No products in the cart.
Verospiron, 50 mg capsules, 30 pcs.
€6.00 €5.42
Description
Pharmacodynamics
Veroshpiron is a potassium-saving, diuretic. Spironolactone is a potassium-saving diuretic, a specific aldosterone antagonist (mineralocorticosteroid hormone of the adrenal cortex) with prolonged action.
In the distal nephron, spironolactone prevents sodium and water retention by aldosterone and suppresses potassium withdrawal effect of aldosterone, reduces the synthesis of permease in aldosterone-dependent section of the collecting tubes and distal tubules.
Binding to aldosterone receptors, it increases excretion of sodium, chlorine and water ions with urine, decreases excretion of potassium ions and urea, reduces urine acidity. Increased diuresis is caused by the presence of diuretic effect, which is not constant; diuretic effect appears on the 2nd-5th day of treatment.
Pharmacokinetics
Absorption and distribution
On oral administration it is quickly and completely absorbed from the gastrointestinal tract. It is about 98% bound to plasma proteins (canrenone – 90%). Tmax of canrenone in blood plasma is 2-4 hours. After daily administration of 100 mg of spironolactone for 15 days, Cmax reaches 80 ng/ml, Tmax after another morning dose is 2-6 hours. Vd is 0.05 l/kg.
Metabolism
Spironolactone is converted to active metabolites: metabolite containing sulfur (80%) and partially to canrenone (20%). Spironolactone poorly penetrates into organs and tissues, while it and its metabolites pass through the placental barrier and canrenone into breast milk.
Elimation
Extracted by the kidneys: 50% – as metabolites, 10% – unchanged and partially through the intestine. T1/2 of spironolactone is 13-24 hours, the active metabolites – up to 15 hours.
Extraction of canrenone (mainly by kidneys) is biphasic; T1/2 in the first phase is 2-3 hours, in the second phase – 12-96 hours.
In liver cirrhosis and heart failure: T1/2 duration increases without evidence of cumulation, which is more likely in chronic renal failure and hyperkalemia.
Indications
Indications
Primary hyperaldosteronism (Conn’s syndrome) – for a short preoperative course of treatment.
To establish the diagnosis of primary hyperaldosteronism. Essential hypertension (as part of combination therapy). Edema syndrome in chronic heart failure (can be used as monotherapy and in combination with standard therapy).
Conditions in which secondary hyperaldosteronism may be detected, incl. liver cirrhosis, accompanied by ascites and/or edema, nephrotic syndrome and other conditions accompanied by edema.
Hypokalemia/hypomagnesemia (as an adjuvant for its prevention during treatment with diuretics and when it is impossible to use other methods of correcting potassium levels).
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Veroshpiron is potassium-sparing, diuretic. Spironolactone is a potassium-sparing diuretic, a specific antagonist of aldosterone (mineralocorticosteroid hormone of the adrenal cortex) with prolonged action.
In the distal parts of the nephron, spironolactone prevents the retention of sodium and water by aldosterone and suppresses the potassium-removing effect of aldosterone, reduces the synthesis of permeases in the aldosterone-dependent area of the collecting ducts and distal tubules.
By binding to aldosterone receptors, it increases the excretion of sodium, chlorine and water ions in the urine, reduces the excretion of potassium and urea ions, and reduces the acidity of urine. Increased diuresis is due to the presence of a diuretic effect, which is not constant; The diuretic effect appears on the 2nd–5th day of treatment.
Pharmacokinetics
Suction and distribution
When taken orally, it is quickly and completely absorbed from the gastrointestinal tract. Binds to plasma proteins by approximately 98% (canrenone – 90%). Tmax of canrenone in blood plasma is 2–4 hours. After daily administration of 100 mg of spironolactone for 15 days, Cmax reaches 80 ng/ml, Tmax after the next morning dose is 2–6 hours. Vd is 0.05 l/kg.
Metabolism
Spironolactone is converted into active metabolites: a metabolite containing sulfur (80%) and partially into canrenone (20%). Spironolactone penetrates poorly into organs and tissues, while it and its metabolites penetrate the placental barrier, and canrenone passes into breast milk.
Removal
Excreted by the kidneys: 50% – in the form of metabolites, 10% – unchanged and partially through the intestines. T1/2 of spironolactone – 13–24 hours, active metabolites – up to 15 hours.
Canrenone excretion (mainly by the kidneys) is biphasic, T1/2 in the first phase is 2–3 hours, in the second — 12–96 hours.
In liver cirrhosis and heart failure: the duration of T1/2 increases without signs of cumulation, the likelihood of which is higher in chronic renal failure and hyperkalemia.
Special instructions
Special instructions
Impact on the ability to drive vehicles and operate machinery
During the initial period of treatment, it is prohibited to drive a car or engage in activities that require increased concentration and speed of psychomotor reactions. The duration of restrictions is set individually.
When using Veroshpiron, a temporary increase in the level of urea nitrogen in the blood serum is possible, especially with reduced renal function and hyperkalemia. It is also possible to develop reversible hyperchloremic metabolic acidosis.
When prescribing Veroshpiron to patients with impaired renal and liver function, and elderly patients, regular monitoring of serum electrolytes and renal function is necessary.
Taking Veroshpiron makes it difficult to determine the concentration of digoxin, cortisol and adrenaline in the blood. Despite the absence of a direct effect on carbohydrate metabolism, the presence of diabetes mellitus, especially with diabetic nephropathy, requires special caution when prescribing Veroshpiron due to the possibility of developing hyperkalemia.
When treating NSAIDs while taking Veroshpiron, kidney function and blood electrolyte levels should be monitored. During treatment with Veroshpiron, you should avoid eating foods rich in potassium.
During treatment, alcohol consumption is contraindicated.
Active ingredient
Active ingredient
Spironolactone
Composition
Composition
1 capsule contains:
Active ingredient:
spironolactone – 50 mg.
Excipients:
sodium lauryl sulfate – 2.5 mg,
magnesium stearate – 2.5 mg,
corn starch – 42.5 mg,
lactose monohydrate – 127.5 mg.
Composition of hard gelatin capsule:
cap – quinoline yellow dye (E104) – 0.48%,
titanium dioxide (E171) – 2%,
gelatin – up to 100%;
body – titanium dioxide (E171) – 2%,
gelatin – up to 100%.
Pregnancy
Pregnancy
Contraindicated. If it is necessary to use the drug during lactation, breastfeeding should be discontinued.
Contraindications
Contraindications
Pregnancy. Lactation period (breastfeeding). Children under 3 years of age. Addison’s disease. Hyperkalemia. Hyponatremia. Severe renal failure (creatinine clearance less than 10 ml/min). Anuria.
Lactose intolerance, lactase deficiency, glucose/galactose malabsorption syndrome. Hypersensitivity to the components of the drug.
With caution: the drug should be prescribed for hypercalcemia, metabolic acidosis, AV block (hyperkalemia contributes to its intensification), diabetes mellitus (with confirmed or suspected chronic renal failure), diabetic nephropathy, surgical interventions, taking medications that cause gynecomastia, local and general anesthesia, menstrual disorders, breast enlargement, liver failure, liver cirrhosis, as well as elderly patients.
Side Effects
Side Effects
Allergic reactions: urticaria; rarely – maculopapular and erythematous rash, drug fever, itching. Dermatological reactions: alopecia, hypertrichosis.
From the urinary system: acute renal failure.
From the musculoskeletal system: muscle spasms, cramps of the calf muscles.
From the digestive system: nausea, vomiting, diarrhea, ulceration and bleeding from the gastrointestinal tract, gastritis, intestinal colic, abdominal pain, constipation, impaired liver function.
From the central nervous system and peripheral nervous system: ataxia, lethargy, dizziness, headache, drowsiness, lethargy, confusion.
From the hematopoietic system: agranulocytosis, thrombocytopenia, megaloblastosis.
From the metabolic side: hyperuricemia, hypercreatininemia, increased urea concentration, hyperkalemia, hyponatremia, metabolic hyperchloremic acidosis or alkalosis.
From the endocrine system: deepening of the voice, in men – gynecomastia (the likelihood of development depends on the dose, duration of treatment and is usually reversible and disappears after discontinuation of Veroshpiron, only in rare cases the mammary gland remains slightly enlarged), decreased potency and erection; in women – menstrual irregularities, dysmenorrhea, amenorrhea, metrorrhagia during menopause, hirsutism, pain in the mammary glands, breast carcinoma (no connection with taking the drug has been established).
Interaction
Interaction
Fludrocortisone causes a paradoxical increase in tubular secretion of potassium. Reduces the effect of mitotane. Enhances the effect of triptorelin, buserelin, gonadorelin.
Veroshpiron reduces the effect of anticoagulants, indirect anticoagulants (heparin, coumarin derivatives, indanedione) and the toxicity of cardiac glycosides (since normalizing the level of potassium in the blood prevents the development of toxicity). Enhances the metabolism of phenazole. Reduces the sensitivity of blood vessels to norepinephrine (requires caution during anesthesia). Increases T1/2 of digoxin, so digoxin intoxication is possible.
Strengthens the toxic effect of lithium due to a decrease in its clearance. Accelerates the metabolism and excretion of carbenoxolone. Carbenoxolone promotes sodium retention by spironolactone. GCS and diuretics (benzothiazine derivatives, furosemide, ethacrynic acid) enhance and accelerate the diuretic and natriuretic effects.
Enhances the effect of diuretic and antihypertensive drugs. GCS enhance the diuretic and natriuric effect in hypoalbuminemia and/or hyponatremia. The risk of developing hyperkalemia increases when taking Veroshpiron with potassium preparations, potassium supplements and potassium-sparing diuretics, ACE inhibitors (acidosis), angiotensin II antagonists, aldosterone blockers, indomethacin, cyclosporine.
Salicylates and indomethacin reduce the diuretic effect. Ammonium chloride and cholestyramine contribute to the development of hyperkalemic metabolic acidosis.
Overdose
Overdose
Symptoms: diarrhea, skin rash, hyperkalemia (paresthesia, muscle weakness, arrhythmias), nausea, vomiting, dizziness, decreased blood pressure, hyponatremia (dry mouth, thirst, drowsiness), hypercalcemia, dehydration, increased urea concentration.
Treatment: gastric lavage, symptomatic treatment of dehydration, arterial hypotension.
In case of hyperkalemia, it is necessary to normalize water-electrolyte metabolism with the help of potassium-removing diuretics, rapid parenteral administration of a dextrose solution (5-20% solutions) with insulin at the rate of 0.25-0.5 units per 1 g of dextrose; if necessary, dextrose can be reintroduced. In severe cases, hemodialysis is performed.
Storage conditions
Storage conditions
Store out of the reach of children at a temperature not exceeding 30°C.
Shelf life
Shelf life
5 years
Manufacturer
Manufacturer
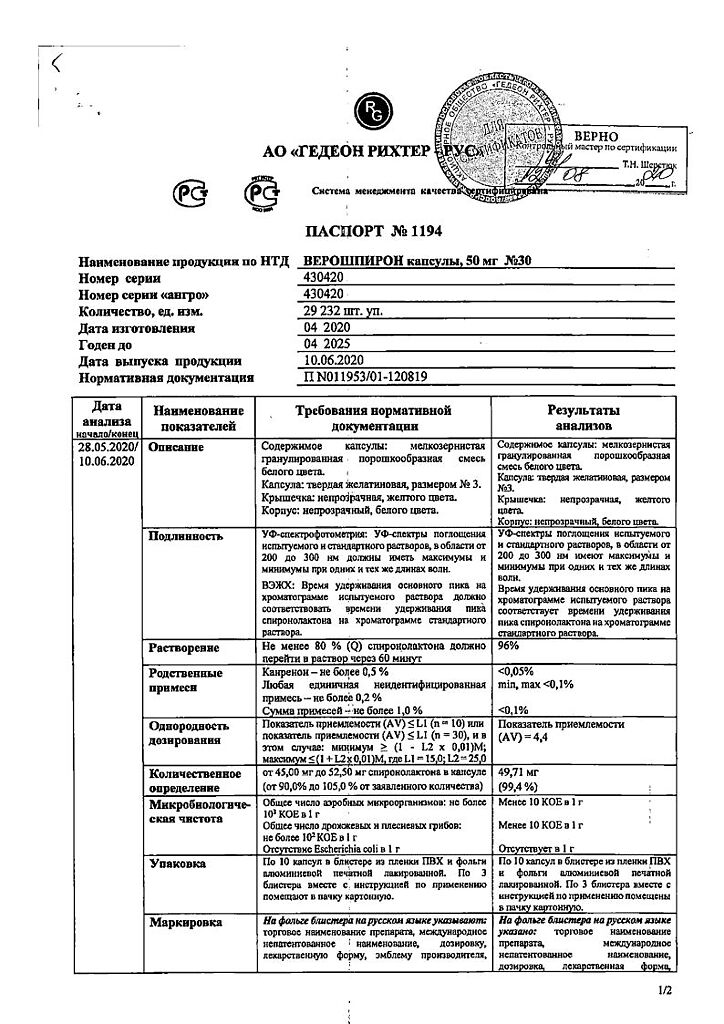
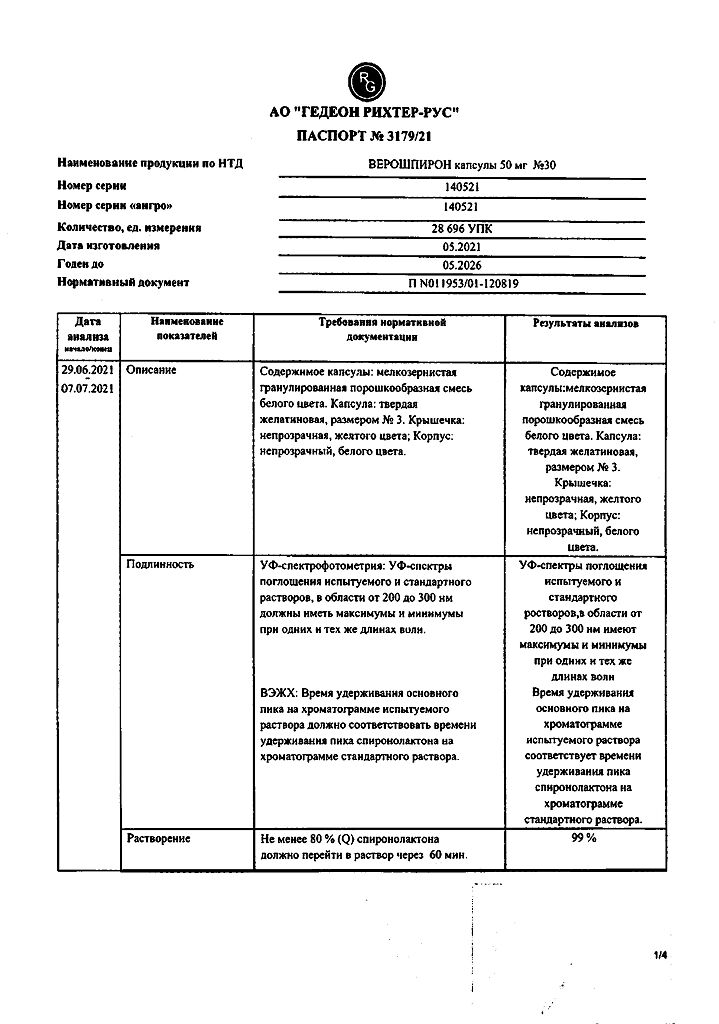
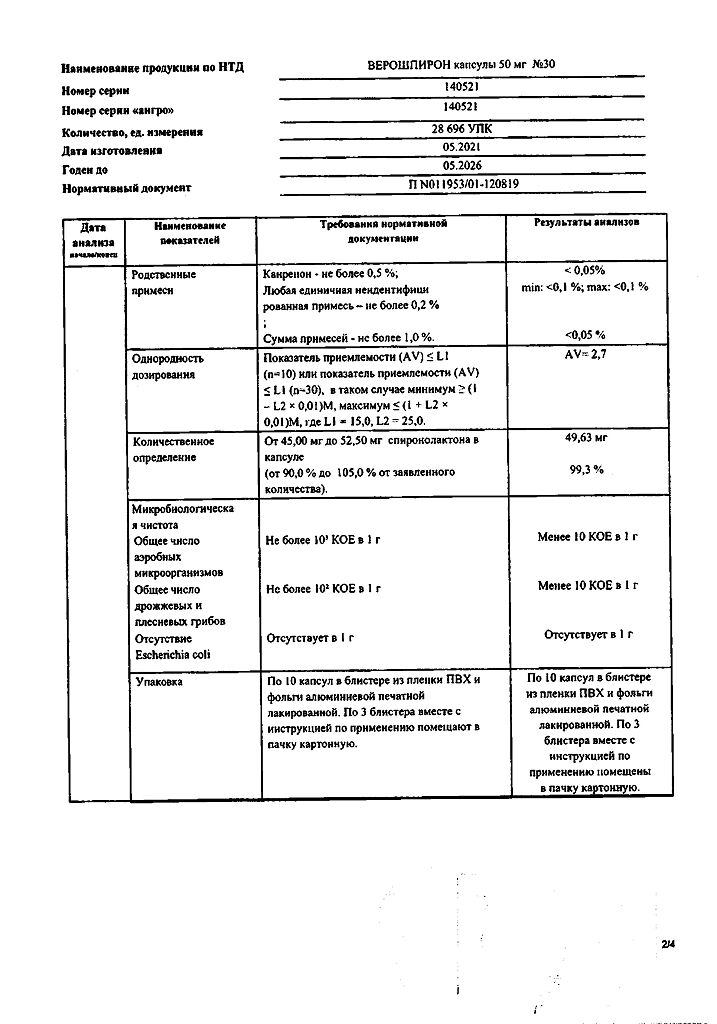
Gedeon Richter-RUS, Russia
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | Keep out of reach of children at temperatures under 30 ° C. |
| Manufacturer | Gedeon Richter, Hungary |
| Medication form | capsules |
| Brand | Gedeon Richter |
Other forms…
Related products
Buy Verospiron, 50 mg capsules, 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.