No products in the cart.
Velafax, tablets 37.5 mg 28 pcs
€26.55 €22.12
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: antidepressant
Code ATX: N06AX16
Pharmacological properties
Pharmacodynamics. An antidepressant that is not chemically related to any known class of antidepressants (tricyclic, tetracyclic or other). It is a racemate of two active enantiomers. The antidepressant effect of venlafaxine is related to its ability to potentiate nerve impulse transmission in the CNS. Venlafaxine and its main metabolite O-desmethylvenlafaxine (ODV) are potent inhibitors of serotonin and noradrenaline reuptake by neurons and weakly inhibit dopamine reuptake. Venlafaxine and EFA reduce CNS beta-adrenergic reactivity both after a single dose and with continuous administration.
Venlafaxine has no affinity for m-cholinergic, H1-histamine and α1-adrenergic receptors in the brain. It does not inhibit the activity of MAOIs. The drug does not affect norepinephrine release from brain tissue.
Pharmacokinetics. After oral administration venlafaxine is well absorbed from the gastrointestinal tract. After a single dose of 25-150 mg, maximum plasma concentrations (Cmax) are reached within approximately 2.4 hours and are 33-172 ng/mL. After taking the drug with meals, the time to reach maximum plasma concentrations is increased by 20-30 minutes, but the values of maximum concentration and absorption do not change.
Venlafaxine undergoes intensive metabolism during “first passage” through the liver. The main metabolite is O-desmethylvenlafaxine (ODV). Maximum plasma concentration of EFA is reached approximately 4.3 hours after administration and is 61-325 ng/ml. The pharmacokinetics of venlafaxine and EFAs are linear in the daily dose range of 75-450 mg.
The binding of venlafaxine and EFA to plasma proteins is 27% and 30%, respectively. Equilibrium concentrations (Css) of venlafaxine and EFA are reached within 3 days with multiple dosing.
The half-life (T1/2) of venlafaxine and EFA are 5 and 11 h, respectively. EFA and other metabolites, as well as unchanged venlafaxine, are excreted by the kidneys.
In patients with cirrhosis, plasma concentrations of venlafaxine and EFA are elevated and their elimination rate is reduced. In moderate to severe renal failure (creatinine clearance (CK) less than 30 ml/min), total clearance of venlafaxine and EFA is decreased and the elimination half-life is prolonged.
The patient’s age and sex have no effect on the pharmacokinetics of the drug.
Indications
Indications
Treatment of depression of various etiologies, including depression accompanied by symptoms of anxiety.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antidepressant
ATX code: N06AX16
Pharmacological properties
Pharmacodynamics. An antidepressant whose chemical structure does not belong to any known class of antidepressants (tricyclic, tetracyclic or others). It is a racemate of two active enantiomers. The antidepressant effect of venlafaxine is associated with the ability to potentiate the transmission of nerve impulses to the central nervous system. Venlafaxine and its main metabolite O-desmethylvenlafaxine (ODV) are potent neuronal serotonin and norepinephrine reuptake inhibitors and weakly inhibit dopamine reuptake. Venlafaxine and EDV reduce beta-adrenergic reactivity of the central nervous system both after a single dose and with continuous use.
Venlafaxine has no affinity for m-cholinergic, H1-histamine and α1-adrenergic receptors in the brain. Does not inhibit MAO activity. The drug does not affect the release of norepinephrine from brain tissue.
Pharmacokinetics. After oral administration, venlafaxine is well absorbed from the gastrointestinal tract. After a single dose of 25-150 mg, maximum concentrations (Cmax) in blood plasma are reached within approximately 2.4 hours and are 33-172 ng/ml. After taking the drug with food, the time to reach the maximum concentration in the blood plasma increases by 20-30 minutes, but the values of the maximum concentration and absorption do not change.
Venlafaxine undergoes extensive first-pass metabolism in the liver. The main metabolite is O-desmethylvenlafaxine (ODV). The maximum concentration of EDV in blood plasma is reached approximately 4.3 hours after administration and is 61-325 ng/ml. In the range of daily doses of 75-450 mg, the pharmacokinetics of venlafaxine and EDV are linear.
The binding of venlafaxine and EDV to plasma proteins is 27% and 30%, respectively. With repeated dosing, steady-state concentrations (Css) of venlafaxine and EDV are achieved within 3 days.
The half-life (T1/2) of venlafaxine and EDV are 5 and 11 hours, respectively. EDV and other metabolites, as well as unchanged venlafaxine, are excreted by the kidneys.
In patients with liver cirrhosis, plasma concentrations of venlafaxine and EDV are increased, and their elimination rate is reduced. In moderate to severe renal failure (creatinine clearance (CC) less than 30 ml/min), the total clearance of venlafaxine and EDV is reduced and the half-life is increased.
The age and gender of the patient do not affect the pharmacokinetics of the drug.
Special instructions
Special instructions
Depression increases the risk of suicidal thoughts and suicide attempts. This risk persists until stable remission occurs. Since improvement may not occur for the first few weeks or more of treatment, patients should be under constant medical supervision throughout this period until sustained improvement occurs. The risk of suicide attempts is highest immediately after starting the drug, but also increases again during the initial period of recovery.
Venlafaxine should not be used in the treatment of children and adolescents under 18 years of age.
In patients with a history of suicidal behavior or a tendency to develop suicidal thoughts before treatment, as well as in young adult patients, the risk of suicidal thoughts or suicide attempts is highest. Placebo-controlled clinical trials of antidepressants in adult patients with mental disorders showed an increased likelihood of suicidal behavior (suicide attempt and suicidal ideation) in persons under 25 years of age receiving antidepressants, including venlafaxine.
Patients and caregivers should be warned to monitor for suicidal ideation and to seek immediate medical attention if symptoms occur.
As with other serotonergic drugs, potentially life-threatening serotonin syndrome or neuroleptic malignant syndrome-like reactions may occur during treatment with venlafaxine.
Careful monitoring of patients undergoing concomitant therapy with venlafaxine and other drugs that can affect the serotonergic and/or dopaminergic neurotransmitter systems is recommended.
The simultaneous use of venlafaxine with serotonin precursors is not recommended.
As with treatment with other antidepressants, abrupt cessation of venlafaxine therapy – especially after using high doses of the drug – may cause withdrawal symptoms, and therefore it is recommended to gradually reduce its dose before discontinuing the drug. The risk of withdrawal symptoms depends on the dose size, duration of therapy, and the individual sensitivity of the patient. In patients with affective disorders, when treated with antidepressants (including venlafaxine), hypomanic or manic states may occur. Venlafaxine (like other antidepressants) should be prescribed with caution to patients with a history of mania (such patients require medical supervision).
Like other antidepressants, venlafaxine should be administered with caution to patients with a history of epileptic seizures. Treatment with venlafaxine should be interrupted if epileptic seizures occur. The drug should not be prescribed to patients with uncontrolled epilepsy, and patients with controlled epilepsy require careful monitoring.
The use of venlafaxine may be associated with the development of psychomotor restlessness, which clinically resembles akathisia and is characterized by a subjectively unpleasant and distressing restlessness with a need to move, often combined with an inability to sit or stand still. This condition is most often observed during the first few weeks of treatment. If such symptoms occur, increasing the dose may have an adverse effect and continued use of venlafaxine should be considered.
Patients should be warned to seek immediate medical attention if rash, hives, or other allergic reactions occur.
Some patients experienced a dose-dependent increase in blood pressure while taking venlafaxine; therefore, regular monitoring of blood pressure is recommended, especially during the period of dose selection or increase.
During treatment with the drug, an increase in heart rate is possible, especially when taken in high doses. Caution should be exercised when using the drug in patients with a tendency to tachycardia.
Patients, especially older people, should be warned about the possibility of dizziness and impaired balance (orthostatic hypotension).
In patients taking venlafaxine, changes in ECG parameters (prolongation of the PR interval, widening of the QRS complex, prolongation of the QT interval) were rarely observed.
Venlafaxine should be prescribed with caution to patients who have recently suffered a myocardial infarction and with unstable angina, since the safety of the drug in this category of patients has not been studied.
Like other serotonin reuptake inhibitors, venlafaxine may increase the risk of bleeding into the skin and mucous membranes. Caution is required when treating patients predisposed to such conditions.
While taking venlafaxine, especially in conditions of dehydration or decreased circulating blood volume (including in elderly patients and patients taking diuretics), hyponatremia and/or syndrome of insufficient secretion of antidiuretic hormone may occur.
While taking the drug, mydriasis may occur, and therefore it is recommended to monitor intraocular pressure in patients prone to increased pressure or with angle-closure glaucoma.
It is not recommended to combine venlafaxine with weight-loss drugs (including phentermine) due to the lack of data on effectiveness and safety.
Clinical studies conducted to date have not revealed tolerance or dependence on venlafaxine. Despite this, the physician should closely monitor patients for signs of drug abuse (as with other drugs that act on the central nervous system). Patients with a history of drug dependence require special monitoring.
When using venlafaxine for a long period of time, monitoring of serum cholesterol levels is required.
The drug should be prescribed with caution if liver or kidney function is impaired. Sometimes a dose reduction may be necessary.
While taking venlafaxine, special care should be taken when conducting electroconvulsive therapy, because There is no experience with the use of venlafaxine in these conditions.
Alcohol consumption is not recommended during treatment.
Aggression has been reported in a small number of patients receiving antidepressants, including venlafaxine. This has been reported during venlafaxine therapy initiation, dose changes, and treatment discontinuation.
Like other antidepressants, venlafaxine should be used with caution in patients with a history of aggression.
Dry mouth may occur while taking the drug, which may increase the risk of tooth decay. In this connection, patients should be drawn to the importance of oral hygiene.
In patients with diabetes, treatment with an SSRI or venlafaxine may result in changes in glycemic control. Dosage adjustments of insulin and/or oral antidiabetic agent may be necessary.
SSRIs/SNRIs may cause symptoms of sexual dysfunction. Long-term sexual dysfunction has been reported in which symptoms persisted despite discontinuation of SSRI/SNRI therapy.
Influence on the ability to drive vehicles and operate machinery
Venlafaxine has virtually no effect on psychomotor and cognitive functions. However, given the possibility of significant side effects from the central nervous system, during treatment with venlafaxine, care must be taken when driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Venlafaxine
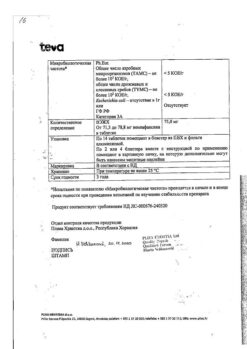
Composition
Composition
1 tablet contains: active ingredient venlafaxine hydrochloride 42.43 mg/84.86 mg (in terms of venlafaxine 37.50 mg/75.00 mg); excipients: microcrystalline cellulose (type 101), corn starch, yellow iron oxide dye (E 172), sodium carboxymethyl starch, talc, colloidal silicon dioxide, magnesium stearate.
Pregnancy
Pregnancy
During pregnancy (including before childbirth), venlafaxine is contraindicated, because The safety of its use during this period has not been determined.
Venlafaxine and the EDV metabolite are excreted in breast milk. The safety of these substances for newborns has not been proven, therefore, if it is necessary to take the drug during lactation, breastfeeding should be stopped during treatment.
Contraindications
Contraindications
Individual intolerance to venlafaxine and other components of the drug; simultaneous use of MAO inhibitors (see section “Interaction with other drugs”); age under 18 years; severe renal dysfunction (creatinine clearance less than 10 ml/min) and/or liver; pregnancy and lactation period.
With caution
Recent myocardial infarction, unstable angina, arterial hypertension, tachycardia, history of convulsive syndrome, increased intraocular pressure, closed-angle glaucoma, history of mania, hyponatremia, hypovolemia, dehydration, concomitant use of diuretics, suicidal tendencies, predisposition to bleeding from the skin and mucous membranes membranes, with initially reduced body weight.
Side Effects
Side Effects
Adverse reactions are systematized for each organ system depending on the frequency of occurrence using the World Health Organization classification: very common (≥1/10), common (≥1/100 and <1/10), uncommon (≥1/1000 and <1/100), rare (≥1/10000 and <1/1000), very rare (<1/10000), frequency unknown - cannot be estimated based on available data.
Most of the side effects listed below are dose dependent. With long-term treatment, their severity and frequency decreases, and there is usually no need to discontinue therapy.
Disorders of the blood and lymphatic system: rarely – agranulocytosis, aplastic anemia, neutropenia, pancytopenia; very rarely – thrombocytopenia.
Immune system disorders: rarely – anaphylactic reactions.
Endocrine system disorders: rarely – insufficient secretion of antidiuretic hormone; very rarely – increased plasma prolactin levels.
Metabolic and nutritional disorders: often – loss of appetite; rarely – hyponatremia.
Mental disorders: very often – insomnia; often – confusion, depersonalization, anorgasmia, unusual dreams, decreased libido, increased nervous excitability, agitation; infrequently – mania, hypomanic state, hallucinations, derealization, impaired orgasm, apathy, bruxism; rarely – delirium; frequency unknown – aggression, the appearance of suicidal thoughts and suicidal behavior during therapy and after discontinuation of the drug.
Nervous system disorders: very often – dizziness, headache, sedation; often – psychomotor restlessness/akathisia, tremor, paresthesia, dysgeusia; infrequently – syncope, myoclonus, imbalance, loss of coordination, dyskinesia; rarely – convulsions, dystonia, serotonin syndrome, neuroleptic malignant syndrome; very rarely – tardive dyskinesia.
Violations of the organ of vision: often – blurred vision, spasm of accommodation, mydriasis, deterioration of visual acuity; rarely – angle-closure glaucoma.
Hearing and labyrinthine disorders: often – noise or ringing in the ears; frequency unknown – dizziness.
Cardiac disorders: often – rapid heartbeat, tachycardia; rarely – ventricular fibrillation, ventricular tachycardia.
Vascular disorders: often – increased blood pressure, vasodilation (mainly hot flashes); infrequently – orthostatic collapse, hypotension.
Disorders of the respiratory system, chest and mediastinal organs: often – yawning, shortness of breath; rarely – interstitial lung diseases, pulmonary eosinophilia.
Gastrointestinal disorders: very often – nausea, dry mouth, constipation; often – dyspepsia, vomiting, diarrhea; uncommon – bleeding from the gastrointestinal tract; rarely – pancreatitis.
Disorders of the liver and biliary tract: infrequently – impaired liver function; rarely – hepatitis.
Disorders of the skin and subcutaneous tissues: very often – increased sweating (including night sweating); often – rash, itching; uncommon – alopecia, photosensitivity, angioedema (Quincke’s edema), urticaria, hematomas; rarely – exudative erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis.
Musculoskeletal and connective tissue disorders: often – hypertonicity; rarely – rhabdomyolysis.
Renal and urinary tract disorders: often – frequent urination, pollakuria, urinary retention; infrequently – urinary incontinence.
Disorders of the genital organs and mammary gland: often – erectile dysfunction and/or ejaculation, menorrhagia, metrorrhagia.
General disorders and disorders at the injection site: often – asthenia, fatigue, chills; very rarely – bleeding of the mucous membranes.
Laboratory and instrumental data: often – increased cholesterol levels in the blood, increased body weight, decreased body weight; rarely – prolongation of QT intervals; very rarely – prolonged bleeding time.
After abrupt discontinuation of venlafaxine or a dose reduction, increased fatigue, drowsiness, asthenia, headache, nausea, vomiting, anorexia, dry mouth, dizziness, diarrhea, insomnia, unusual dreams, difficulty falling asleep, restlessness, anxiety, irritability and emotional lability, paresthesia, confusion, disorientation, hypomania, tremor, increased sweating, tachycardia, convulsions, ringing or noise in the ears, refusal to eat. To prevent the development of withdrawal symptoms, it is very important to gradually reduce the dose of the drug, especially after taking high doses.
Interaction
Interaction
MAO inhibitors
Irreversible non-selective MAO inhibitors
Venlafaxine should not be taken in combination with irreversible, non-selective MAO inhibitors, and the interval between discontinuation of MAO inhibitor therapy and initiation of venlafaxine therapy should be at least 14 days. Venlafaxine therapy must be discontinued no later than 7 days before starting therapy with MAO inhibitors.
Reversible selective MAO inhibitors (moclobemide)
Due to the risk of developing serotonin syndrome, the combination of venlafaxine with reversible and selective MAO inhibitors such as moclobemide is not recommended. After treatment with reversible MAO inhibitors, an interval of less than 14 days may be allowed before starting venlafaxine therapy. It is recommended to discontinue venlafaxine therapy at least 7 days before starting therapy with reversible MAO inhibitors.
Reversible non-selective MAO inhibitors (linezolid)
The antibiotic linezolid is a weakly reversible and non-selective MAO inhibitor and should not be prescribed to patients taking venlafaxine.
Serious adverse reactions have been reported in patients who stopped MAO inhibitor therapy shortly before starting venlafaxine and in those who started a course of MAO inhibitors immediately after a course of venlafaxine. These side effects included tremor, myoclonus, diaphoresis, nausea, vomiting, flushing with a feeling of heat, dizziness and pyrexia with symptoms similar to those of neuroleptic malignant syndrome, as well as seizures and death.
Serotonin syndrome
Venlafaxine may affect the pharmacodynamics of other drugs acting at the level of the serotonergic neurotransmitter system, so caution should be exercised when co-prescribing it with triptans, other selective serotonin reuptake inhibitors and lithium preparations.
During concomitant treatment with venlafaxine and selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs) or serotonin receptor antagonists, it is recommended to carefully monitor the patient, especially at the beginning of therapy and when increasing the dose of the drug.
Concomitant use of venlafaxine with serotonin precursors, such as dietary supplements containing tryptophan, is not recommended.
Drugs acting on the central nervous system (CNS)
The risk of using venlafaxine in combination with other drugs acting on the central nervous system has not been studied. Caution should be exercised during therapy with venlafaxine in combination with other drugs acting on the central nervous system.
Ethanol
Concomitant use of ethanol and venlafaxine was not accompanied by a decrease in mental and motor activity. Despite this (as in the case of taking other drugs that affect the central nervous system), the use of ethanol is not recommended during venlafaxine therapy.
Drugs that prolong the QT interval
When venlafaxine is used concomitantly with other drugs that prolong the QT interval, the risk of QT prolongation and/or ventricular arrhythmias increases. The combined use of these drugs should be avoided.
Drugs that prolong the QT interval include:
class Ia and III antiarrhythmic drugs (eg, quinidine, amiodarone, sotalol, dofetilide);
some antipsychotics (eg, thioridazine);
some macrolide antibiotics (for example, erythromycin);
some antihistamines;
some quinolone antibiotics (eg, moxifloxacin).
This list is not exhaustive, so other drugs known to significantly prolong the QT interval should be avoided.
The influence of other drugs on the effects of venlafaxine
Ketoconazole (CYP3A4 inhibitor)
A pharmacokinetic study with ketoconazole in CYP2D6 extensive and poor metabolizers showed a higher area under the curve for venlafaxine (70% and 21% in poor and extensive metabolizers, respectively) and O-desmethylvenlafaxine (ODV) (33% and 23% in poor and extensive metabolizers, respectively) after administration of ketoconazole. Concomitant use of CYP3A4 inhibitors (eg, atazanavir, clarithromycin, indinavir, itraconazole, voriconazole, posaconazole, ketoconazole, nelfinavir, ritonavir, saquinavir, telithromycin) and venlafaxine may increase blood levels of venlafaxine and EDV. Caution is recommended if the patient’s therapy includes concomitant use of CYP3A4 inhibitors and venlafaxine.
The effect of venlafaxine on other medications
Drugs metabolized by cytochrome P450 isoenzymes
In vivo studies indicate that venlafaxine is a relatively weak inhibitor of CYP2D6. Venlafaxine did not inhibit CYP3A4 (alprazolam and carbamazepine), CYP1A2 (caffeine) and CYP2C9 (tolbutamide) or CYP2C19 (diazepam) in vivo.
Lithium
When venlafaxine is used concomitantly with lithium preparations, the level of lithium in the blood may increase, which can cause potentially life-threatening serotonin syndrome.
Diazepam
When used simultaneously with diazepam, the pharmacokinetics of the drugs and their main metabolites do not change significantly.
Imipramine
When used concomitantly with imipramine, the pharmacokinetics of venlafaxine and its metabolite EDV do not change. Venlafaxine does not affect the metabolism of imipramine and its metabolite 2-hydroxyimipramine, but increases the area under the pharmacokinetic curve and maximum plasma concentrations of desipramine (the main metabolite of imipramine), and also reduces the renal clearance of 2-hydroxydesipramine. The clinical significance of this phenomenon is unknown. Caution should be exercised when co-administering venlafaxine with imipramine.
Haloperidol
Venlafaxine reduces the renal clearance of haloperidol by 42%, while the area under the pharmacokinetic curve and Cmax increase by 70% and 88%, respectively. The effects of haloperidol may be enhanced.
Risperidone
When used simultaneously with risperidone, despite an increase in the area under the pharmacokinetic curve of the drug, the pharmacokinetics of the sum of the active components (risperidone and its active metabolite) did not change significantly.
Metoprolol
Coadministration of venlafaxine and metoprolol to healthy volunteers in a pharmacokinetic interaction study of the two drugs resulted in an increase in plasma concentrations of metoprolol by 30-40% without changes in the concentration of its active metabolite α-hydroxymetoprolol. The clinical significance of this result in patients with hypertension is unknown. Metoprolol did not change the pharmacokinetic profile of venlafaxine or its active metabolite EDV. Caution should be exercised when taking venlafaxine and metoprolol together.
Indinavir
When taken simultaneously with indinavir, there is a decrease in the area under the pharmacokinetic curve of indinavir by 28% and a decrease in its maximum concentration in blood plasma by 36%, while the pharmacokinetic parameters of venlafaxine and EDV do not change. The clinical significance of this effect is unknown.
Oral contraceptives
During post-marketing experience, unintended pregnancies have been reported in patients taking oral contraceptives during treatment with venlafaxine. There is no convincing evidence that these pregnancies were the result of drug interactions with venlafaxine. Interaction studies with hormonal contraceptives have not been conducted.
Warfarin
When used simultaneously with warfarin, the anticoagulant effect of the latter may be enhanced, while prothrombin time, expressed through INR (international normalized ratio), is prolonged.
Cimetidine
Cimetidine suppresses the metabolism of venlafaxine during the “first pass” through the liver and has no effect on the pharmacokinetics of EDV. In most patients, only a slight increase in the pharmacological activity of venlafaxine and EDV is expected (more pronounced in elderly patients and with impaired liver function). In elderly patients and in patients with impaired liver function, the simultaneous use of cimetidine and venlafaxine should be carried out under medical supervision.
Antihypertensive and hypoglycemic drugs
No clinically significant interaction of venlafaxine with antihypertensive (including beta-blockers, angiotensin-converting enzyme inhibitors and diuretics) and hypoglycemic drugs was found.
A potential interaction between venlafaxine and drugs that inhibit the activity of the CYP2D6 isoenzyme cannot be excluded. Caution should be exercised when using Velafax® simultaneously with these drugs (for example, quinidine, paroxetine, fluoxetine, fluvoxamine, perphenazine, haloperidol, levomepromazine).
Overdose
Overdose
Symptoms (often occur with concomitant use of ethanol): dizziness, decreased blood pressure, ECG changes (prolongation of the QT interval, bundle branch block, widening of the QRS complex), sinus and ventricular tachycardia or bradycardia, disturbances of consciousness (from drowsiness to coma), convulsions, death.
Treatment is symptomatic, under continuous monitoring of ECG and vital organ functions. Inducing vomiting is not recommended due to the risk of aspiration. It is recommended to ensure a patent airway, adequate pulmonary ventilation and oxygenation. Hemodialysis is ineffective – venlafaxine and EDV are not removed by dialysis. Specific antidotes are unknown.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25º C.
KEEP OUT OF REACH OF CHILDREN!
Shelf life
Shelf life
3 years.
Do not use after expiration date.
Manufacturer
Manufacturer
Pliva Hrvatska d.o.o., Croatia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25º C. KEEP OUT OF REACH OF CHILDREN! |
| Manufacturer | Pliva Hrvatska d.o.o., Croatia |
| Medication form | pills |
| Brand | Pliva Hrvatska d.o.o. |
Other forms…
Related products
Buy Velafax, tablets 37.5 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.