No products in the cart.
Warfarin, tablets 2.5mg 100 pcs
€5.63 €5.00
Description
Warfarin (4-hydroxycoumarin) is an indirect acting anticoagulant that prevents vitamin K-dependent synthesis of clotting factors II, VII, IX and X, proteins C and S through dose-dependent inhibition of C1-subunit of vitamin K-epoxidoreductase, resulting in reduced production of vitamin K1-epoxide.
S-isomer of warfarin is about 5 times more active than R-isomer. In therapeutic doses warfarin reduces the rate of synthesis of clotting factors by 30-50% and reduces their biological activity. The beginning of the anticoagulation action is observed 36-72 hours after the beginning of the drug administration with maximal effect on the 5th-7th day after the beginning of the drug administration. After discontinuation of the drug activity of vitamin K-dependent clotting factors is restored within 4-5 days.
Indications
Indications
Treatment and prevention of thrombosis and embolism of blood vessels:
acute and recurrent venous thrombosis, pulmonary embolism;
transient ischemic attacks and strokes;
secondary prevention of myocardial infarction and prevention of thromboembolic complications after myocardial infarction;
prevention of thromboembolic complications in patients with atrial fibrillation, lesions of the heart valves or with prosthetic heart valves;
prevention of postoperative thrombosis.
Pharmacological effect
Pharmacological effect
Warfarin (4-hydroxycoumarin) is an indirect anticoagulant that prevents vitamin K-dependent synthesis of blood coagulation factors II, VII, IX and X, proteins C and S due to dose-dependent inhibition of the C1 subunit of vitamin K epoxide reductase, resulting in reduced production of vitamin K1 epoxide.
The S-isomer of warfarin is approximately 5 times more active than the R-isomer. In therapeutic doses, warfarin reduces the rate of synthesis of coagulation factors by 30-50% and reduces their biological activity. The onset of the anticoagulant effect is observed 36-72 hours after the start of taking the drug, with the development of the maximum effect on days 5-7 from the start of use. After stopping the drug, restoration of the activity of vitamin K-dependent blood coagulation factors occurs within 4-5 days.
Special instructions
Special instructions
A prerequisite for warfarin therapy is the patient’s strict adherence to the recommended dose of the drug.
The target MHO value for oral anticoagulant therapy to prevent thromboembolic complications in patients with prosthetic heart valves is 2.5-3; for other indications – 2-3.
Patients with alcoholism or dementia may be unable to adhere to the prescribed warfarin regimen.
In conditions such as fever, hyperthyroidism, decompensated heart failure, alcoholism with concomitant liver damage, the effect of warfarin may be enhanced. With hypothyroidism, the effect of warfarin may be reduced. In the case of chronic renal failure or nephrotic syndrome, the concentration of the free fraction of warfarin in plasma increases, which, depending on concomitant diseases, can lead to either an increase or decrease in the effect. In cases of moderate chronic renal failure, the effect of warfarin is enhanced. In all of the above conditions, careful monitoring of MHO should be carried out.
For patients receiving warfarin, it is recommended to prescribe paracetamol, tramadol or narcotic analgesics as analgesic drugs.
During 1 year of treatment, bleeding is observed in approximately 8% of cases. Of these, 1% are classified as severe (intracranial, retroperitoneal), leading to hospitalization or blood transfusion, and 0.25% as fatal. The most common risk factor for intracranial hemorrhage is uncontrolled arterial hypertension. The likelihood of bleeding increases if the MHO is significantly higher than the target value. If bleeding begins when the MHO is within the target value, then there are other risk factors that should be investigated.
Coumarin necrosis is a rare complication of warfarin treatment. Necrosis usually begins with swelling and darkening of the skin of the lower extremities and buttocks, less commonly in other places. Later the lesions become necrotic. In 90% of cases, necrosis develops in women. Lesions are observed from the 3rd to the 10th day of dosing and the etiology suggests a deficiency of protein C or S. Congenital deficiency of these proteins can cause complications, so warfarin should be started simultaneously with the introduction of heparin and small initial doses of the drug. If a complication occurs, warfarin is discontinued and heparin is continued until the lesions heal or scar.
Hand-foot syndrome is a rare complication of warfarin therapy; its development is typical for men with atherosclerosis. Warfarin causes hemorrhages of atheromatous plaques, leading to microembolism. Symmetrical purple lesions appear on the skin of the fingers and soles of the feet, accompanied by burning pain. After stopping warfarin, these symptoms gradually disappear.
When using warfarin, hypersensitivity reactions may occur, manifested in the form of skin rash and characterized by a reversible increase in the activity of liver enzymes, cholestatic hepatitis, vasculitis, priapism, reversible alopecia and tracheal calcification.
Risk factors for the development of serious bleeding: older age, high intensity of concomitant anticoagulant and antiplatelet therapy, history of strokes and gastrointestinal bleeding, polymorphism of the CYP2C9 isoenzyme gene.
Patients with a mutation in the CYP2C9 isoenzyme gene have a longer T1/2 of warfarin. These patients require lower doses of the drug because… When taking normal therapeutic doses, the risk of bleeding increases.
Active ingredient
Active ingredient
Warfarin
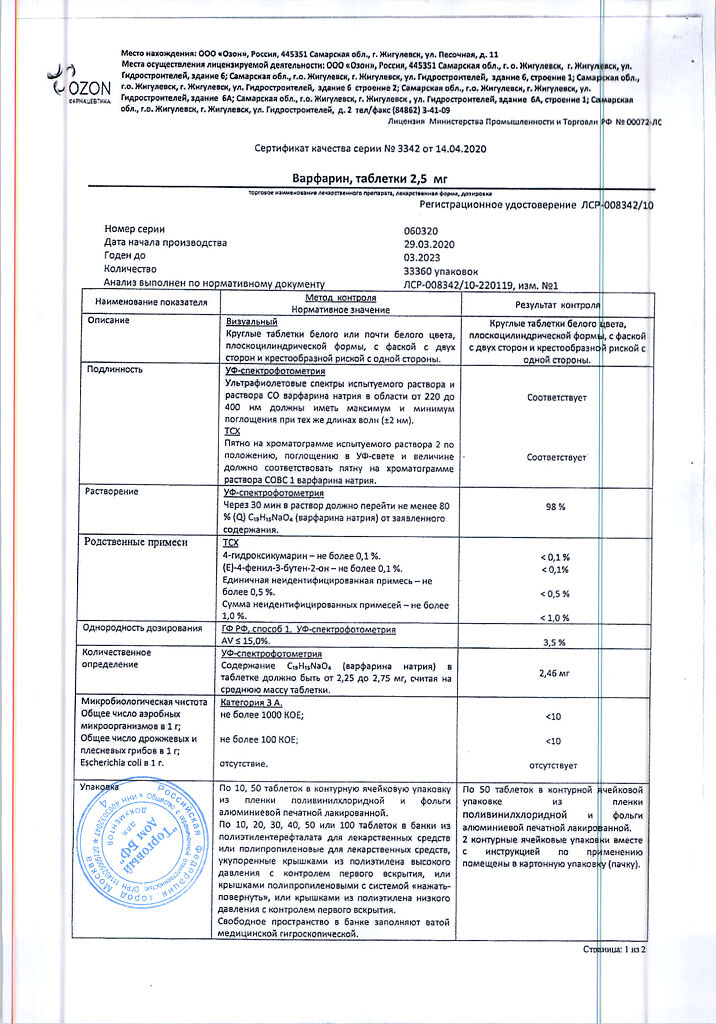
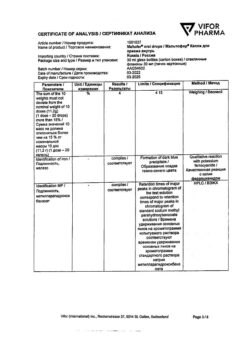
Composition
Composition
1 tablet contains warfarin sodium 2.5 mg.
Contraindications
Contraindications
established or suspected hypersensitivity to the components of the drug;
acute bleeding;
pregnancy (first trimester and last 4 weeks of pregnancy);
severe liver or kidney disease;
acute DIC syndrome;
deficiency of proteins C and S;
thrombocytopenia;
patients at high risk of bleeding, including patients with bleeding disorders;
varicose veins of the esophagus;
arterial aneurysm;
lumbar puncture;
peptic ulcer of the stomach and duodenum;
severe wounds (including surgical wounds)
Side Effects
Side Effects
Frequency: very often – more than 1/10, often – more than 1/100 and less than 1/10, infrequently – more than 1/1000 and less than 1/100, rarely – more than 1/10000 and less than 1/1000.
Very common: increased bleeding.
Common: increased sensitivity to warfarin after prolonged use.
Uncommon: anemia, vomiting, abdominal pain, nausea, diarrhea.
Rarely: eosinophilia, increased activity of liver enzymes, jaundice, rash, urticaria, itching, eczema, skin necrosis, vasculitis, hair loss, nephritis, urolithiasis, tubular necrosis, hand-foot syndrome.
Interaction
Interaction
It is not recommended to start or stop taking other drugs, or change the dose of drugs taken without consulting your doctor.
With the simultaneous use of warfarin and other drugs that affect blood coagulation (including ASA, clopidogrel, ticlopidine, dipyridamole, most NSAIDs (with the exception of low doses of COX-2 inhibitors)), penicillins in high doses, the risk of bleeding increases.
The combined use of warfarin with potent inhibitors of microsomal liver enzymes (including cimetidine and chloramphenicol) should be avoided – there is an increased risk of bleeding. In such cases, cimetidine can be replaced with ranitidine or famotidine.
The anticoagulant effect of warfarin is enhanced by: ASA, allopurinol, amiodarone, azapropazone, azithromycin, interferon alpha, interferon beta, amitriptyline, bezafibrate, influenza vaccine, vitamin E, glibenclamide, glucagon, gemfibrozil, heparin, grepafloxacin, danazol, dextropropoxyphene, diazoxide, digoxin, disopyramide, disulfiram, zafirlukast, indomethacin, ifosfamide, itraconazole, ketoconazole, clarithromycin, clofibrate, codeine, co-trimoxazole, levamisole, lovastatin, metolazone, methotrexate, metronidazole, miconazole (including topical and external use), male sex hormones (anabolic and/or androgenic, including testosterone), nalidixic acid, norfloxacin, ofloxacin, omeprazole, oxyphenbutazone, paracetamol (especially after 1-2 weeks of continuous use), paroxetine, piroxicam, proguanil, propafenone, propranolol, retinol, roxithromycin, sertraline, simvastatin, sulfafurazole, sulfamethizole, sulfafenazole, sulfinpyrazone, sulindac, tamoxifen, tegafur, tetracyclines, thienylic acid, tolmetin, trastuzumab, troglitazone, phenytoin, phenylbutazone, fenofibrate, feprazone, fluconazole, fluoxetine, fluorouracil, fluvastatin, fluvoxamine, flutamide, quinine, quinidine, chloral hydrate, chloramphenicol, celecoxib, cefamandole, cephalexin, cefmenoxime, cefmetazole, cefoperazone, cefuroxime, cimetidine, ciprofloxacin, cyclophosphamide, erythromycin, etoposide, ethanol.
Some medicinal plants can also both enhance the effect of warfarin, for example, ginkgo (Ginkgo biloba), garlic (Allium sativum), angelica sinensis, papaya (Carica papaya), sage (Salvia miltiorrhiza), and reduce, for example, ginseng (Panax ginseng), St. John’s wort (Hypericum) perforatum).
You should not take warfarin and St. John’s wort preparations at the same time, since the inducing effect of warfarin on cytochrome P450 may persist for another 2 weeks after discontinuation of St. John’s wort preparations. If the patient is taking St. John’s wort preparations, the MHO should be determined and the intake should be stopped. MHO monitoring must be careful, because its value may increase when St. John’s wort preparations are discontinued. After this, warfarin can be prescribed.
The effect of warfarin may be enhanced by quinine contained in tonic drinks.
Warfarin may enhance the hypoglycemic effect of oral sulfonylurea hypoglycemic agents.
The effect of warfarin may be weakened when taken simultaneously with the following drugs: azathioprine, aminoglutethimide, ascorbic acid, barbiturates, valproic acid, menadione sodium bisulfite, glutethimide, griseofulvin, dicloxacillin, disopyramide, carbamazepine, cholestyramine, mercaptopurine, mesalazine, mianserin, mitotane, nafcillin, primidone, retinoids, ritonavir, rifampicin, rofecoxib, spironolactone, sucralfate, trazodone, ubidecarenone, phenazone, chlordiazepoxide, chlorthalidone, cyclosporine.
Taking diuretics in the case of a pronounced hypovolemic effect can lead to an increase in the concentration of blood coagulation factors, which reduces the effect of anticoagulants. In the case of combined use of warfarin with other drugs, it is necessary to carry out monitoring (MHO) at the beginning and end of treatment, and, if possible, after 2-3 weeks from the start of therapy.
Foods rich in vitamin K reduce the effect of warfarin; Decreased absorption of vitamin K caused by diarrhea or laxatives increases the effect of warfarin. The most vitamin K is found in green vegetables, so when treating with warfarin, you should eat the following foods with caution: amaranth greens, avocados, broccoli, Brussels sprouts, cabbage, canola oil, chayo leaf, onions, coriander (cilantro), cucumber peel, chicory, kiwi fruits, lettuce, mint, mustard greens, olive oil, parsley, peas, pistachios, red seaweed, spinach greens, spring onions, soybeans, tea leaves (but not tea drink), turnip greens, watercress.
Overdose
Overdose
Symptoms: bleeding.
Treatment: depending on the INR. If the INR is less than 5, skip the next dose and continue taking lower doses until the therapeutic INR value is reached. With an INR of 5-9, skip 1-2 doses and continue taking lower doses until the therapeutic INR value is reached, or skip 1 dose of warfarin and take 1-2.5 mg of menadione sodium bisulfite (vitamin K) orally. If the INR is more than 9, you should stop taking warfarin and take 3-5 mg of menadione sodium bisulfite orally. If the INR is 5-9 against the background of a planned operation, you should stop taking warfarin 24 hours before it and take 2-4 mg of menadione sodium bisulfite orally. If the INR is more than 20 or severe bleeding, warfarin should be discontinued and menadione sodium bisulfite 10 mg administered slowly intravenously, coagulation factor concentrate, fresh frozen plasma, or whole blood should be transfused. If necessary, re-introduce menadione sodium bisulfite every 12 hours.
Storage conditions
Storage conditions
Store the drug in a dry place, protected from light, at a temperature not exceeding 25C.
Manufacturer
Manufacturer
Ozon, Russia
Additional information
| Conditions of storage | The drug should be stored in a dry place protected from light at a temperature not exceeding 25C. |
|---|---|
| Manufacturer | Ozon, Russia |
| Medication form | pills |
| Brand | Ozon |
Other forms…
Related products
Buy Warfarin, tablets 2.5mg 100 pcs with delivery to USA, UK, Europe and over 120 other countries.