No products in the cart.
Valsacor H80.80 mg+12, 5 mg 90 pcs.
€26.32 €21.93
Description
hypotensive drug combined
(angiotensin II receptor antagonist + diuretic).
Indications
Indications
Arterial hypertension (patients who are indicated for combination therapy).
Active ingredient
Active ingredient
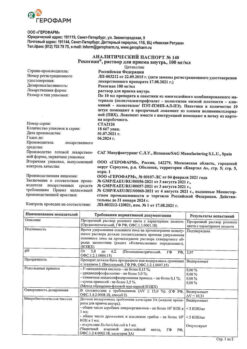
Composition
Composition
1 film-coated tablet contains:
Kernel:
Active substances:
Valsartan 80.00 mg
Hydrochlorothiazide 12.50 mg
Auxiliary substances:
Microcrystalline cellulose, croscarmellose sodium, povidone-K25, lactose monohydrate, magnesium stearate, colloidal silicon dioxide
Film coating: hypromellose 2910, titanium dioxide (E171), macrogol-4000, iron oxide red dye (E172), iron oxide yellow dye (E172)
How to take, the dosage
How to take, the dosage
Before starting therapy with the drug Valsacor® H 80, water-electrolyte disturbances should be corrected (see sections “Caution”, “Special Precautions”).
Orally, once daily, regardless of meal time, the tablet should be swallowed whole and with plenty of liquid.
The recommended daily dose is 1 tablet of Valsacor® H 80.
The dose of Valsacor® H 80 is adjusted after previously titrated doses of individual drug components. In case of insufficient antihypertensive effect the dose can be increased (not earlier than after 4-6 weeks) by titration of doses up to maximum daily dose in terms of valsartan 320 mg and up to maximum daily dose by GXTZ 25 mg.
Maximum BP reduction is usually achieved within 2-4 weeks of therapy, but in some patients within 4-8 weeks, which should be considered when titrating the dose.
Kidney function impairment
Patients with mild to moderate renal dysfunction (CK ⥠30 ml/min (0.5 ml/sec)) do not require dose adjustment of the drug.
Liver function impairment
The maximum recommended daily dose of Valsacor® H 80 in patients with mild (Child-Pugh score 5-6) or moderate (Child-Pugh score 7-9) impaired liver function without cholestasis is 1 tablet daily (80/12.5 mg).
Interaction
Interaction
General drug interactions for valsartan and hydrochlorothiazide
Simultaneous use is not recommended
Lithium preparations
When ACE inhibitors, ARA II, or thiazide diuretics are used concomitantly with lithium preparations, reversible increases in plasma lithium concentrations and the development of intoxication have been observed. The risk of toxic manifestations associated with the use of lithium preparations may be further increased when concomitant use with the drug Valsacor® H 80 because renal clearance of lithium preparations is decreased under the influence of thiazide diuretics. If it is necessary to use simultaneously with lithium preparations, the lithium concentration in blood plasma should be monitored carefully.
Simultaneous use with caution
Other hypotensive drugs
The antihypertensive effect may be enhanced when used concomitantly with other BP-lowering drugs (e.g., ACE inhibitors, beta-adrenoblockers, slow calcium channel blockers (SCBs), guanethidine, methyldopa, vasodilators, direct renin inhibitors, ARA II).
Pressor amines (for example,norepinephrine and epinephrine)
The effects of pressor amines may be attenuated without requiring discontinuation of concomitant use of valsartan and HCTZ.
Non-steroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 inhibitors (COX-2)
The simultaneous use of ARA II and COX-2 with NSAIDs may attenuate diuretic and antihypertensive effects. Under conditions of hypovolemia development of ARF is possible. It is recommended to monitor renal function at the beginning of therapy and conduct adequate replacement of the circulatory blood pressure by the patient.
Drug interactions for valsartan
Simultaneous use is contraindicated
The concomitant use of ARA II, including valsartan, with drugs containing aliskiren is contraindicated in patients with DM and/or moderate to severe renal function impairment (GFR less than 60 mL/min/1.73 m2 body surface area) and is not recommended in other patients.
Simultaneous use of ARA II with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Simultaneous use is not recommended
Kalice-saving diuretics (spironolactone, eplerenone, triamterene, amiloride), potassium preparations, potassium-containing food salt substitutes, and other drugs and substances that may cause elevated serum potassium levels (e.g., heparin)
When concomitant use with drugs that affect potassium content is necessary, it is recommended to monitor the plasma potassium content.
Simultaneous use with caution
The concomitant use of ARA II, including valsartan, with drugs that affect the RAAS, such as ACE inhibitors or aliskiren, increases the incidence of arterial hypotension, hyperkalemia, and renal function impairment. It is necessary to monitor BP, renal function, plasma electrolyte content in such patients.
Protein carriers
Studies in vitro on liver cultures have shown that valsartan is a substrate for OATP1B1/OATP1B3 and MRP2 carrier proteins. Concomitant use of valsartan with OATP1B1/OATP1B3 transporter protein inhibitors (rifampicin, cyclosporine) or MRP2 (ritonavir) may increase systemic valsartan exposure (Cmax and AUC). Caution should be exercised at the beginning of concomitant use with the above drugs or after their withdrawal.
No drug interactions
No clinically significant interactions were identified with the following drugs: cimetidine, warfarin, furosemide, digoxin, atenolol, indomethacin, HCTC, amlodipine, and glibenclamide.
Drug interactions for HCTZ
Simultaneous use with caution
Drugs affecting plasma potassium
When used concomitantly with “loop” diuretics, glucocorticosteroids (GCS), adrenocorticotropic hormone (ACTH), amphotericin B, benzathine benzylpenicillin, carbenoxolone, laxatives, acetylsalicylic acid or its derivatives the risk of plasma potassium reduction and hypokalemia increases. In this case it is recommended to monitor the potassium content in plasma.
Drugs ncapable of inducing polymorphic ventricular tachycardiatypea “pirouette”
When concomitant use of antiarrhythmic drugs IA and class III and some antipsychotic drugs (neuroleptics) with HCHTZ caution should be exercised as there is a risk of developing “pirouette” type arrhythmias against a background of possible hypokalemia. It is recommended to control potassium content in blood plasma.
Myorelaxants with non-depolarizing peripheral action (tubocurarin)
GCTZ potentiates action of muscle relaxants.
Hypoglycemic agents (oral and insulin)
Combined use may require dose adjustment of hypoglycemic agents.
Metformin should be used with caution since lactoacidosis may develop due to renal failure when taking HCTS.
Drugs that affect plasma sodium
In long-term concomitant use with antidepressants, anticonvulsants, antipsychotics (neuroleptics) (e.g., carbamazepine), etc. etc., caution should be exercised because the risk of hyponatremia increases. It is recommended to monitor sodium content in blood plasma regularly.
Heart glycosides
Hypokalemia and hypomagnesemia on thiazide diuretics may contribute to heart rhythm abnormalities in patients receiving cardiac glycosides.
H- and m-cholinoblockers
H- and m-cholinoblockers (atropine, biperiden) may increase the bioavailability of thiazide diuretics by reducing gastrointestinal (GI) peristaltic activity and slowing gastric emptying. Accordingly, gastrointestinal motility stimulators (cisapride) may decrease the bioavailability of thiazide diuretics.
Anion exchange resins (colestyramine and colestipol)
The absorption of thiazide diuretics, including HCTHZ, is reduced when colestiramine and colestipol are used simultaneously. Therefore, HCTS should be taken 4 hours or 4-6 hours after taking anion-exchange resins.
Methyldopa
Individual cases of hemolytic anemia have been described when using methyldopa and HCTS concomitantly.
Vitamin D and calcium salts
Simultaneous use of thiazide diuretics, including HCTC, with vitamin D or calcium salts may result in increased plasma calcium levels as a result of increased calcium reabsorption.
Cyclosporine
The simultaneous use of HCTC and cyclosporine increases the risk of hyperuricemia and gout-like symptoms.
Iodine contrast agents
Hypovolemia during diuretic use increases the risk of ARF. The BOD should be replenished prior to the use of agents with high iodine content (e.g., radiopaque agents containing iodine).
Gout medications (probenecid, sulfinpyrazone, and allopurinol)
The use of HCTCs may increase plasma uric acid concentrations, which may require dosage adjustments of gout medications (e.g., increasing the dose of sulfinpyrazone and probenecid). Concomitant use with thiazide diuretics, including GHTZ, may lead to an increased incidence of hypersensitivity reactions to allopurinol.
Amantadine
Simultaneous use with thiazide diuretics, including HCTC, increases the risk of amantadine side effects.
Beta-adrenoblockers and diazoxide
Concurrent use with thiazide diuretics, including HCTC, increases the risk of hyperglycemia.
Cytotoxic drugs (cyclophosphamide, methotrexate)
Simultaneous use with thiazide diuretics, including HCTC, reduces the renal excretion of cytotoxic drugs, resulting in potentiation of their myelosuppressive effects.
Ethanol, barbiturates and narcotics
Simultaneous use with thiazide diuretics, including HCTS, may potentiate orthostatic hypotension.
Directions for use
Directions for use
Special Instructions
Special Instructions
Concomitant use of potassium-saving diuretics, potassium preparations, potassium-containing supplements, or other drugs that can increase serum potassium (e.g., heparin), conditions accompanied by water-electrolyte disturbances: nephropathy with salt loss and prerenal (cardiogenic) renal dysfunction, hypokalemia, hypomagnesemia, hypercalcemia, chronic heart failure (CHF) III-IV functional class according to NYHA classification, moderately expressed liver function disorders without cholestasis phenomena, marked hyponatremia and/or conditions accompanied by a decrease in the BOD (including diarrhea, vomiting, high-dose diuretic therapy, bilateral or unilateral renal artery stenosis or stenosis of the artery of the sole kidney, post kidney transplantation, primary hyperaldosteronism, aortic and/or mitral valve stenosis, hypertrophic obstructive cardiomyopathy (HCMP), systemic lupus erythematosus (SLE), history of nonmelanoma skin cancer (NSCLC) (see sect. in patients with hereditary angioedema or angioedema against the background of previous therapy with ARA II or ACE inhibitors.
It is contraindicated in children under the age of 18 years (effectiveness and safety in children is not proven).
Kidney function impairment
Patients with mild to moderate renal dysfunction (CK ⥠30 ml/min (0.5 ml/sec)) do not require dose adjustment of the drug.
Liver function impairment
The maximum recommended daily dose of Valsacor® H 80 in patients with mild (5-6 Child-Pugh scores) or moderate (7-9 Child-Pugh scores) impaired liver function without cholestasis is 1 tablet daily (80/12.5 mg).
Double RAAS blockade
The concomitant use of ARA II, including valsartan, with drugs containing aliskiren is contraindicated in patients with DM and/or moderate to severe renal function impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
Simultaneous use of ARA II with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Renal dysfunction
In patients with impaired renal function (CKR over 30 ml/min) no change in drug dose is required. When using Valsacor® N 80 in patients with impaired renal function, it is recommended to monitor regularly potassium, creatinine and uric acid in plasma.
Condition after kidney transplantation
The safety of Valsacor® H 80 in patients who have recently undergone a kidney transplant has not been established.
Aortic and/or mitral valve stenosis, GOCMP
Valsacor® H 80 should be used with caution in patients with hemodynamically significant aortic and/or mitral valve stenosis or with GOCMP.
Liver function impairment
The drug Valsacor® H 80 is not used in patients with severe hepatic dysfunction (greater than 9 points on the Child-Pugh scale). In patients with mild or moderate hepatic impairment without cholestasis, Valsacor® H 80 should be used with caution.
Water-electrolyte balance disorders
When using thiazide diuretics, including HCTC, cases of hypokalemia, hyponatremia and hypochloremic alkalosis, hypomagnesemia (because renal excretion of magnesium increases) and hypercalcaemia (because renal calcium excretion decreases) have been reported. It is recommended to monitor serum electrolytes, especially potassium, when using Valsacor® H 80.
Hyponatremia and/or decreased OCC
In patients with severe hyponatremia and/or with decreased RBC (e.g., when taking high doses of diuretics), a significant BP decrease with clinical manifestations is possible in rare cases at the beginning of Valsacor® N 80 therapy. Therefore at the beginning of the treatment it is necessary to correct the serum sodium content and / or make up the BCCF.
In case of marked BP decrease, patient should be transferred to horizontal position with elevated legs and, if necessary, intravenous infusion of 0.9 % sodium chloride solution. After BP stabilization, the treatment with Valsacor® N 80 may be continued.
Severe CHF (III-IV functional class by NYHA) or other diseases accompanied by RAAS stimulation
In patients whose renal function depends on the state of RAAS (e.g., in CHF class III-IV according to NYHA classification), therapy with ACE inhibitors may be accompanied by oliguria and/or progressive azotemia, in rare cases – ARF. It is impossible to exclude development of renal function impairment due to inhibition of RAAS activity during Valsacor® N 80 administration. Therapy with Valsacor® H 80 should be performed with caution and under control of renal function.
Primary hyperaldosteronism
The drug Valsacor® H 80 is not effective for the treatment of AH in patients with primary hyperaldosteronism due to the lack of activation of the RAAS.
Renal artery stenosis
In patients with unilateral or bilateral renal artery stenosis or stenosis of the artery of the only kidney the drug should be used with caution due to the possible increase of creatinine and urea concentrations in plasma.
Systemic lupus erythematosus
In cases of thiazide diuretics (including HCTS), exacerbations and worsening the course of connective tissue diseases (such as SLE) are described.
Photosensitivity
Cases have been described of photosensitivity developing against HCTC administration. In case of photosensitivity development it is recommended to stop the therapy. If it is necessary to continue the therapy, it is recommended to protect exposed parts of the body from sunlight and ultraviolet (UV) rays.
NMRC
Two pharmacoepidemiological studies using data from the Danish National Cancer Registry demonstrated an association between HCTS intake and an increased risk of developing basal cell carcinoma and squamous cell carcinoma (SCC). The risk of NSCLC development increased with increasing total (cumulative) dose of HCTS. A possible mechanism of NMRK development is the photosensitizing effect of HCTS.
Patients taking HCTC as monotherapy or in combination with other medications should be aware of the risk of developing NMR. It is recommended that such patients have regular skin examinations to detect any new suspicious lesions as well as changes in existing skin lesions.
Any suspicious skin changes should be reported to the physician immediately. Suspicious skin areas should be examined by a specialist. Histological examination of skin biopsy specimens may be required to confirm the diagnosis.
Patients should be advised to follow preventive measures such as limiting exposure to sunlight and UV rays and use appropriate protective equipment to minimize the risk of developing SLE.
In patients with a history of NMR, it is recommended to reconsider the appropriateness of HCTC.
Other metabolic disorders
Thiazide diuretics, including HCTC, may cause altered glucose tolerance and increased plasma concentrations of cholesterol, triglycerides and uric acid.
Patients with diabetes may need to adjust the dose of insulin or oral hypoglycemic agents.
Thiazide diuretics reduce renal calcium excretion and may cause a slight increase in plasma calcium in the absence of concomitant calcium metabolic disorders. Severe hypercalcemia against the background of thiazide diuretic use may indicate hyperparathyroidism. Thiazide diuretics, including HCTC, should be cancelled before parathyroid function tests.
Antidoping test
The HCTS may test positive for doping controls.
Sensitivity reactions
A hypersensitivity reactions against GXTZ use were most frequently observed in patients with allergic reactions and bronchial asthma in the anamnesis.
The development of angioedema, including edema of the larynx and vocal cords leading to airway obstruction, and/or edema of the face, lips, pharynx, and/or tongue was observed in patients using valsartan. Some of these patients have a history of development of angioedema against the background of the use of other drugs, including ACE inhibitors. In case of development of angioedema, Valsacor® N 80 should be immediately discontinued and the drug should not be resumed.
An acute attack of closed-angle glaucoma
Transient myopia and acute development of closed-angle glaucoma have been reported during HCTC use. Symptoms include a sudden onset, abrupt decrease in visual acuity, or pain in the eye, usually occurring within a few hours to a week after the start of therapy. Untreated closed-angle glaucoma can lead to permanent vision loss.
The first step is to stop taking HCTCs as soon as possible. If the intraocular pressure remains uncontrolled, emergency medication or surgery may be needed. A history of allergic reactions to sulfonamides or penicillin may be a risk factor for acute angle closure glaucoma.
Special information on excipients
The drug Valsacor® H 80 contains lactose; therefore, it should not be used in the following conditions: lactose intolerance, lactase deficiency, glucose-galactose malabsorption syndrome.
Due to the possibility of dizziness or weakness when using Valsacor® H 80, caution should be exercised while driving vehicles and operating other technical devices requiring increased concentration and rapid psychomotor reaction.
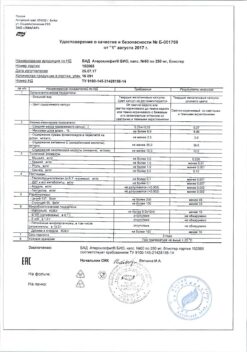
Synopsis
Synopsis
Oval, biconvex pink film-coated tablets.
Breakage appearance: white, rough mass with a pink colored film coating.
Contraindications
Contraindications
Side effects
Side effects
The frequency classification of side effects recommended by the World Health Organization (WHO):
very frequently â¥1/10
often ⥠1/100 to < 1/10
infrequently from ⥠1/1000 to < 1/100
rarely from ⥠1/10000 to < 1/1000
very rarely < 1/10000
frequency is unknown cannot be estimated from available data.
With valsartan/hydrochlorothiazide combination
Metabolic and nutritional disorders:
infrequent: dehydration.
Nervous system disorders:
often: headache;
infrequently: paresthesia;
very rare: dizziness;
frequency unknown: syncope.
Visual organ disorders:
infrequent: decreased visual acuity.
Hearing organ and labyrinth disorders:
infrequent: tinnitus.
vascular disorders:
infrequent: marked BP decrease, peripheral edema.
Disorders of respiratory system, thorax and mediastinum:
infrequent: cough;
frequency unknown: noncardiogenic pulmonary edema.
Gastrointestinal tract disorders:
infrequently: nausea;
very rarely: diarrhea.
Muscular and connective tissue disorders:
infrequently: myalgia;
very rarely: arthralgia.
Kidney and urinary tract disorders:
frequency unknown: renal dysfunction.
General disorders and disorders at the site of administration:
infrequently: increased fatigue.
Laboratory and instrumental data:
frequency is unknown: increase of uric acid concentration in serum, increase of bilirubin concentration in serum, increase of creatinine concentration in serum, hyponatremia, hypokalemia, neutropenia, increase of urea residual nitrogen concentration in serum.
The following adverse events (AEs) with no apparent association with drug intake were observed in patients with AH when studying the clinical use of the fixed valsartan/HCGTZ combination: abdominal pain, upper abdominal pain, anxiety, arthritis, asthenia, back pain, bronchitis (including acute), chest pain, postural dizziness, dyspepsia, shortness of breath, dry mouth, nasal bleeding, erectile dysfunction, gastroenteritis, headache, increased sweating, hypoesthesia, flu-like condition, insomnia sprains, muscle cramps, muscle hypertonicity, nasal congestion, nasopharyngitis, nausea, neck pain, peripheral edema, otitis media, pain in extremities, palpitations, sore throat and larynx, pyrexia, pollakiuria, hyperthermia, sinusitis, sleepiness, upper respiratory infections, urinary tract infections, vertigo, viral infections, vision disorders.
The following are the NJs associated with each component used individually.
With valsartan
Blood and lymphatic system disorders:
incidence unknown: decreased hemoglobin, decreased hematocrit, thrombocytopenia.
immune system disorders:
frequency unknown: hypersensitivity/allergic reactions, including serum sickness.
Metabolic and nutritional disorders:
frequency unknown: increased serum potassium, hyponatremia.
Hearing organ and labyrinth disorders:
infrequent: vertigo.
vascular disorders:
frequency unknown: vasculitis.
Gastrointestinal tract disorders:
infrequent: abdominal pain.
Disorders of the liver and biliary tract:
frequency unknown: increased activity of “liver” enzymes.
Skin and subcutaneous tissue disorders:
frequency unknown: angioedema, skin rash, pruritus, bullous dermatitis.
Renal and urinary tract disorders:
incidence unknown: renal failure.
The following ONs have been observed in studies of clinical use of valsartan in patients with AH regardless of their causal relationship to valsartan use: arthralgia, asthenia, back pain, diarrhea, dizziness, headache, insomnia, decreased libido, nausea, edema, pharyngitis, rhinitis, sinusitis, upper respiratory infections, viral infections.
When using thiazide diuretics, including HCTC
Blood and lymphatic system disorders:
rarely: thrombocytopenia, sometimes with purpura;
very rare: agranulocytosis, suppression of bone marrow hematopoiesis, hemolytic anemia, leukopenia;
frequency unknown: aplastic anemia.
immune system disorders:
very rare: hypersensitivity reactions.
Metabolic and nutritional disorders:
very common: hypokalemia, increased plasma lipid concentration (especially at high doses of HCTS);
Overdose
Overdose
Symptoms:The main expected manifestation of valsartan overdose is a marked decrease in BP, which may lead to impaired consciousness, collapse, and/or shock. In overdose of HCTS the following symptoms are possible: nausea, somnolence, decreased RBC, heart rhythm disturbances and muscle cramps caused by the disturbed water-electrolyte balance.
Treatment:is symptomatic and depends on the time since taking the drug and the severity of symptoms. In case of early diagnosis of overdose, it is recommended to induce vomiting and/or gastric lavage. Hemodynamic parameters should be stabilized. If BP is significantly decreased, the patient should be transferred to a horizontal position with elevated legs and make up the blood circulation (intravenous injection of 0.9% sodium chloride solution) under control of hemodynamic parameters and diuresis. Valsartan is not excreted by hemodialysis, as it is significantly bound to plasma proteins. HCTS is excreted by hemodialysis.
Pregnancy use
Pregnancy use
Pregnancy
Valsartan
PRA II use in the first trimester of pregnancy is not recommended. The use of APA II is contraindicated in II-III trimesters of pregnancy, since its use in II-III trimesters of pregnancy may cause fetotoxic effects (decreased renal function, scarcity of water, delayed ossification of fetal skull bones) and neonatal toxic effects (renal failure, arterial hypotension, hyperkalemia). There have been reports of spontaneous abortions, oligohydramnios, and renal dysfunction in infants whose mothers unintentionally received valsartan during pregnancy.
If the drug was still used in the second to third trimesters of pregnancy, then ultrasound examination of the fetal kidneys and skull bones should be performed.
If pregnancy is planned, it is recommended to switch the patient to an alternative hypotensive therapy taking into account the safety profile.
Newborns whose mothers received ARA II during pregnancy need medical monitoring because of the risk of developing arterial hypotension.
GHTZ
HCHTZ use during pregnancy, especially in the first trimester, is limited. HCTC penetrates the placenta. When thiazide diuretics are used in the II-III trimester of pregnancy, thrombocytopenia, water-electrolyte imbalance, and fetal or neonatal jaundice may develop.
If pregnancy is confirmed, Valsacor® N 80 should be discontinued as soon as possible.
Breastfeeding
There are no data on the excretion of valsartan in breast milk. HCTS is excreted with breast milk in women. If it is necessary to use Valsacor® H 80 during lactation, breastfeeding should be stopped.
Similarities
Similarities
Additional information
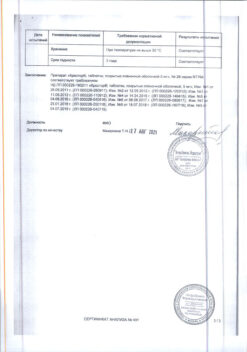
| Weight | 0.046 kg |
|---|---|
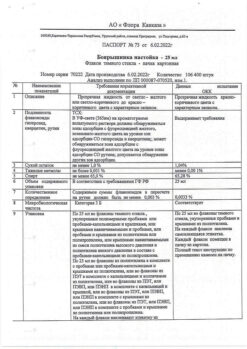
| Shelf life | 5 years. Do not use the product after the expiration date. |
| Conditions of storage | At temperature no higher than 25°C, in original packaging. Store out of the reach of children. |
| Manufacturer | KRKA-RUS, Russia |
| Medication form | pills |
| Brand | KRKA-RUS |
Related products
Buy Valsacor H80.80 mg+12, 5 mg 90 pcs. with delivery to USA, UK, Europe and over 120 other countries.