No products in the cart.
Xarelto, 15 mg 98 pcs
€315.89 €263.24
Description
Pharmacotherapeutic group: direct factor Xa inhibitors.
ATX code: B01AF01.
Pharmacological properties
Pharmacodynamics
The mechanism of action
p> Rivaroxaban is a highly selective direct factor Xa inhibitor with high bioavailability when taken orally.
The activation of factor X to form factor Xa through the internal and external clotting pathways plays a central role in the coagulation cascade. Factor Xa is a component of the forming prothrombinase complex, the action of which leads to the conversion of prothrombin into thrombin. As a result, these reactions lead to the formation of fibrin thrombus and platelet activation by thrombin. One molecule of factor Xa catalyzes the formation of over 1000 molecules of thrombin, which has been termed the “thrombin burst. The reaction rate of prothrombinase-bound factor Xa increases 300,000 times that of free factor Xa, providing a dramatic jump in thrombin levels. Selective factor Xa inhibitors can stop the thrombin burst. Thus, rivaroxaban affects the results of some specific or general laboratory tests used to evaluate clotting systems.
Pharmacodynamic effects
In humans, there is a dose-dependent inhibition of factor Xa activity. Rivaroxaban has a dose-dependent effect on prothrombin time and correlates well with plasma concentrations (r=0.98) if the Neoplastin kit is used for the assay. Results will differ if other reagents are used. Prothrombin time should be measured in seconds because the INR (international normalized ratio) is calibrated and certified only for coumarin derivatives and cannot be used for other anticoagulants.
In patients with non-valvular atrial fibrillation taking rivaroxaban for prevention of stroke and systemic thromboembolism, the 5/95 percentile for prothrombin time (Neoplastin) 1-4 hours after taking the tablet (ie.i.e., at maximum effect) range from 14 to 40 seconds in patients taking 20 mg once daily and from 10 to 50 seconds in patients with moderate renal impairment taking 15 mg once daily.
In patients receiving rivaroxaban for the treatment and prevention of recurrent deep vein thrombosis (DVT) and pulmonary embolism (TELA), 5/95 percentiles for prothrombin time (Neoplastin) 2 to 4 hours after taking the tablet (ie.i.e., at maximum effect) range from 17 to 32 seconds in patients taking 15 mg twice daily and from 15 to 30 seconds in patients taking 20 mg once daily.
Rivaroxaban also dose-dependently increases activated partial thromboplastin time (APT) and the HepTest® result; however, these parameters are not recommended for evaluating the pharmacodynamic effects of rivaroxaban. Also, if clinically warranted, rivaroxaban concentrations may be measured using a calibrated quantitative anti-factor Xa test.
Monitoring of clotting parameters is not required during treatment with Xarelto®.
In healthy men and women over 50 years of age, no prolongation of the electrocardiogram QT interval was observed under the influence of rivaroxaban.
Pharmacokinetics
Intake and bioavailability
Rivaroxaban is rapidly absorbed; maximum concentration (Cmax) is reached 2 to 4 hours after tablet administration.
The absolute bioavailability of rivaroxaban after a dose of 10 mg is high (80-100%) regardless of food intake. No change in AUC (area under the curve “concentration – time”) and Cmax (maximum concentration) was observed when rivaroxaban 10 mg was taken with food.
Due to the reduced degree of absorption, a bioavailability of 66% was observed when 20 mg was taken on an empty stomach. When Xarelto® 20 mg was taken with meals, there was a 39% increase in mean AUC compared to fasting intake, showing almost complete absorption and high bioavailability. Xarelto® 20 mg, 15 mg should be taken with meals.
The pharmacokinetics of rivaroxaban are characterized by moderate individual variability; individual variability (coefficient of variation) is 30% to 40%.
The absorption of rivaroxaban depends on the site of release in the gastrointestinal tract (GIT). A 29% and 56% reduction in AUC and Cmax, respectively, compared to whole tablet administration was observed when rivaroxaban pellet was administered to the proximal small intestine. Exposure to the drug is also reduced when administered into the distal small intestine or the ascending colon. Administration of rivaroxaban in the gastrointestinal tract distal to the stomach should be avoided as it may reduce absorption and therefore exposure to the drug.
The bioavailability (AUC and Cmax) of rivaroxaban 20 mg when taken as a whole tablet is comparable to the bioavailability of the drug taken orally as a crushed tablet (mixed with apple puree or suspended in water) and the bioavailability of the drug when administered via gastric tube followed by liquid food. Given the predictable dose-dependent pharmacokinetic profile of rivaroxaban, the results of this bioavailability study are also applicable to lower doses.
Distribution
In humans, most of rivaroxaban (92-95%) is bound to plasma proteins, with serum albumin being the major binding component. The volume of distribution is moderate, Vss is approximately 50 liters.
Metabolism and excretion
On oral administration, approximately 2/3 of the administered dose of rivaroxaban is metabolized and subsequently excreted in equal amounts in the urine and through the intestine. The remaining 1/3 of the dose is excreted via direct renal excretion unchanged primarily through active renal secretion.
Rivaroxaban is metabolized by CYP3A4, CYP2J2 isoenzymes as well as by mechanisms independent of the cytochrome system. The main sites of biotransformation are oxidation of the morpholine group and hydrolysis of the amide bonds. According to in vitro data, rivaroxaban is a substrate for P-gp (P-glycoprotein) and Bcrp (breast cancer resistance protein) transporter proteins. Unchanged rivaroxaban is the only active compound in human plasma; no major or active circulating metabolites have been detected in plasma. Rivaroxaban, which has a systemic clearance of approximately 10 L/h, may be classified as a low clearance drug. In the plasma excretion of rivaroxaban, the final elimination half-life is 5 to 9 hours in young patients and 11 to 13 hours in elderly patients.
Gender/Elderly (>65 years)
The plasma concentrations of rivaroxaban are higher in elderly patients than in younger patients; the average AUC is approximately 1.5 times greater than in younger patients, primarily due to the apparent decrease in total and renal clearance (see section “Dosage and administration”).
There are no clinically significant differences in pharmacokinetics between men and women (see section “Dosage and administration”).
Body weight
High or low body weight (less than 50 kg and greater than 120 kg) only slightly affects the plasma concentration of rivaroxaban (less than 25% difference) (see section “Administration and Dosages”).
Child and adolescent age (from birth to 18 years)
There are no data for this age group (see section on Dosage and administration).
Interethnic differences
There were no clinically significant differences in pharmacokinetics and pharmacodynamics in patients of Caucasian, African American, Hispanic, Japanese, or Chinese ethnicity (see section on Dosage and administration).
Patients with hepatic impairment
The effect of hepatic impairment on the pharmacokinetics of rivaroxaban has been studied in patients allocated according to the Child-Pugh classification (according to standard procedures in clinical trials). The Child-Pugh classification provides an assessment of the prognosis of chronic liver disease, mainly cirrhosis. In patients scheduled for anticoagulant therapy, the most important consequence of impaired liver function is reduced synthesis of blood clotting factors in the liver. Because this figure corresponds to only one of the five clinical/biochemical criteria that make up the Child-Pugh classification, the risk of bleeding does not correlate clearly with this classification. Treatment of such patients with anticoagulants should be considered regardless of the Child-Pugh classification.
Rivaroxaban is contraindicated in patients with liver disease presenting with coagulopathy that is clinically significant bleeding risk.
In patients with cirrhosis and mild hepatic impairment (Child-Pugh class A) the pharmacokinetics of rivaroxaban did not significantly differ from those of control group of healthy subjects (on the average there was 1.2-fold increase of AUC of rivaroxaban). There were no significant differences in pharmacodynamic properties between the groups.
In patients with cirrhosis and moderate hepatic impairment (Child-Pugh class B) the mean AUC of rivaroxaban was significantly increased (2.3-fold) compared to healthy volunteers due to significantly decreased clearance of the drug substance, indicating serious liver disease. Suppression of factor Xa activity was more pronounced (2.6-fold) than in healthy volunteers. Prothrombin time was also 2.1 times that of healthy volunteers. Prothrombin time measurement assesses the external coagulation pathway, which includes clotting factors VII, X, V, II and I, which are synthesized in the liver. Patients with moderate hepatic insufficiency are more sensitive to rivaroxaban, which is a consequence of a closer relationship between pharmacodynamic effects and pharmacokinetic parameters, especially between concentration and prothrombin time.
There are no data for patients with Child-Pugh class C hepatic impairment (see sections “Dosage and administration” and “Contraindications”).
Patients with impaired renal function
In patients with impaired renal function, there was an increase in the area under the concentration-time curve of rivaroxaban inversely proportional to the degree of decrease in renal function as assessed by creatinine clearance.
. Patients with mild renal impairment (creatinine clearance 50-80 mL/min), moderate renal impairment (CLKR 30-49 mL/min), and severe renal impairment (CLKR 15-29 mL/min) showed 1.4-, 1.5-, and 1.6-fold increases in rivaroxaban plasma concentrations (AUC) compared to healthy volunteers, respectively(see Dosage and Administration, Caution, and Special Precautions).
The corresponding increase in pharmacodynamic effects was more pronounced. In patients with CLKR 50-80 ml/min, CLKR 30-49 ml/min, and CLKR 15-29 ml/min, total suppression of factor Xa activity was increased 1.5, 1.9, and 2-fold compared with healthy volunteers; prothrombin time due to factor Xa activity was also increased 1.3, 2.2, and 2.4-fold, respectively.
The data on the use of Xarelto® in patients with CLR 15-29 ml/min are limited, and therefore caution should be exercised when using the drug in this category of patients. There are no data on the use of Xarelto® in patients with CLR < 15 ml/min, therefore it is not recommended to use the drug in this category of patients.
Due to the underlying disease, patients with severe renal dysfunction are at high risk of bleeding and thrombosis.
Patients with acute deep vein thrombosis (DVT)
. In patients receiving rivaroxaban at a dose of 20 mg once daily for treatment of acute deep vein thrombosis (DVT), the geometric mean value of maximum concentration 2-4 hours after drug administration was 215 mcg/L (22-535 mcg/L); the geometric mean value of the minimum concentration 24 hours after the drug intake was 32 mcg/L (6-239 mcg/L). Prediction interval = 90%
Ratio of pharmacokinetic parameters and pharmacodynamic effects The ratio of pharmacokinetic parameters and pharmacodynamic effects (PK/PD) between the plasma concentration of rivaroxaban and the pharmacodynamic endpoints was assessed with the administration of rivaroxaban at doses of 5 to 30 mg twice daily <
(Factor Xa inhibition, prothrombin time, activated partial thromboplastin time (APTV) and HepTest® results).
The relationship between rivaroxaban concentration and factor Xa activity is best demonstrated using the Emax model.
The linear slope model demonstrates the relationship between rivaroxaban concentration and prothrombin time value. The slope angle varied significantly depending on the reagents used to determine the prothrombin time. Using the Neoplastin kit, the baseline prothrombin time was about 13 s with a slope of about 3-4 s (100 µg/L). The results of the FK/FD ratio analysis in the phase II and III studies were similar to those of healthy patients.
Indications
Indications
prevention of stroke and systemic thromboembolism in patients with non-valvular atrial fibrillation;
treatment of deep vein thrombosis and pulmonary embolism and prevention of relapses of DVT and PE.
Pharmacological effect
Pharmacological effect
PHARMACOTHERAPEUTIC GROUP: direct factor Xa inhibitors.
ATX code: В01AF01.
PHARMACOLOGICAL PROPERTIES
Pharmacodynamics
Mechanism of action
Rivaroxaban is a highly selective direct factor Xa inhibitor with high oral bioavailability.
Activation of factor X to form factor Xa through the intrinsic and extrinsic coagulation pathways plays a central role in the coagulation cascade. Factor Xa is a component of the developing prothrombinase complex, the action of which leads to the conversion of prothrombin to thrombin. As a result, these reactions lead to the formation of a fibrin thrombus and activation of platelets by thrombin. One molecule of factor Xa catalyzes the formation of more than 1000 molecules of thrombin, which is called the “thrombin burst”. The rate of reaction of factor Xa bound in prothrombinase is increased 300,000 times compared to that of free factor Xa, which provides a sharp jump in thrombin levels. Selective factor Xa inhibitors can stop the thrombin burst. Therefore, rivaroxaban may interfere with the results of some specific or general laboratory tests used to evaluate coagulation systems.
Pharmacodynamic effects
In humans, dose-dependent inhibition of factor Xa activity is observed. Rivaroxaban has a dose-dependent effect on prothrombin time and correlates well with plasma concentrations (r=0.98) when the Neoplastin kit is used for analysis. Results will vary if other reagents are used. Prothrombin time should be measured in seconds because the INR (International Normalized Ratio) is calibrated and certified only for coumarin derivatives and cannot be used for other anticoagulants.
In patients with nonvalvular atrial fibrillation taking rivaroxaban for the prevention of stroke and systemic thromboembolism, the 5/95 percentile for prothrombin time (Neoplastin) 1 to 4 hours after tablet dosing (i.e., at maximum effect) ranges from 14 to 40 seconds in patients taking 20 mg once daily and from 10 to 50 seconds in patients taking 20 mg once daily. with moderate renal impairment taking 15 mg once daily.
In patients receiving rivaroxaban for the treatment and prevention of recurrent deep vein thrombosis (DVT) and pulmonary embolism (PE), the 5/95 percentile for prothrombin time (Neoplastin) 2 to 4 hours after tablet dosing (i.e., at maximum effect) ranges from 17 to 32 seconds in patients taking 15 mg twice daily and from 15 to 30 seconds in patients taking 20 mg once daily.
Also, rivaroxaban dose-dependently increases activated partial thromboplastin time (aPTT) and HepTest® result; however, these parameters are not recommended for assessing the pharmacodynamic effects of rivaroxaban. Also, if clinically warranted, rivaroxaban concentrations can be measured using a calibrated quantitative anti-factor Xa test.
During treatment with Xarelto®, monitoring of blood coagulation parameters is not required.
In healthy men and women over 50 years of age, prolongation of the electrocardiogram QT interval under the influence of rivaroxaban was not observed.
Pharmacokinetics
Absorption and bioavailability
Rivaroxaban is rapidly absorbed; the maximum concentration (Cmax) is achieved 2-4 hours after taking the tablet.
The absolute bioavailability of rivaroxaban after a 10 mg dose is high (80-100%), regardless of food intake. When taking rivaroxaban at a dose of 10 mg with food, there was no change in AUC (area under the concentration-time curve) and Cmax (maximum concentration).
Due to the reduced degree of absorption, a bioavailability of 66% was observed when taking 20 mg on an empty stomach. When Xarelto® 20 mg was taken with food, there was a 39% increase in mean AUC compared to fasting, indicating almost complete absorption and high bioavailability. Xarelto® 20 mg, 15 mg should be taken with food.
The pharmacokinetics of rivaroxaban is characterized by moderate individual variability; individual variability (variation coefficient) ranges from 30 to 40%.
The absorption of rivaroxaban depends on the site of release in the gastrointestinal (GI) tract. Reductions of 29% and 56% in AUC and Cmax, respectively, compared to whole tablet administration were observed when rivaroxaban granulate was administered into the proximal small intestine. Drug exposure is also reduced when administered into the distal small intestine or ascending colon. Administration of rivaroxaban into the gastrointestinal tract distal to the stomach should be avoided as this may result in decreased absorption and, consequently, decreased exposure of the drug.
The bioavailability (AUC and Cmax) of rivaroxaban 20 mg when taken as a whole tablet is comparable to the bioavailability of the drug taken orally as a crushed tablet (mixed with applesauce or suspended in water), as well as the bioavailability of the drug when administered through a gastric tube followed by a liquid diet. Given the predictable dose-dependent pharmacokinetic profile of rivaroxaban, the results of this bioavailability study also apply to lower doses.
Distribution
In the human body, most of rivaroxaban (92-95%) is bound to plasma proteins, the main binding component being serum albumin. The volume of distribution is moderate, Vss is approximately 50 l.
Metabolism and excretion
When taken orally, approximately 2/3 of the prescribed dose of rivaroxaban is metabolized and subsequently excreted in equal parts through the urine and intestines. The remaining 1/3 of the dose is eliminated unchanged by direct renal excretion, mainly due to active renal secretion.
Rivaroxaban is metabolized through isoenzymes CYP3A4, CYP2J2, as well as through mechanisms independent of the cytochrome system. The main sites of biotransformation are the oxidation of the morpholine group and the hydrolysis of amide bonds. According to in vitro data, rivaroxaban is a substrate for the transporter proteins P-gp (P-glycoprotein) and Bcrp (breast cancer resistance protein). Unchanged rivaroxaban is the only active compound in human plasma, and no major or active circulating metabolites have been detected in plasma. Rivaroxaban, whose systemic clearance is approximately 10 L/h, can be classified as a drug with low clearance. When rivaroxaban is eliminated from plasma, the terminal half-life is 5 to 9 hours in younger patients and 11 to 13 hours in older patients.
Gender/Old age (over 65 years old)
In elderly patients, plasma concentrations of rivaroxaban are higher than in younger patients; the average AUC value is approximately 1.5 times higher than the corresponding values in young patients, mainly due to an apparent decrease in total and renal clearance (see section “Dosage and Administration”).
No clinically significant differences in pharmacokinetics were found in men and women (see section “Dosage and Administration”).
Body weight
Too little or too much body weight (less than 50 kg and more than 120 kg) only slightly affects the concentration of rivaroxaban in the blood plasma (the difference is less than 25%) (see section “Dosage and Administration”).
Childhood and adolescence (from birth to 18 years)
There are no data for this age category (see section “Dosage and Administration”).
Interethnic differences
There were no clinically significant differences in pharmacokinetics and pharmacodynamics in patients of Caucasian, African American, Hispanic, Japanese or Chinese ethnicity (see section “Dosage and Administration”).
Patients with liver dysfunction
The effect of hepatic impairment on the pharmacokinetics of rivaroxaban was studied in patients allocated according to the Child-Pugh classification (according to standard procedures in clinical trials). The Child-Pugh classification allows you to assess the prognosis of chronic liver diseases, mainly cirrhosis. In patients undergoing anticoagulant therapy, the most important consequence of impaired liver function is a decrease in the synthesis of coagulation factors in the liver. Since this indicator corresponds to only one of the five clinical/biochemical criteria that make up the Child-Pugh classification, the risk of bleeding does not clearly correlate with this classification. The question of treating such patients with anticoagulants should be decided regardless of the Child-Pugh class.
Rivaroxaban is contraindicated in patients with liver disease associated with coagulopathy causing a clinically significant risk of bleeding.
In patients with liver cirrhosis and mild liver failure (Child-Pugh class A), the pharmacokinetics of rivaroxaban differed only slightly from the corresponding indicators in the control group of healthy subjects (on average, there was an increase in the AUC of rivaroxaban by 1.2 times). There were no significant differences in pharmacodynamic properties between groups.
In patients with cirrhosis and moderate hepatic impairment (Child-Pugh class B), the mean AUC of rivaroxaban was significantly increased (2.3-fold) compared to healthy volunteers due to significantly reduced drug clearance, indicating significant liver disease. The suppression of factor Xa activity was more pronounced (2.6 times) than in healthy volunteers. Prothrombin time was also 2.1 times higher than in healthy volunteers. By measuring prothrombin time, the extrinsic coagulation pathway is assessed, including coagulation factors VII, X, V, II and I, which are synthesized in the liver. Patients with moderate hepatic impairment are more sensitive to rivaroxaban, which is a consequence of a closer relationship between pharmacodynamic effects and pharmacokinetic parameters, especially between concentration and prothrombin time.
There are no data on patients with hepatic insufficiency class C according to the Child-Pugh classification (see sections “Method of administration and dosage”, “Contraindications”).
Patients with impaired renal function
In patients with impaired renal function, an increase in the area under the concentration-time curve of rivaroxaban was observed, inversely proportional to the degree of decrease in renal function, as assessed by creatinine clearance.
In patients with mild renal impairment (creatinine clearance 50-80 ml/min), moderate renal impairment (CrCl 30-49 ml/min) and severe renal impairment (CrCl 15-29 ml/min), 1.4-, 1.5- and 1.6-fold increases in rivaroxaban plasma concentrations (AUC) were observed, respectively, compared with healthy controls. volunteers (see sections “Method of administration and dosage”, “With caution”, “Special instructions”).
The corresponding increase in pharmacodynamic effects was more pronounced. In patients with ClCr 50-80 ml/min, ClCr 30-49 ml/min and ClCr 15-29 ml/min, the overall suppression of factor Xa activity increased by 1.5, 1.9 and 2 times compared with healthy volunteers; prothrombin time due to the action of factor Xa also increased by 1.3, 2.2 and 2.4 times, respectively.
Data on the use of Xarelto® in patients with CrCl 15-29 ml/min are limited, and therefore caution should be exercised when using the drug in this category of patients. There are no data on the use of Xarelto® in patients with ClCr < 15 ml/min, and therefore it is not recommended to use the drug in this category of patients.
Due to the underlying disease, patients with severe renal impairment are at high risk of bleeding and thrombosis.
Patients with acute deep vein thrombosis (DVT)
In patients receiving rivaroxaban 20 mg for the treatment of acute deep vein thrombosis (DVT) once daily, the geometric mean maximum concentration 2-4 hours after dosing was 215 μg/L (22-535 μg/L); the geometric mean minimum concentration 24 hours after dosing was 32 µg/l (6-239 µg/l). Prediction interval = 90%
Ratio of pharmacokinetic parameters and pharmacodynamic effects When taking rivaroxaban at a dose of 5 to 30 mg twice daily, the ratio of pharmacokinetic parameters and pharmacodynamic effects (PK/PD) between the concentration of rivaroxaban in the blood plasma and pharmacodynamic end points was assessed.
(factor Xa inhibition, prothrombin time, activated partial thromboplastin time (aPTT) and HepTest® result).
The relationship between rivaroxaban concentration and factor Xa activity is best demonstrated using the Emax model.
The linear intercept model demonstrates the relationship between rivaroxaban concentration and prothrombin time. The slope angle varied significantly depending on the reagents used to determine prothrombin time. Using the Neoplastin kit, the baseline prothrombin time was about 13 seconds with a slope of about 3-4 seconds (100 μg/L). The results of the analysis of the PK/PD ratio in phase II and III studies corresponded to those in healthy patients.
Special instructions
Special instructions
Use of concomitant medications
The use of rivaroxaban is not recommended in patients receiving concomitant systemic treatment with azole antifungals (eg, ketoconazole) or HIV protease inhibitors (eg, ritonavir). These drugs are potent inhibitors of CYP3A4 and P-glycoprotein. Thus, these drugs may increase the plasma concentration of rivaroxaban to clinically significant levels (2.6-fold on average), which may lead to an increased risk of bleeding (see sections “Precautions”, “Interaction with other drugs”).
However, the azole antifungal drug fluconazole, a moderate inhibitor of CYP3A4, has a less pronounced effect on the exposure of rivaroxaban and can be used concomitantly with it (see section “Interactions with other medicinal products”).
Renal dysfunction
Rivaroxaban should be used with caution in patients with moderate renal impairment (CrCl 30-49 ml/min) receiving concomitant medications that may lead to increased plasma concentrations of rivaroxaban (see sections
“With caution”, “Interaction with other drugs”).
In patients with severe renal impairment (CrCl < 30 ml/min), plasma concentrations of rivaroxaban may be significantly increased (1.6-fold on average), which may lead to an increased risk of bleeding. Therefore, due to the presence of this underlying disease, such patients have an increased risk of developing both bleeding and thrombosis. Due to limited clinical data, rivaroxaban should be used with caution in patients with CrCl 15-29 ml/min.
There are no clinical data on the use of rivaroxaban in patients with severe renal impairment (CrCl < 15 ml/min). Therefore, the use of Xarelto® is not recommended in such patients (see sections “Contraindications”, “Dosage and Administration”, “Pharmacological Properties”).
Patients with severe renal impairment (CrCl 15-29 ml/min), an increased risk of bleeding, and patients receiving concomitant systemic treatment with azole antifungals or HIV protease inhibitors should be closely monitored for signs of bleeding after initiation of treatment.
Risk of bleeding
As with other anticoagulants, patients taking Xarelto should be carefully monitored for signs of bleeding.
In case of severe bleeding, Xarelto® should be discontinued.
In clinical studies, mucocutaneous bleeding (namely, bleeding from the nose, gums, gastrointestinal tract, genitourinary system, including abnormal vaginal or increased menstrual bleeding) and anemia were observed more often with long-term treatment with rivaroxaban compared with VKA treatment. Thus, in addition to proper clinical monitoring, laboratory testing of hemoglobin/hematocrit may be useful in identifying occult bleeding and quantifying the clinical significance of overt bleeding that would be considered acceptable.
Xarelto®, like other antithrombotic agents, should be used with caution in patients at increased risk of bleeding, including:
patients with a congenital or acquired tendency to bleeding;
patients with uncontrolled severe arterial hypertension;
patients with gastric and duodenal ulcers in the acute stage;
patients who have recently suffered from gastric and duodenal ulcers;
patients with vascular retinopathy;
patients who have recently suffered intracranial or intracerebral hemorrhage;
patients with pathology of the blood vessels of the brain or spinal cord;
patients who have recently undergone surgery on the brain, spinal cord, or eyes;
patients with a history of bronchiectasis or pulmonary hemorrhage.
Caution should be exercised if the patient is concomitantly receiving medications that affect hemostasis, such as non-steroidal anti-inflammatory drugs (NSAIDs), platelet aggregation inhibitors, other antithrombotic drugs or selective serotonin reuptake inhibitors (SSRIs) and selective serotonin norepinephrine reuptake inhibitors (SNRIs) (see section “Interactions with other drugs”).
In patients at risk of developing gastric and duodenal ulcers, appropriate preventive treatment can be prescribed.
If there is an unexplained decrease in hemoglobin or blood pressure, it is necessary to look for the source of bleeding.
Rivaroxaban therapy does not require routine monitoring of its exposure. However, measuring rivaroxaban concentrations using a calibrated test to quantify anti-Xa activity may be useful in exceptional cases where information about rivaroxaban exposure can be used to make clinically relevant decisions, such as in cases of overdose or emergency surgery.
Patients with artificial heart valves
Based on data from a randomized controlled clinical trial comparing Xarelto® therapy with antiplatelet therapy, the use of Xarelto® is not recommended for the prevention of thrombosis in patients who have undergone recent transcatheter aortic valve replacement. The safety and effectiveness of Xarelto® have not been studied in patients with any other prosthetic heart valves or in patients undergoing other heart valve interventions; therefore, there is no data to support that Xarelto® 20 mg (15 mg in patients with moderate to severe renal impairment with CrCl 15-49 ml/min) provides a sufficient anticoagulant effect in these categories of patients.
Patients at high risk of triple-positive antiphospholipid syndrome The use of Xarelto is not recommended in patients with a history of thrombosis who have been diagnosed with persistent triple-positive antiphospholipid syndrome (presence of lupus anticoagulant, antibodies to cardiolipin and antibodies to beta-2-glycoprotein I), since therapy with rivaroxaban is accompanied by an increased incidence of recurrent thrombotic events compared with therapy with antagonists vitamin K (VKA).
Patients with non-valvular atrial fibrillation who underwent PCI with stenting
There are data from an international clinical study, the primary purpose of which was to assess safety in patients with non-valvular atrial fibrillation who underwent PCI with stenting. Data on efficacy in this population are limited (see section “Dosage and Administration”). There are no data available for such patients with a history of stroke/transient ischemic attack.
Patients with hemodynamically unstable pulmonary embolism (PE) and patients requiring thrombolysis or thrombectomy
Rivaroxaban is not recommended as an alternative to unfractionated heparin in patients with hemodynamically unstable pulmonary embolism, or in patients who may require thrombolysis or thrombectomy, as the safety and effectiveness of Xarelto in these clinical situations has not been established.
Surgical operations and interventions
If an invasive procedure or surgery is necessary, Xarelto® should be discontinued at least 24 hours before the procedure and as determined by your physician.
If the procedure cannot be delayed, the increased risk of bleeding should be weighed against the need for urgent intervention.
Xarelto® should be restarted after an invasive procedure or surgery, provided that appropriate clinical indicators and adequate hemostasis are present (see section “Pharmacological properties”).
Spinal anesthesia
When performing epidural/spinal anesthesia or spinal puncture in patients receiving platelet aggregation inhibitors to prevent thromboembolic complications, there is a risk of developing an epidural or spinal hematoma, which can lead to long-term paralysis. The risk of these events is further increased by the use of an indwelling epidural catheter or concomitant therapy with drugs that affect hemostasis. Traumatic epidural or spinal puncture or repeated puncture may also increase the risk.
Patients should be monitored for signs and symptoms of neurological impairment (eg, numbness or weakness of the legs, bowel or bladder dysfunction). If neurological disorders are detected, urgent diagnosis and treatment are necessary.
The physician should weigh the potential benefit against the relative risk before performing spinal surgery in patients receiving anticoagulants or who are scheduled to receive anticoagulants for the purpose of preventing thrombosis. There is no experience with the clinical use of rivaroxaban in dosages of 15 mg and 20 mg in the described situations.
To reduce the potential risk of bleeding associated with concomitant use of rivaroxaban and epidural/spinal anesthesia or spinal puncture, the pharmacokinetic profile of rivaroxaban should be considered. Insertion or removal of an epidural catheter or lumbar puncture is best performed when the anticoagulant effect of rivaroxaban is assessed as weak.
However, the exact time to achieve a sufficiently low anticoagulant effect in each patient is unknown.
Based on general pharmacokinetic characteristics, the epidural catheter is removed after at least twice the half-life has elapsed, i.e. no earlier than 18 hours after the last dose of Xarelto® for young patients and no earlier than 26 hours for older patients. Xarelto® should be prescribed no earlier than 6 hours after removal of the epidural catheter.
In the event of a traumatic puncture, the administration of Xarelto® should be postponed for 24 hours.
Skin reactions
Cases of Stevens-Johnson syndrome and toxic epidermal necrolysis have been reported during post-marketing surveillance. At the first appearance of severe skin rash (for example, if it spreads, intensifies and/or blisters) or if there are other symptoms of hypersensitivity associated with damage to the mucous membrane, Xarelto® therapy should be discontinued.
Women of reproductive age
Xarelto® should only be used by women of childbearing age if they are using effective contraception.
Corrected QT interval prolongation
There was no effect of Xarelto® on the duration of the QT interval.
Safety data obtained from nonclinical studies
With the exception of effects associated with enhanced pharmacological action (bleeding), analysis of preclinical data obtained in pharmacological safety studies did not reveal any specific hazard to humans.
INFLUENCE ON THE ABILITY TO DRIVE VEHICLES AND MECHANISMS
While taking the drug, fainting and dizziness have been observed, which may affect the ability to drive vehicles or operate other machinery (see section “Side Effects”). Patients who experience such adverse reactions should not drive vehicles or operate machinery.
Active ingredient
Active ingredient
Rivaroxaban
Composition
Composition
One film-coated tablet contains:
active ingredient:
rivaroxaban micronized 15.00 mg;
excipients:
microcrystalline cellulose – 37.50 mg,
croscarmellose sodium – 3.00 mg,
hypromellose 5cP (hydroxypropyl methylcellulose 2910) – 3.00 mg,
lactose monohydrate – 25.40 mg,
magnesium stearate – 0.60 mg,
sodium lauryl sulfate – 0.50 mg;
shell: red iron oxide dye – 0.15 mg, hypromellose 15cP (hydroxypropyl methylcellulose 2910) – 1.50 mg, macrogol 3350 (polyethylene glycol (3350)) – 0.50 mg, titanium dioxide – 0.35 mg.
Pregnancy
Pregnancy
Pregnancy
The safety and effectiveness of rivaroxaban in pregnant women have not been established. Data obtained in experimental animals have shown pronounced maternal toxicity of rivaroxaban, associated with the pharmacological action of the drug (for example, complications in the form of hemorrhages) and leading to reproductive toxicity. No primary teratogenic potential was detected.
Due to the possible risk of bleeding and the ability to cross the placenta, rivaroxaban is contraindicated during pregnancy (see section “Contraindications”).
Women with preserved reproductive capacity should use effective methods of contraception during treatment with Xarelto®.
Breast-feeding
There are no data on the use of rivaroxaban for the treatment of women during breastfeeding. Data obtained in experimental animals show that rivaroxaban is excreted in breast milk. Xarelto® can be used only after breastfeeding has been stopped (see section “Contraindications”).
Fertility
Studies have shown that rivaroxaban does not affect male or female fertility in rats. There are no human studies of the effects of rivaroxaban on fertility.
Contraindications
Contraindications
hypersensitivity to rivaroxaban or any excipients contained in the tablet;
clinically significant active bleeding (eg, intracranial hemorrhage, gastrointestinal bleeding);
injury or condition associated with an increased risk of major bleeding, such as a current or recent gastrointestinal ulcer, the presence of malignant tumors with a high risk of bleeding, recent trauma to the brain or spinal cord, surgery on the brain, spinal cord or eyes, intracranial hemorrhage, diagnosed or suspected esophageal varices, arteriovenous malformations, vascular aneurysms or vascular pathology of the brain or spinal cord;
concomitant therapy with any other anticoagulants, for example, unfractionated heparin, low molecular weight heparins (enoxaparin, dalteparin, etc.), heparin derivatives (fondaparinux, etc.), oral anticoagulants (warfarin, apixaban, dabigatran, etc.), except in cases of switching from or to rivaroxaban (see section “Dosage and Administration”) or when using unfractionated heparin in doses necessary to ensure the functioning of a central venous or arterial catheter;
liver diseases occurring with coagulopathy, which causes a clinically significant risk of bleeding (see section “Pharmacological properties”);
pregnancy and breastfeeding (see section “Use during pregnancy and breastfeeding”);
children and adolescents up to 18 years of age (efficacy and safety in patients of this age group have not been established);
severe renal impairment (CrCl < 15 ml/min) (there are no clinical data on the use of rivaroxaban in this category of patients);
congenital lactase deficiency, lactose intolerance, glucose-galactose malabsorption (due to the presence of lactose in the composition).
WITH CAUTION
The drug should be used with caution:
When treating patients with an increased risk of bleeding (including congenital or acquired tendency to bleeding, uncontrolled severe arterial hypertension, gastric and duodenal ulcers in the acute stage, recent gastric and duodenal ulcers, vascular retinopathy, bronchiectasis or a history of pulmonary hemorrhage);
In the treatment of patients with moderate renal impairment (CrCl 30-49 ml/min) who are simultaneously receiving drugs that increase the concentration of rivaroxaban in the blood plasma (see section “Interaction with other drugs”);
When treating patients with severe renal impairment (ClCr 15-29 ml/min) (see section “Special Instructions);
In patients receiving concomitant medications that affect hemostasis, such as nonsteroidal anti-inflammatory drugs (NSAIDs), antiplatelet agents, other antithrombotics or selective serotonin reuptake inhibitors (SSRIs) and selective serotonin norepinephrine reuptake inhibitors (SNRIs).
Rivaroxaban is not recommended for use in patients receiving systemic treatment with azole antifungals (for example, ketoconazole) or HIV protease inhibitors (for example, ritonavir) (see sections “Interactions with other drugs”, “Special instructions”).
Patients with severe renal impairment (CrCl 15-29 ml/min), an increased risk of bleeding, and patients receiving concomitant systemic treatment with azole antifungals or HIV protease inhibitors should be closely monitored after initiation of treatment for timely detection of complications in the form of bleeding.
Side Effects
Side Effects
The safety of Xarelto® was assessed in thirteen phase III studies involving 53,103 patients treated with Xarelto®.
The number of patients enrolled in the study who received at least 1 dose of rivaroxaban, the total daily dose and the maximum duration of treatment in the phase III clinical studies using Xarelto® are shown in Table 2 below:
Table 2.
Therapeutic area
Number
patients*
Total daily dose
Maximum duration of treatment
Prevention of venous thromboembolism (VTE) in patients undergoing elective hip or knee replacement surgery
6,097
10 mg
39 days
Prevention of venous thromboembolism in patients hospitalized for medical reasons
3,997
10 mg
39 days
Treatment of DVT, PE and prevention of recurrence of DVT, PE
6,790
Day 1 – 21: 30 mg
From day 22: 20 mg
After at least 6 months of therapy: 10 mg or 20 mg
21 months
Prevention of stroke and systemic thromboembolism in patients with non-valvular atrial fibrillation
7 750
20 mg
41 months
Prevention of atherothrombic complications in patients after acute coronary syndrome (ACS)
10 225
5 mg or 10 mg, respectively, in combination with acetylsalicylic acid or acetylsalicylic acid with clopidogrel or ticlopidine
31 months
Prevention of stroke, myocardial infarction and death due to cardiovascular causes, as well as for the prevention of acute limb ischemia and all-cause mortality in patients with coronary heart disease (CHD) or PAD
18244
5 mg in combination with acetylsalicylic acid 100 mg or 10 mg in monotherapy
47 months
*Patients who have received at least one dose of rivaroxaban.
Incidence of bleeding and anemia in patients treated with Xarelto® in phase III clinical studies:
Table 3.
Indications for use
Number of patients
Any bleeding
Anemia
Prevention of venous thromboembolism (VTE) in patients undergoing elective replacement surgery
6.8%
5.9%
hip or knee joint
Prevention of venous thromboembolism in patients hospitalized for medical reasons
12.6%
2.1%
Treatment of DVT, PE and prevention of recurrence of DVT, PE
23%
1.6%
Prevention of stroke and systemic thromboembolism in patients with non-valvular atrial fibrillation
28 events
per 100 patient-years
2.5 events
per 100 patient-years
Prevention of atherothrombotic complications in patients after acute coronary syndrome (ACS)
22 events
per 100 patient-years
1.4 events
per 100 patient-years
Prevention of stroke, myocardial infarction and death due to cardiovascular causes, as well as for the prevention of acute limb ischemia and all-cause mortality in patients with coronary artery disease or PAD
6.7 events
per 100 patient-years
0.15 events
per 100 patient-years*
* When collecting data on adverse events, a prespecified sampling approach was used. Given the mechanism of action, the use of Xarelto® may be accompanied by an increased risk of hidden or overt bleeding from any organs and tissues, which can lead to post-hemorrhagic anemia. The risk of bleeding may increase in patients with uncontrolled arterial hypertension and/or when used together with drugs that affect hemostasis (see section “Precautions”). Signs, symptoms and severity (including possible death) vary depending on the location, intensity or duration of bleeding and/or anemia (see Overdose section). Hemorrhagic complications may include weakness, pallor, dizziness, headache, or unexplained swelling, shortness of breath, or shock that cannot be explained by other causes. In some cases, symptoms of myocardial ischemia, such as chest pain and angina, developed as a result of anemia.
Known complications secondary to severe bleeding, such as increased subfascial pressure syndrome (compartment syndrome) and renal failure due to hypoperfusion, have also been reported with the use of Xarelto®. Therefore, the possibility of bleeding should be considered when assessing any patient receiving anticoagulants.
The incidence of ADRs (adverse drug reactions) when using Xarelto® is shown in the table below. Within each frequency group, adverse events are presented in order of decreasing severity.
Frequency of occurrence is defined as:
very often (≥1/10),
often: (from ≥1/100 to <1/10), infrequently: (from ≥1/1,000 to <1/100), rarely: (from ≥1/10,000 to <1/1,000),
Table 4: All treatment-emergent adverse drug reactions recorded in patients in phase III clinical trials (cumulative data RECORD 1-4, ROCKET AF, J-ROCKET, MAGELLAN, ATLAS
and EINSTEIN (DVT/PE/Extension CHOICE) and COMPASS*)
Systemic organ class (MedDRA –
Medical dictionary of regulatory and legal vocabulary
version 20.0)
Often
Uncommon
Rarely
Blood and lymphatic system disorders
Anemia (including relevant laboratory parameters)
Thrombocytosis (including increased levels
platelets)A
Immune system disorders
Allergic reaction, allergic
dermatitis
Nervous system disorders
Dizziness, headache
Intracerebral and intracranial hemorrhages,
fainting
Visual disorders
Bleeding in the eye (including bleeding in the eye)
conjunctiva)
Violations with
sides of the heart
Tachycardia
Vascular disorders
Marked decrease in arterial
pressure, hematoma
Disorders of the respiratory system, chest organs and
mediastinum
Nosebleeds, hemoptysis
Gastrointestinal disorders
Bleeding gums, gastrointestinal bleeding (including rectal bleeding), abdominal pain, dyspepsia, nausea, constipation,
diarrhea, vomitingA
Dry mouth
Liver and biliary disorders
ways
Liver dysfunction
Jaundice
Skin and subcutaneous tissue disorders
Pruritus (including rare cases of generalized pruritus), skin rash, ecchymosis, cutaneous and subcutaneous
hemorrhages
Hives
Musculoskeletal and connective tissue disorders
fabrics
Pain in limbsA
Hemarthrosis
Bleeding into a muscle
Renal and urinary tract disorders
Bleeding from the urogenital tract (including hematuria and menorrhagia), renal dysfunction (including increased creatinine concentrations, increased concentrations of
urea)A
General and administration site disorders
FeverA, peripheral edema, decreased overall muscle strength and tone (including weakness,
asthenia)
Deterioration in general health (including malaise)
Local edema
Laboratory and instrumental data
Increased activity
“liver” transaminases
Increased bilirubin concentration, increased alkaline phosphatase A activity, increased LDHA activity, increased lipase A activity, increased amylase A activity, increased
GGTA activity
Increased concentration of conjugated bilirubin (with or without a concomitant increase in ALT activity)
Injuries, intoxications and complications of manipulations
Hemorrhages after procedures (including postoperative anemia and bleeding from
wounds), hematoma
Secretion from a woundA
Vascular pseudoaneurysmC
And were observed mainly after major orthopedic operations on the lower extremities
B observed in the treatment of VTE as very common in women aged < 55 years
C were observed as infrequent as part of the prevention of complications in ACS (after percutaneous interventions).
*A prespecified selective approach was used to collect data on adverse events. Because the incidence of adverse drug reactions did not increase, and because no new adverse drug reactions were identified, data from the COMPASS study were not included to calculate the incidence in this table.
During post-marketing monitoring, cases of the following adverse reactions were reported, the development of which had a temporary relationship with taking Xarelto®. It is not possible to assess the frequency of occurrence of such adverse reactions within the framework of post-registration monitoring.
Immune system disorders: angioedema, allergic edema. In the phase III RCT, such adverse events were considered infrequent (>1/1000 to <1/100).
Disorders of the liver and biliary tract: cholestasis, hepatitis (including hepatocellular damage). In the phase III RCT, such adverse events were considered rare (>1/10,000 to <1/1,000).
Disorders of the circulatory and lymphatic system: thrombocytopenia. In the phase III RCT, such adverse events were considered infrequent (>1/1000 to <1/100).
Interaction
Interaction
Pharmacokinetic interactions
Elimination of rivaroxaban occurs primarily through hepatic metabolism mediated by the cytochrome P450 system (CYP3A4, CYP2J2), as well as through renal excretion of unchanged drug using the P-gp/Bcrp (P-glycoprotein/breast cancer resistance protein) transporter systems.
CYP inhibition
Rivaroxaban does not inhibit CYP 3A4 or any other major CYP isoforms.
CYP induction
Rivaroxaban does not induce CYP 3A4 or any other major CYP isoforms.
Effect on rivaroxaban
Concomitant use of rivaroxaban and strong inhibitors of CYP3A4 and P-glycoprotein may result in decreased renal and hepatic clearance of rivaroxaban and thus significantly increase its systemic exposure.
The combined use of rivaroxaban and the azole antifungal agent ketoconazole (400 mg 1 time per day), which is a potent inhibitor of CYP3A4 and P-glycoprotein, led to an increase in the average steady-state AUC of rivaroxaban by 2.6 times and an increase in the average Cmax of rivaroxaban by 1.7 times, which was accompanied by a significant increase in the pharmacodynamic effect of the drug.
Co-administration of rivaroxaban and the HIV protease inhibitor ritonavir (600 mg 2 times a day), which is a potent inhibitor of CYP3A4 and P-glycoprotein, led to an increase in the average steady-state AUC of rivaroxaban by 2.5 times and an increase in the average Cmax of rivaroxaban by 1.6 times, which was accompanied by a significant increase in the pharmacodynamic effect of the drug. In this regard, rivaroxaban is not recommended for use in patients receiving systemic treatment with azole antifungals or HIV protease inhibitors (see sections “Precautions”, “Special Instructions”).
Clarithromycin (500 mg twice daily), a potent CYP3A4 inhibitor and moderate P-glycoprotein inhibitor, increased the AUC and Cmax of rivaroxaban by 1.5-fold and the AUC by 1.4-fold. This increase is in the order of normal variability in AUC and Cmax and is considered clinically insignificant.
Erythromycin (500 mg 3 times a day), a moderate inhibitor of the CYP3A4 isoenzyme and P-glycoprotein, caused an increase in the AUC and Cmax values of rivaroxaban by 1.3 times. This increase is in the order of normal variability in AUC and Cmax and is considered clinically insignificant.
In patients with mild renal impairment (CrCl 50-80 ml/min), erythromycin (500 mg 3 times daily) caused an increase in rivaroxaban AUC by 1.8 times and Cmax by 1.6 times compared with patients with normal renal function who did not receive concomitant therapy. In patients with moderate renal impairment (CrCl 30-49 ml/min), erythromycin caused an increase in rivaroxaban AUC values by 2.0 times and Cmax by 1.6 times compared with patients with normal renal function who did not receive concomitant therapy (see section “With caution”).
Fluconazole (400 mg once daily), a moderate CYP3A4 inhibitor, caused a 1.4-fold increase in mean rivaroxaban AUC and a 1.3-fold increase in mean Cmax. This increase is in the order of normal variability in AUC and Cmax and is considered clinically insignificant.
Concomitant use of rivaroxaban with dronedarone should be avoided due to limited clinical data on coadministration.
Co-administration of Xarelto® with rifampicin, a potent inducer of CYP3A4 and P-glycoprotein, resulted in a decrease in the mean AUC of rivaroxaban by approximately 50% and a parallel decrease in its pharmacodynamic effects. Concomitant use of rivaroxaban with other strong CYP3A4 inducers (eg, phenytoin, carbamazepine, phenobarbital or St. John’s wort) may also result in decreased plasma concentrations of rivaroxaban. The decrease in rivaroxaban plasma concentrations was considered clinically insignificant. Potent CYP3A4 inducers should be used with caution.
Pharmacodynamic interactions
After simultaneous use of enoxaparin sodium (single dose 40 mg) and Xarelto® (single dose 10 mg), a additive effect was observed on anti-factor Xa activity, which was not accompanied by additional additive effects on blood clotting tests (prothrombin time, aPTT). Enoxaparin sodium did not change the pharmacokinetics of rivaroxaban (see section “Precautions”).
Due to the increased risk of bleeding, caution should be exercised when combined with any other anticoagulants.
No pharmacokinetic interaction was found between Xarelto® (15 mg) and clopidogrel (loading dose of 300 mg followed by a maintenance dose of 75 mg), but in a subgroup of patients a significant increase in bleeding time was found, which did not correlate with the degree of platelet aggregation and the content of P-selectin or GPIIb/IIIa receptor (see section “Precautions”).
After co-administration of Xarelto® (15 mg) and naproxen 500 mg, no clinically significant increase in bleeding time was observed. However, a more pronounced pharmacodynamic response is possible in some individuals.
Caution should be exercised when using Xarelto® together with NSAIDs (including acetylsalicylic acid) and platelet aggregation inhibitors, since the use of these drugs usually increases the risk of bleeding.
Switching patients from warfarin (INR 2.0 to 3.0) to Xarelto® (20 mg) or from Xarelto® (20 mg) to warfarin (INR 2.0 to 3.0) increased prothrombin time/INR (Neoplastin) to a greater extent than would be expected from simple summation of effects (individual INR values can be as high as 12), while the effect on APTT, factor Xa suppression, and endogenous thrombin potential were additive.
If it is necessary to study the pharmacodynamic effects of Xarelto® during the transition period, anti-Xa activity, PiCT and HepTest® can be used as necessary tests that are not affected by warfarin. Starting from the 4th day after stopping the use of warfarin, all test results (including PT, aPTT, inhibition of factor Xa activity and EPT (endogenous thrombin potential)) reflect only the effect of the drug Xarelto.
If it is necessary to study the pharmacodynamic effects of warfarin during the transition period, measurement of the INR value at Interim can be used. rivaroxaban (24 hours after the previous dose of rivaroxaban), since rivaroxaban has minimal effect on this indicator during this period.
No pharmacokinetic interactions have been reported between warfarin and Xarelto®.
The drug interaction of Xarelto® with the vitamin K antagonist (VKA) phenindione has not been studied. It is recommended, whenever possible, to avoid transferring patients from therapy with Xarelto® to VKA phenindione therapy and vice versa.
There is limited experience in switching patients from VKA acenocoumarol therapy to Xarelto®.
If there is a need to transfer a patient from therapy with Xarelto® to VKA therapy with phenindione or acenocoumarol, then special care should be taken; during the period of joint use of Xarelto® and VKA, daily monitoring of the pharmacodynamic effect of the drugs (INR, prothrombin time) should be carried out immediately before taking the next dose of Xarelto®.
If there is a need to transfer a patient from VKA therapy with phenindione or acenocoumarol to therapy with Xarelto®, then special care should be taken; monitoring of the pharmacodynamic effect of the drugs is not required.
As with other anticoagulants, caution should be exercised when Xarelto is co-administered with selective serotonin reuptake inhibitors (SSRIs) and selective serotonin norepinephrine reuptake inhibitors (SNRIs) as these drugs increase the risk of bleeding. The results of clinical studies demonstrated a numerical increase in major and minor clinically significant bleeding in all treatment groups when these drugs were used together.
Food and dairy products
Xarelto® 15 mg and 20 mg should be taken with food (see section “Pharmacological properties”).
No interactions detected
No pharmacokinetic interactions have been identified between rivaroxaban and midazolam (CYP3A4 substrate), digoxin (P-gp substrate) or atorvastatin (CYP3A4 and P-gp substrate).
Co-administration with the proton pump inhibitor omeprazole, the H2 receptor antagonist ranitidine, aluminum hydroxide/magnesium hydroxide antacids, naproxen, clopidogrel or enoxaparin does not affect the bioavailability and pharmacokinetics of rivaroxaban.
No clinically significant pharmacokinetic or pharmacodynamic interactions were observed with the combined use of Xarelto® and 500 mg of acetylsalicylic acid.
Effect on laboratory parameters
Xarelto® has an effect on blood clotting parameters (PT, APTT, HepTest®) due to its mechanism of action (see section “Pharmacological properties/Pharmacodynamic effects”)
Overdose
Overdose
Rare cases of overdose have been reported when taking rivaroxaban up to 600 mg without bleeding or other adverse reactions. Due to limited absorption, the development of a low-level plateau in drug concentration is expected without a further increase in its average plasma concentration when using doses exceeding therapeutic doses of 50 mg and above.
The specific antidote for rivaroxaban is unknown. In case of overdose, activated charcoal can be used to reduce the absorption of rivaroxaban. Given its extensive binding to plasma proteins, it is expected that rivaroxaban will not be eliminated during dialysis.
Treatment of bleeding
If a bleeding complication occurs in a patient receiving rivaroxaban, the next dose of the drug should be delayed or, if necessary, treatment with this drug should be discontinued. The half-life of rivaroxaban is approximately 5-13 hours. Treatment should be individualized depending on the severity and location of the bleeding. If necessary, appropriate symptomatic treatment can be used, such as mechanical compression (for example, for severe epistaxis), surgical hemostasis with evaluation of its effectiveness, fluid therapy and hemodynamic support, the use of blood products (packed red blood cells or fresh frozen plasma, depending on whether anemia or coagulopathy occurs) or platelets.
If the above measures do not eliminate bleeding, specific procoagulant drugs, such as prothrombin complex concentrate, activated prothrombin complex factor concentrate, or recombinant factor VIIa, may be prescribed. However, at present, experience with the use of these drugs in patients receiving Xarelto® is very limited.
Protamine sulfate and vitamin K are not expected to affect the anticoagulant activity of rivaroxaban.
There is limited experience with the use of tranexamic acid and no experience with the use of aminocaproic acid and aprotinin in patients receiving Xarelto®. There is no scientific basis for or experience with the use of the systemic hemostatic drug desmopressin in patients receiving Xarelto®.
Storage conditions
Storage conditions
At a temperature not higher than 30 °C. Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after expiration date
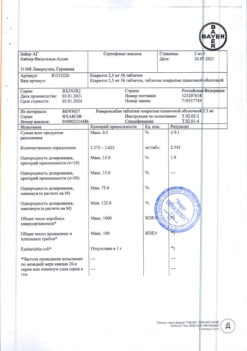
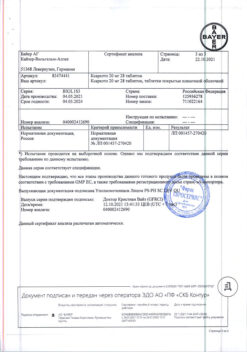
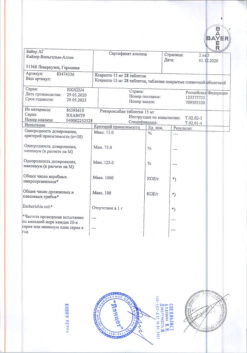
Manufacturer
Manufacturer
Bayer AG, Germany
Additional information
| Shelf life | 3 years. Do not use after the expiration date |
|---|---|
| Conditions of storage | At a temperature not higher than 30 ° C. Keep out of reach of children. |
| Manufacturer | Bayer AG, Germany |
| Medication form | pills |
| Brand | Bayer AG |
Other forms…
Related products
Buy Xarelto, 15 mg 98 pcs with delivery to USA, UK, Europe and over 120 other countries.