Subtotal: €19.26
Vasilip, 20 mg 28 pcs.
€6.43 €5.63
Hypolipidemic drug from the group of statins, HMG-CoA reductase inhibitor. It is a prodrug because it has in its structure a closed lactone ring, which is hydrolyzed after entering the body.
The lactone ring of statins is similar in structure to the part of the HMG-CoA reductase enzyme. By the principle of competitive antagonism, the statin molecule binds to the part of the coenzyme A receptor where this enzyme is attached. The other part of the statin molecule inhibits the conversion of hydroxymethylglutarate into mevalonate, an intermediate product in the synthesis of the cholesterol molecule. Inhibition of HMG-CoA reductase activity leads to a series of sequential reactions resulting in a decrease of intracellular cholesterol content and a compensatory increase of LDL-receptor activity and corresponding acceleration of LDL cholesterol (Xc) catabolism.
The hypolipidemic effect of statins is associated with a decrease in total Xc levels at the expense of LDL Xc. The decrease in LDL levels is dose-dependent and has an exponential rather than linear character. Statins do not affect the activity of lipoprotein and hepatic lipases, have no significant effect on synthesis and catabolism of free fatty acids, so their effect on TG level is secondary and mediated through their main effects on reduction of LDL-C level. A moderate decrease in TG levels during treatment with statins seems to be due to the expression of remnant (apo E) receptors on the surface of hepatocytes involved in catabolism of LDL, which includes approximately 30% of TG. According to controlled studies, simvastatin increases HDL-C levels by up to 14%.
In addition to hypolipidemic action, statins have a positive effect in endothelial dysfunction (preclinical sign of early atherosclerosis), on the vascular wall, atheroma condition, improve rheological properties of blood, have antioxidant, antiproliferative properties. There is evidence that simvastatin improves endothelial function already after 30 days of therapy. The use of simvastatin was accompanied by a decrease in the incidence of cardiovascular disorders regardless of the initial level of CH-LDL.
Indications
Primary hypercholesterolemia with ineffective diet therapy, combined hypercholesterolemia and hypertriglyceridemia.
Pharmacological effect
A lipid-lowering drug from the statin group, an inhibitor of HMG-CoA reductase. It is a prodrug because it has a closed lactone ring in its structure, which is hydrolyzed after entering the body.
The lactone ring of statins is similar in structure to part of the enzyme HMG-CoA reductase. According to the principle of competitive antagonism, the statin molecule binds to the part of the coenzyme A receptor where this enzyme is attached. Another part of the statin molecule inhibits the conversion of hydroxymethyl glutarate to mevalonate, an intermediate in the synthesis of the cholesterol molecule. Inhibition of the activity of HMG-CoA reductase leads to a series of sequential reactions, as a result of which the intracellular cholesterol content decreases and a compensatory increase in the activity of LDL receptors occurs and, accordingly, accelerates the catabolism of LDL cholesterol (Xc).
The lipid-lowering effect of statins is associated with a decrease in the level of total cholesterol due to LDL cholesterol. The decrease in LDL levels is dose-dependent and is not linear, but exponential. Statins do not affect the activity of lipoprotein and hepatic lipases, do not have a significant effect on the synthesis and catabolism of free fatty acids, therefore their effect on TG levels is secondary and indirect through their main effects on reducing LDL-C levels. The moderate decrease in TG levels during statin treatment appears to be associated with the expression of remnant (apo E) receptors on the surface of hepatocytes involved in the catabolism of DILI, which contain approximately 30% TG. According to controlled studies, simvastatin increases HDL-C levels by up to 14%.
In addition to the lipid-lowering effect, statins have a positive effect on endothelial dysfunction (a preclinical sign of early atherosclerosis), on the vascular wall, the condition of atheroma, improve the rheological properties of blood, and have antioxidant and antiproliferative properties. There is evidence that simvastatin improves endothelial function after 30 days of therapy. The use of simvastatin was accompanied by a decrease in the incidence of cardiovascular disorders, regardless of the initial level of LDL-C.
Special instructions
In patients with reduced thyroid function (hypothyroidism) or certain kidney diseases (nephrotic syndrome), if cholesterol levels are elevated, the underlying disease should be treated first.
In patients with severe renal failure, treatment is carried out under the monitoring of renal function.
During treatment with Vasilip®, women of reproductive age should use reliable contraception.
Treatment with simvastatin, like other HMG-CoA reductase inhibitors, can cause myopathy, sometimes leading to rhabdomyolysis with or without the development of renal failure due to myoglobinuria. The risk of developing myopathy increases with increasing doses of simvastatin and in patients with severe renal failure.
When treating with simvastatin, an increase in serum CPK levels is possible, which should be taken into account in the differential diagnosis of chest pain and after intense physical activity.
Before starting therapy with Vasilip® or increasing its dose, patients should be informed of the risk of developing myopathy and the need to immediately consult a doctor if unexplained pain, tension or weakness occurs in the muscles, especially if this is accompanied by malaise or fever.
The initial level of CPK before starting therapy should be determined in the following situations:
in elderly patients;
with kidney damage;
with decompensated hypothyroidism;
with a family history of hereditary muscle diseases;
if there is a history of toxic effects on the muscles of statins or fibrates;
with alcohol abuse.
In these cases, it is necessary to assess the possible risk and expected benefit, and clinical monitoring during therapy is recommended. If the initial CPK level is significantly elevated (more than 5 times the upper limit of normal), the measurement must be repeated after 5–7 days to confirm the results. If a significant initial increase in CPK levels is confirmed (more than 5 times the upper limit of normal), the drug is not recommended to be prescribed.
Before and during the course of treatment, the patient should be on a cholesterol-lowering diet.
During treatment with Vasilip®, if muscle pain, weakness or cramps occur, it is necessary to determine the level of CPK. The criterion for discontinuation of the drug is an increase in the CPK content in the blood serum by more than 5 times relative to the upper limit of normal. If muscle symptoms are severe and cause discomfort, even with CPK levels 5 times the upper limit of normal, treatment may need to be discontinued. If myopathy is suspected, therapy should be discontinued, regardless of the cause of the myopathy.
If symptoms resolve and CPK levels return to normal levels, a statin or an alternative drug of the same class may be reintroduced at the lowest clinically effective dose and under close medical supervision.
Therapy with Vasilip® should be temporarily discontinued several days before major surgery.
In patients with severe renal failure, treatment is carried out under the monitoring of renal function.
Measures to reduce the risk of myopathy caused by drug interactions
The risk of myopathy and rhabdomyolysis is significantly increased when simvastatin is co-administered with strong CYP3A4 inhibitors (e.g. itraconazole, ketoconazole, erythromycin, clarithromycin, telithromycin, HIV protease inhibitors, nefazodone), gemfibrozil or cyclosporine (see Interactions section). The risk of myopathy and rhabdomyolysis is also increased when fibrates are used concomitantly with high doses of niacin (>1 g/day) or when amiodarone or verapamil is used concomitantly with high doses of simvastatin (see Interactions section). The risk is also slightly increased when diltiazem is co-administered with high doses of simvastatin (80 mg).
Therefore, the use of simvastatin concomitantly with itraconazole, ketoconazole, erythromycin, clarithromycin, telithromycin, HIV protease inhibitors and nefazodone is contraindicated (see section “Contraindications”). If therapy with the listed CYP3A4 inhibitors cannot be avoided, simvastatin should be avoided. Simvastatin should also be combined with caution with certain other, less potent CYP3A4 inhibitors: cyclosporine, verapamil and diltiazem (see Interactions section).
The concomitant use of simvastatin and grapefruit juice should be avoided.
In patients taking cyclosporine, gemfibrozil or high doses of nicotinic acid (>1 g/day), the daily dose of simvastatin should not exceed 10 mg.
The simultaneous administration of simvastatin and gemfibrozil is possible only in cases where the expected benefit significantly outweighs the potential risk of such a drug combination. The benefits of combined use of simvastatin 10 mg/day and other fibrates (except fenofibrate), niacin (>1 g/day) or cyclosporine must be carefully weighed against the potential risks of such combinations.
There is a risk of myopathy when fenofibrate and simvastatin are prescribed separately, so caution is required when taking this combination simultaneously.
When taking simvastatin in doses exceeding 20 mg/day, concomitant administration of amiodarone or verapamil should be avoided unless the expected benefit outweighs the potential risk of myopathy.
Effect on the liver
Treatment with simvastatin may cause an increase in the activity of liver enzymes in the blood serum. This increase is usually small and clinically insignificant. After discontinuation of the drug, transaminase levels usually decrease slowly to baseline levels. However, before starting treatment and in the future, it is necessary to conduct a liver function test (monitor the activity of liver transaminases every 6 weeks for the first 3 months, then every 8 weeks for the remaining first year and then once every six months). If it is necessary to increase the dose to 80 mg, it is necessary to monitor liver function before increasing the dose, 3 months after the increase, and then periodically (for example, once every 6 months) during the first year of treatment. If there is a persistent increase in the activity of AST and/or ALT in the blood serum by 3 times relative to the upper limits of normal, treatment with simvastatin should be discontinued.
Prescribe with caution to persons who abuse alcohol and/or have a history of liver disease.
Impact on the ability to drive a car or perform work that requires increased speed of physical and mental reactions.
No adverse effects of Vasilip® on the ability to drive a car or use machinery have been reported. However, it should be borne in mind that isolated cases of dizziness have been reported with post-marketing use of simvastatin.
Active ingredient
Simvastatin
Composition
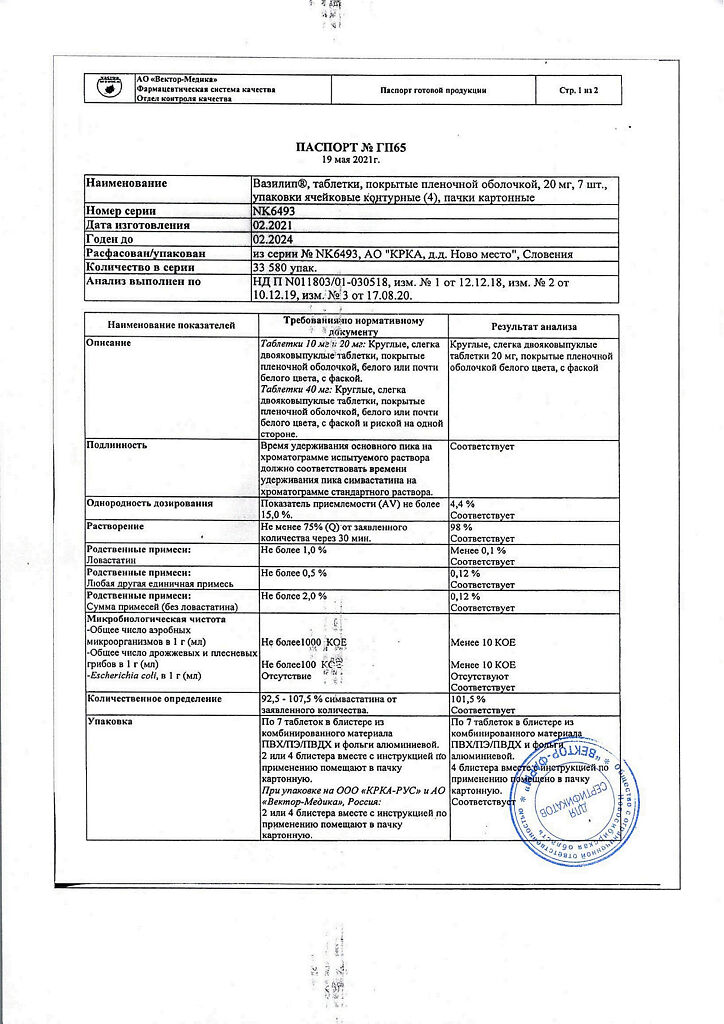
1 tablet contains:
Active substance:
simvastatin – 20 mg.
Excipients:
lactose monohydrate;
pregelatinized starch;
butylated hydroxyanisole;
anhydrous citric acid;
ascorbic acid;
corn starch;
MCC;
magnesium stearate.
Film casing:
hypromellose; talc; propylene glycol; titanium dioxide
Pregnancy
The drug is contraindicated during pregnancy. There has been no evidence of an increase in the incidence of birth defects in children whose mothers took simvastatin or another HMG-CoA reductase inhibitor. When a pregnant woman takes simvastatin, the levels of mevalonate, which is a precursor for cholesterol biosynthesis, may decrease in the fetus. Withdrawal of lipid-lowering drugs during pregnancy does not have a significant effect on the results of the short-term risk associated with primary hypercholesterolemia.
Simvastatin should not be used in pregnant women, women planning pregnancy, or suspected pregnancy. If pregnancy occurs during treatment, the drug should be discontinued and the woman warned of the possible danger to the fetus.
It is not known whether the drug is excreted into breast milk, therefore therapy with Vazilip® during breastfeeding is contraindicated.
Contraindications
Active pathological process in the liver, persistent increase in transaminase activity, pregnancy, lactation, increased sensitivity to simvastatin.
Side Effects
From the gastrointestinal tract, liver: rarely – constipation, abdominal pain, flatulence, dyspepsia, nausea, vomiting, diarrhea, pancreatitis, hepatitis, jaundice, increased activity of liver transaminases, alkaline phosphatase, creatine phosphokinase (CPK).
From the central nervous system, peripheral nervous system and sensory organs: rarely – headache, paresthesia, dizziness, peripheral neuropathy, asthenia, insomnia, convulsions, blurred vision, impaired taste.
From the musculoskeletal system: rarely – myopathy, rhabdomyolysis, myalgia, muscle weakness.
Allergic and immunopathological reactions: full-blown hypersensitivity syndrome (angioedema, lupus-like syndrome, polymyalgia rheumatica, dermatomyositis, vasculitis, thrombocytopenia, eosinophilia, increased erythrocyte sedimentation rate (ESR), arthritis, arthralgia, urticaria, photosensitivity, fever, flushing, shortness of breath and severe weakness).
Dermatological reactions: rarely – skin rash, itching, alopecia.
Other: rarely – anemia; palpitations, acute renal failure (due to rhabdomyolysis), decreased potency.
Interaction
Pharmacodynamic
The simultaneous use of simvastatin with fibrates, nicotinic acid (more than 1 g / day) increases the risk of developing myopathy, including rhabdomyolysis (with simultaneous use with fenofibrate, an increase in the risk of developing myopathy compared with monotherapy with each drug separately has not been proven). Concomitant use with gemfibrozil may lead to increased serum concentrations of simvastatin.
Pharmacokinetic
Inhibitors of cytochrome CYP3A4 (itraconazole, ketoconazole, erythromycin, clarithromycin, telithromycin, HIV protease inhibitors and nefazodone), which is involved in the metabolic transformation of simvastatin in the liver, increase the risk of developing myopathy and rhabdomyolysis during simvastatin therapy. Concomitant use with these drugs is contraindicated. Use caution when used concomitantly with less potent CYP3A4 inhibitors: cyclosporine, verapamil and diltiazem. The daily dose of simvastatin when taken simultaneously with cyclosporine should not exceed 10 mg. The daily dose of simvastatin while taking amiodarone or verapamil should not exceed 20 and 40 mg while taking diltiazem, unless the expected benefit clearly outweighs the potential risk of myopathy and rhabdomyolysis.
Simvastatin at a dose of 20–40 mg/day in volunteers and patients with hypercholesterolemia potentiates the effects of coumarin anticoagulants (for example, warfarin), in particular an increase in PT and MHO. Therefore, in patients taking coumarin anticoagulants, PT and MHO must be determined before starting simvastatin therapy, during the initial period of treatment, when changing the dose of simvastatin or discontinuing the drug. When a stable PT and MHO levels are achieved, further monitoring should be carried out at intervals recommended for patients receiving anticoagulant therapy. Simvastatin therapy does not cause changes in PT and the risk of bleeding in patients not taking anticoagulants.
Grapefruit juice inhibits CYP3A4 activity. Simultaneous intake of large amounts of grapefruit juice (more than 1 liter per day) and simvastatin leads to a significant increase in the plasma concentration of simvastatin acid. Therefore, grapefruit juice should be avoided during simvastatin therapy.
Overdose
Symptoms: There are data on several cases of simvastatin overdose. The maximum dose taken was 3.6 g.
Treatment: in case of overdose, symptomatic treatment is carried out; it is necessary to carry out general measures: monitoring and maintaining vital functions, preventing further absorption of the drug (gastric lavage, taking activated charcoal or laxatives). Monitoring liver function and CPK is recommended. There is no specific antidote.
If myopathy with rhabdomyolysis develops (a rare but severe side effect), you should immediately stop taking the drug and administer a diuretic and sodium bicarbonate to the patient (iv infusion). Rhabdomyolysis can cause hyperkalemia, which can be treated with IV calcium chloride and calcium gluconate, glucose infusion with insulin, use of potassium ion exchangers, or, in severe cases, hemodialysis.
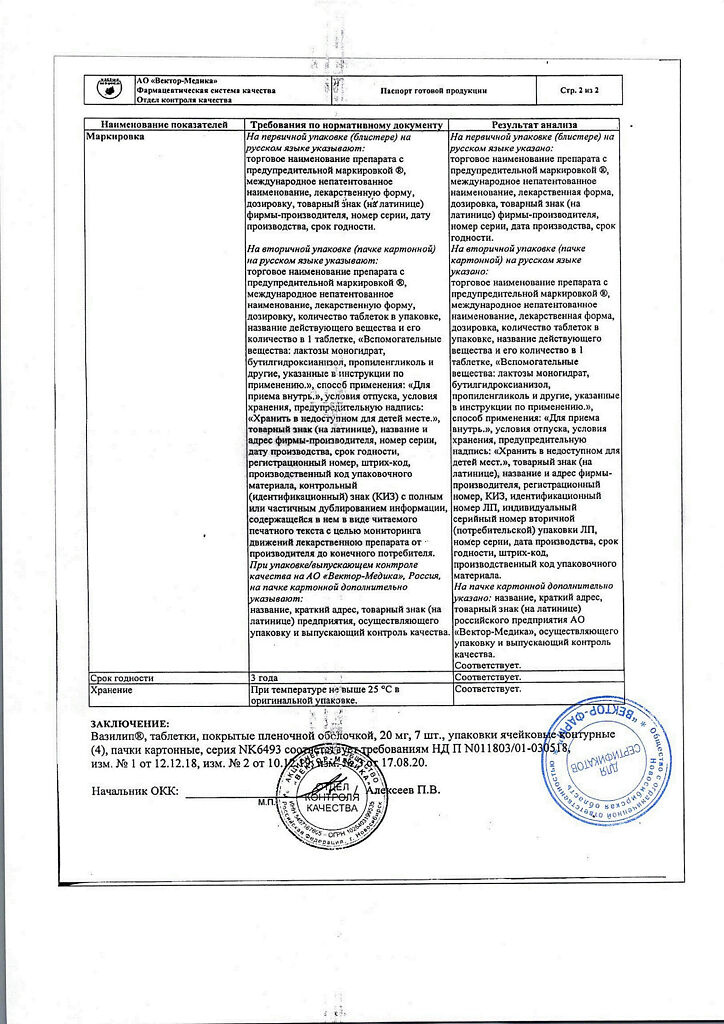
Storage conditions
At a temperature not exceeding 30 °C
Shelf life
3 years
Manufacturer
KRKA dd Novo Mesto, Slovenia
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | pills |
| Brand | KRKA dd Novo mesto |
Related products
Buy Vasilip, 20 mg 28 pcs. with delivery to USA, UK, Europe and over 120 other countries.