequency of vascular patency were noted 180 min after the start of therapy and later.
A decrease in 30-day mortality after myocardial infarction was observed with Actilyse compared with patients who did not receive thrombolytic therapy.
Patients who received Actilise, compared with patients who did not receive thrombolytic therapy, showed less significant damage to overall left ventricular heart function and local wall motility.
In a placebo-controlled trial (LATE), administration of Actilise at a dose of 100 mg for 3 hours in patients with myocardial infarction (if initiated within 6-12 hours of symptom onset), was shown to result in reduced 30-day mortality compared with placebo. Therapeutic effect in patients with confirmed myocardial infarction was also noted when treatment was started within 24 h after the onset of symptoms.
In patients with acute massive pulmonary embolism accompanied by unstable hemodynamics, use of Actylise leads to rapid reduction of thrombus size and decreased pulmonary artery pressure, but no data on mortality are available.
Two U.S. studies (NINDS A/B) examining the effect of the drug in stroke (during the first 3 hours after the onset of symptoms) found more frequent favorable outcomes (no or minimal impairment in patients’ ability to function) compared to placebo.
In case of initiation of therapy at a later time, the effectiveness of the drug decreases, which was shown in two European studies and in an additional study conducted in the USA.
Results of a meta-analysis of all patients who received therapy during the first 3 h after the onset of stroke confirmed the presence of a positive effect of alteplase.
Despite the increased risk of serious and even fatal intracranial hemorrhage, the probability of developing a favorable outcome of therapy compared to placebo was 14.9% (95% confidence intervals: 8.1% and 21.7%). These data do not allow a definite conclusion regarding the effect of therapy on mortality. The benefit/risk ratio in the case of use of alteplase within 3 h after stroke onset (taking into account the caveats above) can generally be considered favorable, although study data do not allow a definite conclusion regarding the effect of therapy on mortality.
Meta-analysis of all available clinical data shows that alteplase is less effective in patients whose treatment is started 3-6 h after symptom onset compared with therapy undertaken in the first 3 h after the development of clinical manifestations. At the same time, the risk of complications of stroke therapy is higher in the former case, resulting in an unfavorable benefit/risk ratio outcome.
Due to its relative specificity to fibrin, use of alteplase at a dose of 100 mg leads to a moderate decrease in circulating fibrinogen levels (to about 60% after 4 h), which tend to increase by more than 80% by 24 h. Plasminogen and alpha-2-antiplasmin concentrations decrease to 20% and 35% of baseline levels, respectively, after 4 h, and rise again to more than 80% after 24 h. A significant and lasting decrease in circulating fibrinogen levels has been observed in only a small number of patients.
Indications
Indications
– thrombolytic therapy of acute myocardial infarction in the first 6 h after the development of symptoms (90-minute /accelerated/ dosing regimen);
– thrombolytic therapy of acute myocardial infarction in the period from 6 to 12 h after the development of symptoms (3-hour dosing regime);
– thrombolytic therapy for acute massive pulmonary thromboembolism accompanied by unstable hemodynamics, the diagnosis should be confirmed objectively if possible (e.g., by pulmonary angiography or noninvasive methods such as pulmonary imaging). Clinical studies regarding mortality and long-term outcomes of pulmonary embolism have not been conducted;
– Thrombolytic therapy for acute ischemic stroke (indicated only if administered within 3 h after development of stroke symptoms, and if intracranial hemorrhage /hemorrhagic stroke/ is excluded by appropriate imaging techniques, such as brain computed tomography).
Active ingredient
Active ingredient
Composition
Composition
1 vial contains alteplase 50 mg.
How to take, the dosage
How to take, the dosage
Actilise should be administered as soon as possible from the onset of symptoms.
In myocardial infarction on a 90-minute (accelerated) dosing regimen for patients in whom treatment can be initiated within 6 h of symptom development,the drug is administered at a dose of 15 mg by IV infusion, then 50 mg by IV infusion for the first 30 min, followed by a 35 mg infusion for 60 min to reach a maximum dose of 100 mg.
In patients with body weight less than 65 kg the drug dose should be calculated according to the body weight. The drug is firstly administered in dose of 15 mg by intravenous stream, then 750 mcg/kg of body weight (maximum 50 mg) during 30 minutes by intravenous drop infusion followed by infusion of 500 mcg/kg (maximum 35 mg) during 60 minutes.
In myocardial infarction on a 3-hour dosing regimen for patients in whom treatment can be initiated between 6 h and 12 h after the development of symptoms, the drug is administered at a dose of 10 mg by IV jet, followed by 50 mg as an IV infusion for the first hour, followed by a 10 mg IV infusion for 30 min until a maximum dose of 100 mg is reached within 3 h.
In patients with a body weight less than 65 kg, the total dose should not exceed 1.5 mg/kg.
The recommended maximum dose of Actylise in acute myocardial infarction is 100 mg.
Complementary therapy: acetylsalicylic acid should be administered as soon as possible after the onset of thrombosis and continued for the first months after the myocardial infarction. The recommended dose is 100-300 mg/day. At the same time, heparin should be started for 24 h or more (for accelerated dosing regimen, at least 48 h). It is recommended to start with intravenous heparin jet injection at a dose of 5000 units/h before the start of thrombolytic therapy. Subsequently, heparin is administered by infusion at a rate of 1000 units/h. The dose of heparin should be adjusted depending on the results of repeated determination of the AFTV (values should exceed the initial level by 1.5-2.5 times).
In pulmonary thromboembolism Aktilise is administered in a total dose of 100 mg for 2 hours. The best experience is obtained using the following dosing regimen: first, the drug is administered in a dose of 10 mg by IV stream for 1-2 minutes, then – 90 mg by IV drip for 2 hours. In patients with body weight less than 65 kg the total dose should not exceed 1.5 mg/kg of body weight.
Complementary therapy: after use of Actilyse, if ACTV exceeds the initial level by less than 2 times, heparin should be administered (or continued). Further infusion is also performed under control of the AFTTV, which should not exceed baseline by more than 1.5-2.5 times.
In ischemic stroke, the recommended dose is 900 mcg/kg (maximum 90 mg), as an IV infusion within 60 min after the initial IV jet dose of 10% of the cumulative dose. Therapy should be initiated as soon as possible after the onset of symptoms (preferably within 3 h).
Complementary therapy: safety and efficacy of the above therapy regimen used in combination with heparin and acetylsalicylic acid in the first 24 h after the onset of symptoms have not been adequately studied. Therefore, the use of acetylsalicylic acid or intravenous heparin should be avoided during the first 24 h after the onset of Actilyse. If heparin is required for other indications (e.g. to prevent deep vein thrombosis), the dose should not exceed 10,000 ME per day, and the drug should be given by injection by mouth.
Interaction
Interaction
There have been no special studies of interaction of Actilise with other drugs commonly used in acute myocardial infarction.
The use of drugs that affect blood clotting or alter platelet function before, during or after initiation of therapy with Actilise may increase the risk of bleeding.
Concomitant use of ACE inhibitors may increase the risk of anaphylactoid reactions. These reactions have been observed in a relatively larger proportion of patients receiving ACE inhibitors.
Pharmaceutical Interactions
Actilise must not be mixed with other medicinal products (even heparin), either in an infusion bottle or in a general IV system.
Special Instructions
Special Instructions
In the following cases when prescribing Aktilise, the degree of expected benefit and possible risk of bleeding should be carefully evaluated:
– Recently performed IV/m injection or small recent interventions such as biopsy, puncture of large vessels, cardiac massage during resuscitation;
– diseases (not mentioned in the list of contraindications) in which the risk of bleeding is increased.
During the treatment of acute myocardial infarction and acute pulmonary embolism the drug should be used with caution:
– With systolic blood pressure over 160 mm Hg;
– In elderly patients when the risk of intracranial hemorrhage may increase. Because in elderly patients the possibility of positive result of this treatment also increases, the benefit/risk ratio should be carefully evaluated.
Caution should be exercised while treating acute ischemic stroke since Aktilize administration in this category of patients (in comparison with its use for other indications) is accompanied by a markedly increased risk of intracranial hemorrhage as the bleeding occurs mostly in necrotic area.
This especially should be taken into account. Given the increased risk of cerebral hemorrhage, the dose of alteplase used should not exceed 900 mcg/kg (maximum dose is 90 mg).
The treatment should not be started later than 3 hours after the onset of symptoms due to an unfavorable benefit/risk ratio, which is due to the following circumstances:
– the positive effect of treatment is reduced if the therapy is started late;
– mortality increases mainly in patients who previously received acetylsalicylic acid;
– the risk of bleeding increases.
Treatment with Actilyse should be performed by a physician experienced in thrombolytic therapy and able to monitor its effectiveness. It is recommended that standard resuscitation equipment and appropriate medications be available when using Actilyse.
The most common complication of Actilyse therapy is bleeding. Simultaneous use of heparin may contribute to bleeding. Because Actilyse dissolves fibrin, bleeding from recent puncture sites may occur. Therefore, thrombolytic therapy requires careful monitoring of areas of possible bleeding (including sites of catheter insertion, arterial and venous punctures, incisions and injections). The use of rigid catheters, intravenous injections and unwarranted manipulations during treatment with Actilyse should be avoided.
In case of severe bleeding, especially cerebral bleeding, fibrinolytic therapy, as well as heparin administration should be stopped immediately. If heparin was used within 4 h before the onset of bleeding, the feasibility of using protamine should be considered. In rare cases, when the above conservative measures are ineffective, the use of blood products may be indicated. Transfusion of cryoprecipitate, fresh frozen plasma and platelets may be administered according to clinical and laboratory parameters determined repeatedly after each infusion. Cryoprecipitate infusion should preferably be administered until a fibrinogen concentration of 1 g/L is reached. Antifibrinolytic agents (e.g. tranexamic acid) may be considered, but no special studies have been conducted.
In acute myocardial infarction and pulmonary embolism, Aktilize should not be used in a dose greater than 100 mg, and in acute ischemic stroke – in a dose greater than 90 mg, because there is an increased risk of intracerebrospinal fibrinogen.
No sustained formation of antibodies to recombinant human tissue plasminogen activator was observed after treatment termination. There is no systematized experience of repeated use of Aktilize. In case of anaphylactoid reaction, the infusion should be discontinued and appropriate treatment administered. Regular monitoring of treatment tolerance is recommended, especially in patients concomitantly receiving ACE inhibitors.
When treating acute myocardial infarction, the following precautions should be additionally kept in mind:
– coronary thrombolysis may lead to reperfusion-related arrhythmias;
– there is no experience with glycoprotein IIb/IIIa antagonists during the first 24 h after treatment initiation;
– use of thrombolytics may increase the risk of thromboembolism in patients with left heart thrombosis, such as in mitral stenosis or atrial fibrillation.
The following precautions should additionally be kept in mind when treating acute stroke.
Treatment should be performed exclusively by an experienced physician with skills and experience in intensive neurological care, in a specialized department setting with the ability to perform a full range of neuroimaging studies.
BP should be monitored during treatment and for 24 h after treatment has ended. If systolic BP rises above 180 mmHg or diastolic BP rises below 105 mmHg, IV administration of antihypertensive drugs is recommended.
Therapeutic effect is reduced in patients who have had a previous stroke or in the presence of uncontrolled diabetes mellitus. In such patients, the benefit/risk ratio is considered less favorable, although still positive. In patients with very minor stroke, the risk exceeds the expected benefit, so the use of Actilise is not recommended.
Patients with very severe stroke have an increased risk of intracranial hemorrhage and death. In these cases, Actilise should not be used.
Patients with massive brain infarcts have an increased risk of adverse outcome, including marked intracerebral hemorrhage and death. In such cases, the risks and benefits of therapy should be carefully weighed.
For stroke, the likelihood of a favorable treatment outcome decreases with increasing age, as the severity of the stroke increases, and with elevated blood glucose levels. At the same time, the likelihood of serious disability and death or serious intracranial hemorrhage increases regardless of treatment. Actilise should not be used in patients over 80 years of age, in cases of severe stroke (based on clinical data and/or imaging studies) and when baseline blood glucose values are less than 50 mg/dL or greater than 400 mg/dL.
Ischemic reperfusion may lead to cerebral edema in the infarct area. Because of the increased risk of hemorrhagia, the use of platelet aggregation inhibitors should not be started within the first 24 h after thrombolysis with alteplase.
Use in Pediatrics
There is currently limited experience with Aktilise in children.
Contraindications
Contraindications
– hemorrhagic diathesis;
– bleeding at present or during the previous 6 months;
– simultaneous use of oral anticoagulants (e.g., warfarin; international normalized ratio >1.3);
– history of CNS disorders (including neoplasms, aneurysm);
– surgical intervention on the brain or spinal cord;
– intracranial (including
– intracranial (including subarachnoid) hemorrhage at the present moment or in the anamnesis;
– suspected hemorrhagic stroke;
– severe uncontrolled arterial hypertension;
– major surgical intervention or severe trauma during the previous 10 days (including any trauma in combination with this acute myocardial infarction);
– recent craniocerebral trauma;
– prolonged or traumatic cardiopulmonary resuscitation (more than 2 minutes), labor within the previous 10 days;
– recent puncture of incompressible blood vessels (e.g., subclavian and jugular vein);
– hemorrhagic retinopathy (includingÑ.
– bacterial endocarditis;
– pericarditis;
– acute pancreatitis;
– confirmed gastric and duodenal ulcer during the last 3 months;
– Severe liver diseases, including liver insufficiency, cirrhosis, portal hypertension (with esophageal varices), active hepatitis;
– Arterial aneurysms, congenital malformations of arteries and veins;
– neoplasms with increased risk of bleeding;
– Hypersensitivity to the preparation components.
In case of using the drug for the treatment of acute myocardial infarction and pulmonary embolism, in addition to the above contraindications, there is the following contraindication:
– stroke in the anamnesis.
If the drug is used for the treatment of acute ischemic stroke, in addition to the above contraindications, there are the following contraindications:
– the onset of ischemic stroke symptoms more than 3 h before the start of the infusion, or lack of accurate information about the time of onset;
– rapid improvement in acute ischemic stroke or mild severity of symptoms by the time the infusion begins;
– severe stroke, based on clinical findings (e.g., if NIHSS>25) and/or appropriate imaging techniques;
– seizures at stroke onset;
– evidence of a previous stroke or serious head trauma within the previous 3 months;
– occurrence of a previous stroke on the background of diabetes mellitus;
– Administration of heparin within 48 hours prior to stroke, if activated partial thrombin time (APT) is increased at this moment;
– Administration of antiplatelet agents at the moment of infusion and within 24 hours after infusion;
– Platelet count is less than 100 000/mm3*;
– Systolic BP is higher than 185 mm Hg.
– systolic BP greater than 185 mm Hg, or diastolic BP greater than 110 mmHg, or intensive therapy (intravenous drug administration) is necessary to reduce BP to these limits;
– blood glucose level is less than 50 mg/dl or more than 400 mg/dl.
Actilise is not indicated for acute stroke therapy in children and adolescents under 18 years old and in adults over 80 years old.
Side effects
Side effects
The most common side effect is bleeding, resulting in a decrease in hematocrit and/or hemoglobin.
Bleeding associated with thrombolytic therapy can be divided into two main categories:
– external bleeding (usually from puncture sites or injuries of blood vessels);
– internal bleeding from the GI tract, urinary tract, retroperitoneal bleeding, brain hemorrhage or bleeding from parenchymal organs.
The data below are based on results from clinical trials of Actilise in 8299 patients with acute myocardial infarction.
A case of cholesterol crystal embolization not observed in the population of patients enrolled in clinical trials is based on a separate report.
Compared with studies in myocardial infarction, the number of patients with pulmonary embolism and stroke who participated in clinical trials (within 0-3 h of the onset of symptoms of these diseases) was very small. Therefore, the small numerical differences noted when comparing with data from myocardial infarction were most likely a consequence of the small sample size. Other than intracranial hemorrhage (as a side effect in stroke) and reperfusion arrhythmias (as a side effect in myocardial infarction), there is no clinical evidence to suggest qualitative and quantitative differences in the spectrum of side effects of Actylise when used for pulmonary embolism and acute ischemic stroke, or for myocardial infarction.
Side effects noted with use in myocardial infarction
Very common: reperfusion arrhythmias, which can be life threatening and may require conventional antiarrhythmic therapy.
Side effects noted with myocardial infarction and pulmonary embolism
Rare: intracranial hemorrhage.
Side effects noted with acute ischemic stroke
Frequent: intracranial hemorrhage. The main adverse events were clinically pronounced intracranial hemorrhages (their frequency reached 10%). However, there was no increase in the incidence of complications or overall mortality.
Side effects noted with myocardial infarction, pulmonary embolism and acute ischemic stroke
Very common: external bleeding, usually from puncture sites or from damaged blood vessels, BP decrease.
Frequently: gastrointestinal bleeding, nausea, vomiting (nausea and vomiting could also be symptoms of myocardial infarction), increased body temperature, bleeding from the urinary tract, nasal bleeding, ecchymosis.
Infrequent: retroperitoneal hemorrhage, gingival hemorrhage, thromboembolism, which may be accompanied by the corresponding consequences of the affected internal organs. Anaphylactoid reactions have been reported (usually mild, but in some cases may be life-threatening); rash, urticaria, bronchospasm, angioedema, hypotension, shock or any other allergic reactions are possible. In case of development of these reactions, generally accepted antiallergic therapy should be used. It was found that in a relatively large proportion of patients with such reactions, ACE inhibitors were used simultaneously. Anaphylactic reactions (i.e., caused by IgE) for Actylise are unknown.
Rare: transient antibody formation to Actylise (in low titers), but the clinical significance of this phenomenon has not been established; cholesterol crystal embolization, which may lead to related effects on the affected internal organs; bleeding from parenchymal organs.
Blood transfusion was often required.
Overdose
Overdose
Symptoms: despite the relative specificity to fibrin, a clinically significant decrease in fibrinogen and clotting factors may be observed in overdose.
Treatment: in most cases, a wait-and-see tactic with the expectation of physiological regeneration of these factors after discontinuation of Aktilize is sufficient. If severe bleeding occurs, a transfusion of fresh frozen plasma or fresh whole blood is recommended; synthetic antifibrinolytic agents may be prescribed if necessary.
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a light-protected place, at a temperature below 25 °C |
| Manufacturer | Boehringer Ingelheim Pharma GmbH & Co. |
| Brand | #Н/Д |
Related products
Buy Actilyse®, 50 mg with delivery to USA, UK, Europe and over 120 other countries.