No products in the cart.
Xalacom, eye drops 2.5 ml
€30.04 €25.03
Description
Because of the different mechanism of lowering elevated intraocular pressure of timolol and latanoprost, Xalacom combined eye drops are more effective in reducing IOP in patients compared to the use of each active ingredient alone.
Latanoprost increases aqueous humor outflow without affecting aqueous humor production. Timolol decreases aqueous humor production in the ciliary epithelium without affecting cardiac muscle function.
Latanoprost penetrates easily through the cornea of the eye, maximum concentration in aqueous humor about 2 hours after injection (in monotherapy). It is almost not metabolized in the eye tissues. The elimination half-life of lathanoprost acid is 17 minutes. Metabolites are excreted with urine and have no marked biological activity.
In aqueous humor timololol is maximally concentrated one hour after injection (in monotherapy). Timolol is partially absorbed systemically, appearing in blood plasma at a concentration of 1 ng/ml after 10-20 minutes. The plasma elimination half-life is about 6 hours. It is excreted with urine.
The concentration of acid latanoprost in aqueous humor may increase in 1-4 hours after injection of Xalacom eye drops (compared to monotherapy).
Pharmacokinetics
No pharmacokinetic interaction between latanoprost and timolol maleate has been established, although 1-4 h after Xalacom administration, latanoprost acid concentration in aqueous humor was approximately 2 times higher than with monotherapy.
Latanoprost
Intake
Latanoprost, being a prodrug, penetrates well through the cornea and is hydrolyzed to its bioactive form (acid). Cmax in aqueous humor is reached 2 h after topical application. Systemic bioavailability of latanoprost acid after topical application of eye drops is 45%.
Distribution
Vd is 0.16±0.02 L/kg. Latanoprost acid is determined in aqueous humor during the first 4 h, and in plasma only during the first hour after topical administration. Binding to plasma proteins is 87%.
Metabolism
Latanoprost undergoes hydrolysis in the cornea by esterases to form bioactive acid. Latanoprost acid entering the systemic bloodstream is metabolized primarily in the liver by beta-oxidation of fatty acids to form 1,2-dinor- and 1,2,3,4-tetranor metabolites.
Elimination
Latanoprost acid is rapidly excreted from the blood plasma. T1/2 is 17 min. Plasma clearance is 0.4 L/h/kg. Systemic clearance is approximately 7 ml/min/kg. Metabolites are excreted mainly by the kidneys: after topical administration, about 88% of the dose is excreted with the urine.
Timolol maleate
Intake
The Cmax of timololol maleate in aqueous humor is reached after 1 hour. Part of the dose undergoes systemic absorption and 10-20 minutes after topical administration of the drug 1 drop in each eye 1 time/day (300 mcg/day), a plasma Cmax of 1 ng/mL is reached.
Metabolism and excretion
Timolol maleate is actively metabolized in the liver. T1/2 timolol maleate from plasma is about 6 h. Metabolites, as well as some unchanged timolol maleate, are excreted by the kidneys.
Indications
Indications
Reduction of elevated intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension with insufficient effectiveness of monotherapy with individual components of the drug.
Pharmacological effect
Pharmacological effect
Mechanism of action
The drug Xalacom contains two active components – latanoprost and timolol. The mechanism by which these components reduce elevated intraocular pressure (IOP) is different, which provides an additional reduction in IOP compared to the effect achieved when using each of these components as monotherapy.
Latanoprost, a prostaglandin F2α analogue, is a selective agonist of prostanoid FP receptors and reduces IOP by increasing the outflow of aqueous humor, mainly through the uveoscleral pathway, but also through the trabecular meshwork. It has been established that latanoprost does not have a significant effect on the production of aqueous humor and the permeability of the blood-ophthalmic barrier. During short-term treatment, latanoprost does not cause fluorescein leakage into the posterior segment of the pseudophakic eye. When used in therapeutic doses, latanoprost does not have a significant pharmacological effect on the cardiovascular and respiratory systems. Timolol is a non-selective β1- and β2-adrenergic blocker that does not have significant internal sympathomimetic activity, does not have a direct inhibitory effect on the myocardium or a local anesthetic (membrane stabilizing) effect.
Blockade of β-adrenergic receptors causes a decrease in cardiac output in healthy people and patients with heart disease. In patients with severe myocardial dysfunction, β-blockers may inhibit the stimulatory effect of the sympathetic nervous system, which is necessary for adequate cardiac function.
Blockade of β-adrenergic receptors in the bronchi and bronchioles leads to an increase in airway resistance under the influence of the parasympathetic nervous system. This effect can be dangerous for patients with bronchial asthma and other bronchospastic diseases (see sections 4.3 and 4.4).
The use of timolol in the form of eye drops causes a decrease in elevated and normal IOP, regardless of the presence or absence of glaucoma. Elevated IOP is a major risk factor for glaucomatous visual field loss. The higher the IOP, the higher the likelihood of glaucomatous visual field loss and optic nerve damage.
The exact mechanism by which timolol lowers IOP has not been established. The results of tonography and fluorophotometry indicate that the main mechanism of action may be associated with a decrease in the formation of aqueous humor. However, some studies also noted a slight increase in churn. In addition, a mechanism of inhibition of increased cyclic AMP synthesis caused by endogenous β-adrenergic stimulation is also possible. No effect of timolol on the permeability of the blood-ophthalmic barrier was noted.
The effect of the combination of latanoprost and timolol begins within an hour, and the maximum effect is observed within 6-8 hours.
With repeated use, an adequate reduction in IOP persists for 24 hours after administration.
Pharmacokinetic interactions between latanoprost and timolol have not been established, although 1-4 hours after administration of the combination drug, the concentration of latanoprost acid in the aqueous humor was approximately twice as high as with monotherapy.
Latanoprost:
Suction
Latanoprost, being a prodrug form, is absorbed through the cornea, where it is hydrolyzed to a biologically active acid. It has been established that the concentration in aqueous humor reaches a maximum approximately two hours after topical application.
Distribution
The volume of distribution is 0.16 0.02 l/kg. Latanoprost acid is determined in aqueous humor during the first 4 hours, and in plasma only during the first hour after topical application.
Metabolism
Latanoprost undergoes hydrolysis in the cornea under the action of esterases to form a biologically active acid. Latanoprost acid entering the systemic circulation is metabolized mainly in the liver by β-oxidation of fatty acids with the formation of 1,2-dinor and 1,2,3,4-tetranor metabolites.
Removal
Latanoprost acid is rapidly cleared from plasma – half-life (t1/2) = 17 minutes. Plasma clearance is 0.40 l/h/kg. System clearance is approximately
7 ml/min/kg. After topical application of eye drops, the systemic bioavailability of latanoprost acid is 45%. The connection with blood plasma proteins is 87%. Metabolites are excreted mainly by the kidneys: after topical application, approximately 88% of the administered dose is excreted in the urine.
Timolol:
The concentration of timolol in aqueous humor reaches a maximum approximately 1 hour after application of eye drops. Part of the dose is subject to systemic absorption, and the maximum plasma concentration of 1 ng/ml is achieved 10-20 minutes after administration of the drug, one drop in each eye once a day (300 mcg/day). The half-life of timolol from plasma is about 6 hours. Timolol is actively metabolized in the liver. Metabolites, as well as some unchanged timolol, are excreted in the urine.
Special instructions
Special instructions
Xalacom should be used no more than once a day, since more frequent administration of latanoprost leads to a weakening of the IOP-lowering effect.
If one dose is missed, the next dose should be given at the usual time.
If the patient is using other eye drops at the same time, they should be used at least 5 minutes apart.
Xalacom contains benzalkonium chloride, which can be absorbed by contact lenses. There are reports of the development of punctate keratopathy and/or toxic ulcerative keratopathy, and eye irritation and discoloration of soft contact lenses may occur with the use of benzalkonium chloride. Careful monitoring of the condition of patients using Xalacom frequently or for a long time, who have dry eye mucosa or conditions that damage the cornea, is recommended. Before instilling drops, contact lenses must be removed and reinserted after 15 minutes.
Latanoprost
Changes in the content of brown pigment Latanoprost can cause a gradual increase in the content of brown pigment in the iris. As with the use of latanoprost in the form of eye drops, when using the drug Xalacom, an increase in iris pigmentation was noted in 16-20% of cases among all patients receiving Xalacom during the year (assessed based on photographs).
The change in eye color is caused by an increase in the melanin content in the stromal melanocytes of the iris, and not by an increase in the number of melanocytes themselves. In typical cases, brown pigmentation appears around the pupil and extends concentrically to the periphery of the iris. In this case, the entire iris or parts of it become brown. In most cases, the color change is minor and may not be clinically detectable. Increased pigmentation of the iris of one or both eyes is observed mainly in patients with mixed iris color, containing a brown color as a base. The drug has no effect on nevi and lentigines of the iris; no accumulation of pigment in the trabecular meshwork or in the anterior chamber of the eye was noted.
When determining the degree of pigmentation of the iris for more than 5 years, no undesirable consequences of increased pigmentation were revealed, even with continued therapy with latanoprost. In patients, the degree of IOP reduction was the same, regardless of the presence or absence of increased iris pigmentation. Therefore, treatment with latanoprost can be continued in cases of increased pigmentation of the iris. Such patients should be monitored regularly and, depending on the clinical situation, treatment may be discontinued.
Increased pigmentation of the iris is usually observed during the first year after the start of treatment, rarely during the second or third year. After the fourth year of treatment, this effect was not observed. The rate of pigmentation progression decreases over time and stabilizes after 5 years. In the longer term, the effects of increased iris pigmentation have not been studied. After stopping treatment, no increase in brown pigmentation of the iris was noted, but the change in eye color may be irreversible.
Patients using drops in only one eye may develop heterochromia, which may also be irreversible.
Changes in eyelashes and vellus hair
In connection with the use of latanoprost, cases of darkening of the skin of the eyelids have been described, which may be reversible.
Latanoprost may cause gradual changes in eyelashes and vellus hairs, such as lengthening, thickening, increased pigmentation, increased thickness, and a change in the direction of eyelash growth. Changes in eyelashes are reversible and disappear after cessation of treatment.
Timolol
When beta-blockers are used topically, the same adverse reactions may occur as when they are used systemically. Patients with a history of severe heart disease should be closely monitored for early detection of symptoms of heart failure. With local use of timolol, the following reactions from the heart and respiratory system may occur: progression of Prinzmetal’s angina, as well as peripheral and central circulatory disorders, hypotension, fatal heart failure, severe reactions from the respiratory system, incl. bronchospasm with fatal outcome in patients with bronchial asthma, bradycardia.
Before undergoing major surgery, the advisability of gradual withdrawal of beta-blockers should be discussed. Drugs in this group impair the heart’s ability to respond to reflex β-adrenergic stimulation, which may increase the risk during general anesthesia. Cases of prolonged severe decrease in blood pressure during anesthesia and difficulties in restoring and maintaining heart contractions have been described. During surgery, the effects of β-blockers can be reversed by sufficient doses of adrenergic agonists.
Drugs with beta-blocking effects may block the systemic agonist effects such as epinephrine. It is necessary to warn the anesthesiologist that the patient is receiving timolol.
β-blockers can enhance the hypoglycemic effect of antidiabetic agents and mask the symptoms and manifestations of hypoglycemia. They should be used with caution in patients with spontaneous hypoglycemia or diabetes mellitus (especially labile cases) receiving insulin or oral hypoglycemic agents.
Therapy with β-blockers may mask some of the underlying symptoms and manifestations of hyperthyroidism. Abrupt cessation of treatment may cause an exacerbation of this disease.
When treated with β-blockers in patients with atopy or a history of severe anaphylactic reactions to various allergens, the response may be enhanced upon repeated contact with these allergens. However, epinephrine in normal doses used to relieve anaphylactic reactions may be ineffective.
In rare cases, timolol has caused increased muscle weakness in patients with myasthenia gravis or myasthenic symptoms (eg, diplopia, ptosis, generalized weakness).
When using drugs that reduce IOP, cases of detachment of the choroid after filtration procedures – fistulizing operations (trabeculectomy and its modifications, sinusotomy with diathermotrabeculospasis, non-penetrating deep sclerectomy and other fistulizing operations that create new or stimulate existing pathways for the outflow of intraocular fluid) have been described.
Active ingredient
Active ingredient
Latanoprost, Timolol
Composition
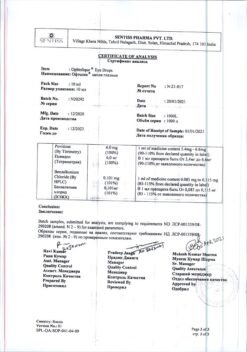
Composition
Active ingredients: latanoprost + timolol.
1 ml of solution contains 0.050 mg of latanoprost and 6.83 mg of timolol maleate, which is equivalent to 5 mg of timolol.
Excipients, the presence of which must be taken into account in the composition of the medicinal product: benzalkonium chloride (in the form of a 50% solution), anhydrous sodium hydrogen phosphate, sodium dihydrogen phosphate monohydrate, sodium chloride, water for injection.
Pregnancy
Pregnancy
There are no adequate controlled studies in pregnant women.
In epidemiological studies, there were no cases of fetal malformations when using beta-blockers orally, but the risk of intrauterine growth retardation was increased. In addition, symptoms of β-blocker action (such as bradycardia, decreased blood pressure, respiratory dysfunction and hypoglycemia) were identified in newborns whose mothers took β-blockers during pregnancy. If a pregnant woman has received β-blocker therapy, the condition of the newborn should be carefully monitored in the first days after birth. In this regard, the use of Xalacom during pregnancy is possible only in cases where the expected benefit to the mother outweighs the potential risk to the fetus or child. Latanoprost and its metabolites may be excreted into breast milk. Timolol, when used in the form of eye drops, has also been found in breast milk. Given the risk of serious adverse reactions in breastfed newborns, as well as the importance of the drug for the mother, you should either stop breastfeeding or discontinue the drug.
Contraindications
Contraindications
– hypersensitivity to the active substances or to any of the excipients listed in section 6.1;
– reactive airway disease, including bronchial asthma or a history of bronchial asthma, severe chronic obstructive pulmonary disease;
– sinus bradycardia, sick sinus syndrome, sinoatrial block, II-III degree atrioventricular block without control of an artificial pacemaker, clinically significant heart failure, cardiogenic shock.
Side Effects
Side Effects
Security Profile Summary
Most of the adverse reactions associated with latanoprost affect the visual system. According to data obtained as a result of an additional phase of pivotal studies of the drug Xalacom, 16-20% of patients experienced increased pigmentation of the iris, which may be irreversible. In a 5-year open-label safety study of latanoprost, iris pigmentation developed in 33% of patients (see section 4.4). Other adverse reactions from the organ of vision were mainly short-term and occurred during the administration of the drug dose. For timolol, the most serious adverse reactions are systemic and include bradycardia, arrhythmia, congestive heart failure, bronchospasm and allergic reactions. As with other ophthalmic drugs for topical use, timolol enters the circulatory system after absorption. As a result, the same undesirable effects may occur as when taking systemic beta-blockers. The incidence of systemic adverse drug reactions after topical application to the eyes is lower than with systemic administration. The listed adverse reactions include reactions that are characteristic of the entire class of ophthalmic beta-blockers.
Summary of adverse reactions
The frequency of adverse reactions is presented according to the following classification:
Very frequent – 10%
Frequent – 1% and <10%
Uncommon – 0.1% and <1%
Rare – 0.01% and <0.1%
Very rare – <0.01%
Violations of the organ of vision: very common – increased pigmentation of the iris, cataracts; common: visual impairment, blepharitis, conjunctivitis, conjunctival lesions (follicles, papillary reactions of the conjunctiva, pinpoint hemorrhages, etc.), corneal lesions (erosions, pigmentation, keratitis, pinpoint keratitis, etc.), refractive errors, conjunctival hyperemia, eye irritation (including burning sensation and itching in eyes), pain in the eyes, photophobia, loss of visual fields, increased tear production; uncommon: hypertrichosis (changes in eyelashes and vellus hair, lengthening, thickening, increased pigmentation, increased thickness and change in the direction of eyelash growth); unknown: changes in refraction.
Infectious and parasitic diseases: common – sinusitis, upper respiratory tract infections and other infections.
Metabolic and nutritional disorders: common – diabetes mellitus, hypercholesterolemia.
Mental disorders: frequent – depression.
Nervous system disorders: frequent – headache.
Cardiovascular system disorders: frequent – increased blood pressure.
Disorders of the skin and subcutaneous tissues: frequent – rash, itching and skin changes (irritation, dermatochalazion, etc.), skin diseases.
Musculoskeletal and connective tissue disorders: common – arthritis. Listed below are other adverse events that were observed during monotherapy with individual components of the drug Xalac (in addition to those listed above).
Latanoprost:
Visual disorders: eye irritation (burning sensation, feeling of sand in the eyes, itching, tingling and foreign body sensation); transient punctate erosions of the corneal epithelium*, eyelid edema, keratitis, punctate keratitis*; swelling of the cornea*, lengthening, thickening, increasing the number and increasing pigmentation of eyelashes and vellus hair; iritis/uveitis*; macular edema (in patients with aphakia, in patients with pseudophakia with rupture of the posterior capsule of the lens, or in patients with risk factors for the development of macular edema), incl. cystoid*; trichiasis*; blurred vision*, photophobia*, changes in the periorbital area and eyelids leading to deepening of the upper eyelid sulcus*, periorbital edema, iris cysts*.
Disorders of the cardiovascular system: exacerbation of angina in patients with coronary heart disease, angina pectoris, unstable angina, palpitations.
Skin and subcutaneous tissue disorders: skin rash, itching*, darkening of the eyelid skin and local skin reactions on the eyelids.
Nervous system disorders: dizziness.
Disorders of the respiratory system, chest and mediastinal organs: asthma (including acute attacks or exacerbation of the disease in patients with a history of bronchial asthma)*, shortness of breath*.
Musculoskeletal and connective tissue disorders: myalgia*, arthralgia*.
General disorders and disorders at the injection site: nonspecific chest pain*.
Infections: herpetic keratitis.
*Adverse reactions registered in the post-marketing period.
Timolol (in the form of eye drops):
Immune system disorders: systemic allergic reactions, including anaphylaxis, angioedema, anaphylactic reactions, urticaria, pruritus, localized and generalized rash.
Metabolic and nutritional disorders: anorexia, hidden symptoms of hypoglycemia in patients with diabetes mellitus.
Mental disorders: behavioral changes and mental disorders, including confusion, hallucinations, anxiety, disorientation, nervousness, memory loss, insomnia, depression and nightmares.
Nervous system disorders: cerebral ischemia, acute cerebrovascular accidents, dizziness, increased symptoms of myasthenia gravis, paresthesia, drowsiness, headache, fainting.
Violations of the organ of vision: cystoid macular edema, decreased sensitivity of the cornea; symptoms and signs of eye irritation (eg, burning sensation, itching, gritty sensation in the eyes, increased lacrimation, redness), blepharitis, keratitis, blurred vision, dry eye mucosa, corneal erosion, choroidal detachment after filtration surgery; ptosis, visual impairment, including changes in refraction and diplopia.
Hearing and labyrinthine disorders: tinnitus.
Cardiac disorders: arrhythmia, bradycardia, atrioventricular block, heart failure, chronic heart failure, cardiac arrest, intracardiac conduction block, palpitations, progression of angina.
Vascular disorders: intermittent claudication, cold hands and feet, decreased blood pressure, Raynaud’s syndrome.
Disorders of the respiratory system, chest and mediastinal organs: bronchospasm (mainly in patients with previous bronchospastic diseases), cough, shortness of breath, nasal congestion, pulmonary edema and respiratory failure.
Gastrointestinal disorders: diarrhea, dry oral mucosa, impaired taste, dyspepsia, nausea, vomiting, abdominal pain, retroperitoneal fibrosis.
Skin and subcutaneous tissue disorders: alopecia, pseudopemphigoid, skin rash, psoriasis-like rash or exacerbation of psoriasis.
Musculoskeletal and connective tissue disorders: systemic lupus erythematosus and myalgia.
Genital and breast disorders: decreased libido, impotence, sexual dysfunction and Peyronie’s disease.
General disorders and disorders at the injection site: asthenia/fatigue, chest pain, edema.
Very rare cases of corneal calcification have been reported in some patients with significant corneal damage in association with the use of phosphate eye drops.
Reporting suspected adverse reactions
It is important to report suspected adverse reactions after registration of a medicinal product to ensure continuous monitoring of the benefit-risk profile of the medicinal product. Healthcare professionals are encouraged to report any suspected adverse drug reactions through the national adverse reaction reporting systems of the member states of the Eurasian Economic Union.
Interaction
Interaction
The interaction of Xalacom with other drugs has not been specifically studied. When using the drug Xalacom in patients receiving a beta-blocker orally, a more pronounced decrease in IOP or increased systemic manifestations of beta-blockers is possible, therefore the simultaneous local use of two or more beta-blockers is not recommended.
When two prostaglandin analogs are instilled into the eyes simultaneously, a paradoxical increase in IOP has been described, therefore the simultaneous use of two or more prostaglandins, their analogs or derivatives is not recommended.
With the simultaneous use of timolol with epinephrine, mydriasis sometimes developed. When timolol is combined with the following drugs, an additive effect with a decrease in blood pressure and/or severe bradycardia is possible:
– blockers of “slow” calcium channels;
– agents that cause a decrease in catecholamine levels, or β-blockers;
– antiarrhythmic drugs (including amiodarone);
– cardiac glycosides;
– guanethidine.
Increased effects of systemic beta-blockers (eg, decreased heart rate, depression) have been reported with concomitant use of CYP2D6 inhibitors (eg, quinidine, fluoxetine, paroxetine) and timolol.
β-blockers can enhance the hypoglycemic effect of hypoglycemic drugs.
An increase in blood pressure is observed when clonidine is suddenly discontinued. This reaction may be enhanced when used concomitantly with β-blockers.
In vitro studies have shown that when eye drops containing thiomersal are mixed with the drug, a precipitate forms. When using such medications simultaneously with Xalacom, eye drops should be instilled at intervals of at least 5 minutes.
Overdose
Overdose
Below is information about overdose with the components of the drug:
Latanoprost
Apart from eye irritation and conjunctival hyperemia, other undesirable changes in the organ of vision are not known with an overdose of latanoprost.
If you accidentally take latanoprost orally, the following information should be taken into account: one bottle of 2.5 ml of solution contains 125 mcg of latanoprost. More than 90% of latanoprost is metabolized during the first passage through the liver. Intravenous infusion at a dose of 3 mcg/kg in healthy volunteers did not cause any symptoms, but when a dose of 5.5-10 mcg/kg was administered, nausea, abdominal pain, dizziness, fatigue were observed
“hot flashes” and sweating. These symptoms resolve 4 hours after stopping the infusion. In patients with moderate bronchial asthma, administration of latanoprost into the eyes at a dose 7 times higher than the therapeutic dose did not cause bronchospasm.
Timolol
Cases of unintentional overdose of timolol eye drops have been described, resulting in systemic effects similar to those with systemic use of beta-blockers: dizziness, headache, shortness of breath, bradycardia, bronchospasm and cardiac arrest (see section 4.8).
In an in vitro study, timolol was shown to be readily cleared from plasma or whole blood upon dialysis.
In patients with renal failure, timolol dialyzed less well. In case of overdose, symptomatic treatment is carried out.
Storage conditions
Storage conditions
Store at a temperature of 2 to 8 °C, protected from light.
Store the opened bottle at a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years
Use the opened bottle within 4 weeks.
Do not use after the expiration date stated on the package.
Manufacturer
Manufacturer
USA
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a light-protected place, at 2-8 °C |
| Manufacturer | Pfizer, Puerto Rico |
| Medication form | eye drops |
| Brand | Pfizer |
Related products
Buy Xalacom, eye drops 2.5 ml with delivery to USA, UK, Europe and over 120 other countries.