No products in the cart.
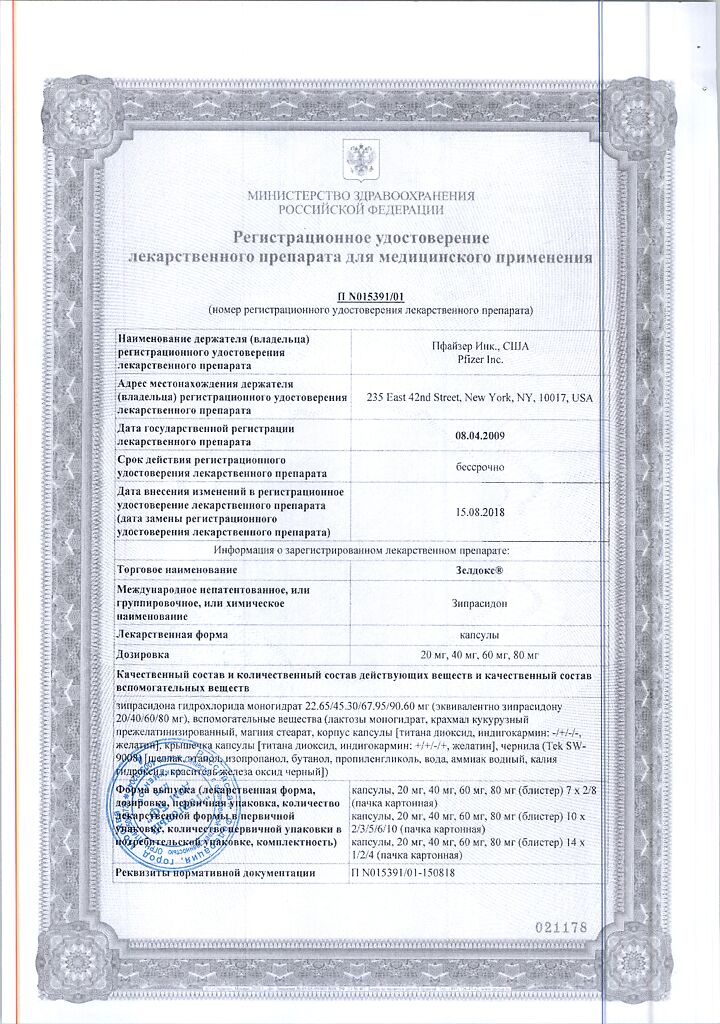
Zeldox, 40 mg capsules 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Zeldox is an antipsychotic drug (neuroleptic).
It has high affinity for dopamine D2 receptors and much stronger affinity for serotonin 5-HT2A receptors; it also interacts with serotonin 5-HT2C, 5-HT1A and 5-HT1D receptors. It has a moderate affinity to neuronal serotonin and norepinephrine transporters, as well as to H1-histamine and alpha1-adrenoceptors (which are associated with the development of somnolence and orthostatic hypotension).
It practically does not interact with m-cholinoreceptors. Antipsychotic activity of the drug is partially caused by blockade of dopaminergic and serotonin receptors. The serotonergic activity of ziprasidone and its effect on neurotransmitter reuptake in neurons are associated with antidepressant activity.
Blockade of 5-HT1A receptors causes anxiolytic effects. Powerful antagonism to 5-HT2C receptors determines antipsychotic activity. The degree of blockade of serotonin 5-HT2A receptors in 12 hours after a single oral dose of 40 mg is 80%, and D2 receptors – 50%.
Indications
Indications
Schizophrenia and similar mental disorders (treatment and prevention of exacerbations).
Active ingredient
Active ingredient
Composition
Composition
Active ingredient:
Ziprasidone hydrochloride monohydrate;
Ancillary substances:
Lactose monohydrate,
Pregelatinized corn starch,
Magnesium stearate;
Capsule body and cap:
Titanium dioxide; indigo carmine (except 60 mg dosage); gelatin
How to take, the dosage
How to take, the dosage
Internal, with meals.
Adults. In treatment of acute schizophrenia and bipolar disorder, the recommended starting dose is 40 mg twice daily. Subsequently, the dose is increased taking into account the clinical condition. The maximum daily dose is 160 mg (80 mg twice daily). If necessary, the daily dose can be increased to the maximum within 3 days. The average therapeutic dose of Zeldox® is 120 mg divided into 2 doses.
The lowest effective dose should be prescribed as maintenance therapy for schizophrenia; in most cases, taking 20 mg of the drug twice daily is sufficient.
There is no need to change the dose in elderly people (65 years and older), patients with impaired renal function, or in patients who smoke.
Interaction
Interaction
The co-administration of ziprasidone and drugs causing prolongation of the QT interval (including antiarrhythmic drugs of classes IA and III) increases the risk of QT interval prolongation and paroxysmal ventricular tachycardia (this combination is contraindicated).
In co-administration of ziprasidone with drugs with CNS depressant effect, mutual enhancement of this effect is possible (this combination requires caution).
Ziprasidone has no inhibitory effect on CYP1A2, CYP2C9 or CYP2C19. In vitro concentrations of ziprasidone causing inhibition of CYP2D6 and CYP3A4 were at least 1000 times higher than concentrations of the drug that would be expected in vivo. This indicates that there is no possibility of a clinically significant interaction between ziprasidone and drugs metabolized by these isoenzymes.
In accordance with the results of in vitro studies and data from clinical trials in healthy volunteers, it was shown that ziprasidone had no CYP2D6-mediated effect on the metabolism of dextromethorphan and its main metabolite dextrophan.
Ziprasidone did not cause significant changes in the pharmacokinetics of estrogen or ethinyl estradiol (a CYP3A4 substrate) or progesterone-containing components when co-administered with oral hormonal contraceptives.
Ziprasidone does not affect the pharmacokinetics of lithium when used together.
Ziprasidone binds significantly to plasma proteins. In in vitro studies, warfarin and propranolol (drugs with high degree of binding to proteins) had no effect on the binding of ziprasidone to plasma proteins, and ziprasidone had no effect on the binding of these drugs to plasma proteins. Thus, the possibility of drug interactions with ziprasidone due to displacement from plasma protein binding seems unlikely.
Ziprasidone is metabolized by aldehydoxidase and, to a lesser extent, by CYP3A4. There are no known clinically relevant inhibitors or inducers of aldehydoxidase.
Co-administration with ketoconazole (400 mg/day) as a potential CYP3A4 inhibitor resulted in an increase of approximately 35% in the AUC and Cmax of ziprasidone, which is hardly clinically relevant.
The co-administration with carbamazepine (200 mg 2 times/day), as a CYP3A4 inducer, in turn resulted in a 36% decrease in the AUC and Cmax of ziprasidone, which is hardly clinically relevant.
When used in combination, cimetidine, a nonspecific isoenzyme inhibitor, had no significant effect on the pharmacokinetics of ziprasidone.
The concomitant use of antacids containing aluminum and magnesium had no effect on the pharmacokinetics of ziprasidone.
In clinical studies, no clinically significant effect of concomitant use of benztropine, propranololol and lorazepam on the pharmacokinetic parameters and serum concentrations of ziprasidone was found.
Contraindications
Contraindications
Side effects
Side effects
CNS and peripheral nervous system disorders: asthenia, headache, extrapyramidal syndrome, insomnia or somnolence, tremor, blurred vision, psychomotor agitation, akathisia, dizziness, dystonic reactions. Seizures were extremely rare (less than 1% of patients receiving ziprasidone). The Movement Disorder Burden Score, which reflects the severity of extrapyramidal symptoms when using ziprasidone, is significantly lower (p
Malignant Neuroleptic Syndrome (MNS): cases of MNS, which is a rare but potentially fatal complication, have been observed when using antipsychotics. Clinical manifestations of MNS are elevated body temperature (hyperpyrexia), muscle rigidity, altered mental status, and autonomic nervous system instability (arrhythmia, BP changes, tachycardia, profuse sweating, heart rhythm disturbances). Additional signs may include elevated CPK levels, myoglobinuria (rhabdomyolysis), and acute renal failure. If symptoms that can be attributed to MNS occur, or if there is a sudden high body temperature that is not accompanied by other symptoms of MNS, all antipsychotics, including ziprasidone, should be stopped immediately.
Cases of MNS have been reported with postmarketing use of Zeldox.
Slow dyskinesia: with long-term use of ziprasidone, as with other antipsychotics, there is a risk of developing slow dyskinesias and other distant extrapyramidal syndromes. If signs of dyskinesia appear, it is advisable to reduce the dose of ziprasidone or discontinue it.
In the digestive system: constipation, dry mouth, dyspepsia, increased salivation, nausea, vomiting.
Others: during maintenance therapy with ziprasidone increased prolactin levels were sometimes observed (normalized in most cases without discontinuation of treatment), arterial hypertension. It was reported about weight fluctuation towards increasing on the average by 0.5 kg with short-term treatment (4-6 weeks) and towards decreasing by 1-3 kg with long-term treatment (within 1 year) compared to patients who did not take this medicine.
Additional information
| Shelf life | 4 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Pfizer, Puerto Rico |
| Medication form | capsules |
| Brand | Pfizer |
Related products
Buy Zeldox, 40 mg capsules 30 pcs with delivery to USA, UK, Europe and over 120 other countries.