No products in the cart.
Velaksin, tablets 37.5 mg 28 pcs
€28.73 €23.94
Out of stock
(E-mail when Stock is available)
Description
Pharmacodynamics
The mechanism of antidepressant effects of Velaksin is related to its ability to potentiate the transmission of the nerve impulse in the central nervous system. Venlafaxine and its main metabolite O-desmethylvenlafaxine (ODV) are strong serotonin and noradrenaline reuptake inhibitors and weak dopamine reuptake inhibitors. Venlafaxine has no vehicle to muscarinic, cholinergic, histamine (H1) and 1-adrenergic brain receptors.
Venlafaxine does not inhibit monoamine oxidase (MAO) activity. It has no affinity for opiate, benzodiazepine, phencyclidine or N-methyl-d-aspartate (NMDA) receptors.
Pharmacokinetics
After a single dose of 250-150 mg, maximum plasma concentration is reached within 2.4 hours. It is subjected to intensive metabolism during the first passage through the liver.
Half-life of venlafaxine its main metabolite EFA is 5 and 11 hours respectively. Maximum plasma concentration of EFA is reached 4.3 hours after administration. Binding of venlafaxine and EFA to plasma proteins is 27% and 30%, respectively. EFA and other metabolites, as well as unmetabolized venlafaxine, are excreted in batches. When administered repeatedly, equilibrium concentrations of venlafaxine and EFA are reached within 3 days. In the daily dose range of 75-150 mg, venlafaxine and EFA have linear kinetics. In patients with cirrhosis, plasma concentrations of venlafaxine and EFA are elevated and their elimination rate is reduced. In patients with moderate or severe renal impairment (creatinine clearance below 30 ml/min), total clearance of venlafaxine and EFA is decreased and the elimination half-life is prolonged. Patient age and gender do not affect the pharmacokinetics of the drug.
Indications
Indications
Depression of various etiologies, treatment and prevention
Pharmacological effect
Pharmacological effect
Pharmacodynamics
The mechanism of the antidepressant effect of the drug Velaxin is associated with its ability to potentiate the transmission of nerve impulses in the central nervous system. Venlafaxine and its main metabolite O-desmethylvenlafaxine (ODV) are strong serotonin and norepinephrine reuptake inhibitors and weak dopamine reuptake inhibitors. Venlafaxine does not act on muscarinic, cholinergic, histamine (H1) and 1-adrenergic receptors in the brain.
Venlafaxine does not inhibit monoamine oxidase (MAO) activity. Has no affinity for opiate, benzodiazepine, phencyclidine, or N-methyl-d-aspartate (NMDA) receptors.
Pharmacokinetics
After a single dose of 250-150 mg, the maximum concentration in the blood plasma is achieved within 2.4 hours. Subject to intensive metabolism during the first passage through the liver.
The half-life of venlafaxine, its main metabolite EDV, is 5 and 11 hours, respectively. The maximum concentration of EDV in blood plasma is achieved 4.3 hours after administration. The binding of venlafaxine and EDV to plasma proteins is 27% and 30%, respectively. EDV and other metabolites, as well as unmetabolized venlafaxine, are released in batches. With repeated administration, equilibrium concentrations of venlafaxine and EDV are achieved within 3 days. In the range of daily doses of 75-150 mg, venlafaxine and EDV have linear kinetics. In patients with liver cirrhosis, plasma concentrations of venlafaxine and EDV are increased, and their elimination rate is reduced. In moderate or severe renal failure (creatinine clearance below 30 ml/min), the total clearance of venlafaxine and EDV is reduced and the half-life is prolonged. The age and gender of the patient do not affect the pharmacokinetics of the drug.
Special instructions
Special instructions
Depression increases the risk of suicidal thoughts and suicide attempts. This risk persists until stable remission occurs. Therefore, patients should be under constant medical supervision and should be given only small quantities of the drug capsules to reduce the risk of possible abuse and/or overdose.
Velaxin should not be used in the treatment of children and adolescents under 18 years of age. Increases in the likelihood of suicidal behavior (suicide attempt and suicidal ideation) and hostility in clinical trials were observed more often among children and adolescents receiving antidepressants compared with groups receiving placebo.
Aggressive behavior has been reported while taking venlafaxine (especially at the beginning of treatment and after discontinuation of the drug).
The use of venlafaxine may cause psychomotor restlessness, which clinically resembles akathisia, characterized by restlessness with a need to move, often combined with an inability to sit or stand still. This is most often observed during the first few weeks of treatment. If these symptoms occur, increasing the dose may have an adverse effect, and continued use of the drug should be considered.
Like all antidepressants, venlafaxine should be prescribed with caution to patients with a history of mania and/or hypomania, because the drug may cause an increase in their symptoms. In these cases, medical supervision is necessary.
Caution should be exercised when treating patients with a history of seizures. If convulsive seizures occur or their frequency increases, treatment with venlafaxine should be interrupted.
Like selective serotonin reuptake inhibitors, venlafaxine should be used with caution when used concomitantly with antipsychotic drugs, because Symptoms resembling neuroleptic malignant syndrome may develop.
Patients should be warned to seek immediate medical attention if rash, hives, or other allergic reactions occur.
Some patients experienced a dose-dependent increase in blood pressure while taking venlafaxine, and therefore regular blood pressure monitoring is recommended, especially at the beginning of treatment or when the dose is increased.
Isolated cases of orthostatic hypotension have been described while taking venlafaxine. Patients, especially the elderly, should be warned about the possibility of dizziness and impaired balance.
Venlafaxine may cause an increase in heart rate, especially at high doses. Particular caution should be exercised when prescribing the drug to patients with conditions that may be aggravated by an increase in heart rate.
There are insufficient studies of the use of venlafaxine in patients who have recently suffered a myocardial infarction or suffering from decompensated heart failure, so this drug should be used with caution in these patients.
Like other serotonin reuptake inhibitors, venlafaxine may increase the risk of bleeding into the skin and mucous membranes, so caution is required when treating patients predisposed to bleeding.
While taking venlafaxine, especially in conditions of dehydration or decreased blood volume (including in elderly patients and patients taking diuretics), hyponatremia and/or syndrome of insufficient ADH secretion may occur.
Cases of mydriasis have been reported while taking venlafaxine, so patients with a predisposition to increased intraocular pressure or those at risk of angle-closure glaucoma require careful medical monitoring.
In case of renal and liver failure, special caution is required. In some cases, a dose reduction is required.
Safety and effectiveness of using venlafaxine with drugs that reduce body weight, incl. phentermine have not been established, so their simultaneous use (as well as the use of venlafaxine as monotherapy for weight loss) is not recommended. Clinically significant increases in serum cholesterol levels have been observed in some patients receiving venlafaxine for at least 4 months. Therefore, when taking the drug for a long time, it is advisable to monitor serum cholesterol levels.
After stopping the drug, especially abruptly, withdrawal symptoms often occur. The risk of withdrawal symptoms may depend on several factors, including: duration of the course and dose, as well as the rate of dose reduction. Withdrawal symptoms, such as dizziness, sensory disturbances (including paresthesias and electrical sensations), sleep disturbances (including insomnia and unusual dreams), agitation or anxiety, nausea and/or vomiting, tremors, sweating, headache, diarrhea, rapid or increased heart rate, and emotional lability, are usually mild to moderate in severity, but may occur in some patients. may be heavy. They are usually observed in the first days after discontinuation of the drug, although there have been isolated reports of such symptoms in patients who accidentally missed a dose. Usually these phenomena resolve on their own within 2 weeks; however, in some patients they may be longer lasting (2–3 months or more). Therefore, before discontinuing venlafaxine, it is recommended to gradually reduce the dose over several weeks or months, depending on the patient’s condition.
Impact on the ability to drive a car or perform work that requires increased speed of physical and mental reactions. It should be taken into account that any drug therapy with psychoactive drugs may reduce the ability to make judgments, think or perform motor functions. The patient should be warned about this before starting treatment. If such effects occur, the degree and duration of restrictions should be determined by a physician.
Active ingredient
Active ingredient
Venlafaxine
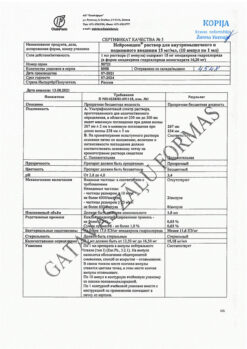
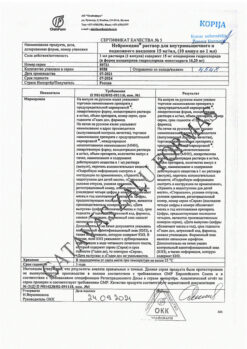
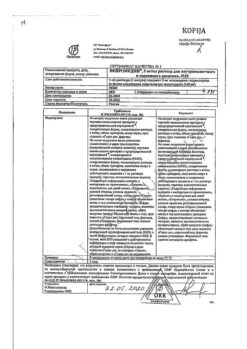
Composition
Composition
1 tablet contains:
active ingredient: venlafaxine 37.5 mg (in the form of venlafaxine hydrochloride),
excipients: lactose monohydrate, microcrystalline cellulose, sodium starch glycolate, colloidal anhydrous silicon dioxide, magnesium stearate
Pregnancy
Pregnancy
The safety of venlafaxine during pregnancy has not been proven, so use during pregnancy (or intended pregnancy) is only possible if the potential benefit to the mother outweighs the possible risk to the fetus. Women of childbearing age should be warned about this before starting treatment and should immediately consult a doctor if they become pregnant or plan to become pregnant during treatment with the drug.
Venlafaxine and EDV are excreted into breast milk. The safety of these substances for newborns has not been proven, so taking venlafaxine during breastfeeding is not recommended. If it is necessary to take the drug during lactation, the issue of stopping breastfeeding should be decided. If maternal treatment was completed shortly before delivery, the newborn may experience drug withdrawal symptoms.
Contraindications
Contraindications
hypersensitivity to any component of the drug Velaxin;
simultaneous use of MAO inhibitors;
severe renal and/or liver dysfunction (glomerular filtration rate (GFR) less than 10 ml/min, PT more than 18 s);
age under 18 years (safety and effectiveness for this age group have not been proven);
pregnancy or suspected pregnancy;
lactation period (there is insufficient data from controlled studies).
With caution: recent myocardial infarction, unstable angina, heart failure, coronary artery disease, ECG changes, incl. prolongation of the QT interval, electrolyte imbalance, arterial hypertension, tachycardia, history of seizures, intraocular hypertension, angle-closure glaucoma, history of manic states, predisposition to bleeding from the skin and mucous membranes, initially reduced body weight.
Side Effects
Side Effects
Most of the side effects listed below are dose dependent. With long-term treatment, the severity and frequency of most of these effects decreases, and there is no need to discontinue therapy.
General symptoms: weakness, fatigue.
From the gastrointestinal tract: loss of appetite, constipation, nausea, vomiting, dry mouth.
Metabolism: increased serum cholesterol levels, decreased body weight.
From the cardiovascular system: arterial hypertension. hyperemia of the skin.
From the nervous system: unusual dreams, dizziness, insomnia, increased excitability, paresthesia, stupor, increased muscle tone, tremor, yawning.
From the genitourinary system: disorders of ejaculation, erection, anorgasmia, dysuric disorders.
From the senses: disturbances of accommodation, mydriasis, visual impairment.
From the skin: sweating.
After abrupt discontinuation of venlafaxine or a reduction in its dose, the following may be observed: fatigue, drowsiness, headache, nausea, vomiting, anorexia, dry mouth, dizziness, diarrhea, insomnia, anxiety, increased irritability, sweating. These symptoms are usually mild and go away without treatment. Because these symptoms are likely to occur, it is very important to gradually reduce the dose of the drug.
Interaction
Interaction
The simultaneous use of MAO inhibitors and venlafaxine is contraindicated. Taking Velaxin can be started no less than 14 days after the end of therapy with MAO inhibitors. If a reversible MAO inhibitor (moclobemide) was used, this interval may be shorter (24 hours). Therapy with MAO inhibitors can be started no less than 7 days after discontinuation of Velaxin.
Concomitant use of venlafaxine with lithium may increase the level of the latter.
When used simultaneously with imipramine, the pharmacokinetics of venlafaxine and EDV do not change. At the same time, their simultaneous use enhances the effects of desipramine, the main metabolite of imipramine, and its other metabolite, 2-OH-imipramine, although the clinical significance of this phenomenon is unknown.
Haloperidol: Concomitant use increases haloperidol blood levels and enhances its effects.
When used simultaneously with diazepam, the pharmacokinetics of the drugs and their main metabolites do not change significantly. There was also no effect on the psychomotor and psychometric effects of diazepam.
When used simultaneously with clozapine, an increase in its level in the blood plasma and the development of side effects (for example, seizures) may be observed.
When used simultaneously with risperidone (despite the increase in AUC of risperidone), the pharmacokinetics of the sum of the active components (risperidone and its active metabolite) does not change significantly.
The decrease in mental and motor activity under the influence of alcohol did not increase after taking venlafaxine. Despite this, as in the case of taking other drugs that affect the central nervous system, the consumption of alcoholic beverages is not recommended during venlafaxine therapy.
While taking venlafaxine, special caution should be exercised during electroconvulsive therapy, because There is no experience with the use of venlafaxine in these conditions.
Drugs metabolized by cytochrome P450 isoenzymes: the cytochrome P450 enzyme CYP2D6 converts venlafaxine to the active metabolite EDV. Unlike many other antidepressants, the dose of venlafaxine does not need to be reduced when coadministered with drugs that inhibit CYP2D6 activity, or in patients with a genetically determined decrease in CYP2D6 activity, since the total concentration of venlafaxine and EDV will not change.
The main route of elimination of venlafaxine involves metabolism by CYP2D6 and CYP3A4; therefore, special caution should be exercised when prescribing venlafaxine in combination with drugs that inhibit both of these enzymes. Such drug interactions have not yet been studied.
Venlafaxine is a relatively weak inhibitor of CYP2D6 and does not suppress the activity of the CYP1A2, CYP2C9 and CYP3A4 isoenzymes; therefore, it should not be expected to interact with other drugs that are metabolized by these liver enzymes.
Cimetidine inhibits the first-pass metabolism of venlafaxine and does not affect the pharmacokinetics of EDV. In most patients, only a slight increase in the overall pharmacological activity of venlafaxine and EDV is expected (more pronounced in elderly patients and with impaired liver function).
Clinical studies have not revealed clinically significant interactions of venlafaxine with antihypertensive (including beta-blockers, ACE inhibitors and diuretics) and antidiabetic drugs.
Drugs bound to plasma proteins: Plasma protein binding is 27% for venlafaxine and 30% for EFA, so drug interactions due to protein binding should not be expected.
When taken simultaneously with warfarin, the anticoagulant effect of the latter may be enhanced, while the PT is prolonged and the MHO increases.
When taken simultaneously with indinavir, the pharmacokinetics of indinavir changes (with a 28% decrease in AUC and a 36% decrease in Cmax), but the pharmacokinetics of venlafaxine and EDV do not change. However, the clinical significance of this effect is unknown.
Overdose
Overdose
Symptoms: ECG changes (prolongation of the QT interval, bundle branch block, expansion of the QRS complex), sinus or ventricular tachycardia, bradycardia, arterial hypotension, convulsive states, depression of consciousness (decreased level of wakefulness). Death has been reported in cases of overdose of venlafaxine when taken concomitantly with alcohol and/or other psychotropic drugs.
Treatment: symptomatic. Specific antidotes are unknown. Continuous monitoring of vital functions (respiration and circulation) is recommended. Prescribing activated carbon to reduce drug absorption. Inducing vomiting is not recommended due to the risk of aspiration. Venlafaxine and EDV are not eliminated by dialysis.
Storage conditions
Storage conditions
In a dry place, at temperatures below 30°C.
Shelf life
Shelf life
5 years.
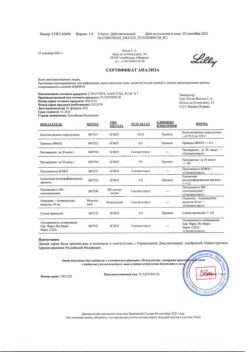
Manufacturer
Manufacturer
EGIS, Hungary
Additional information
| Shelf life | 5 years. |
|---|---|
| Conditions of storage | In a dry place, at a temperature below 30°C. |
| Manufacturer | EGIS, Hungary |
| Medication form | pills |
| Brand | EGIS |
Related products
Buy Velaksin, tablets 37.5 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.