No products in the cart.
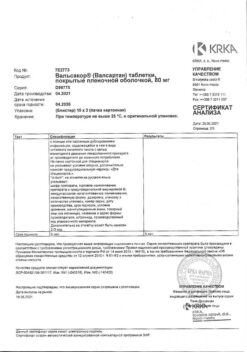
Valsacor, 320 mg 30 pcs
€18.12 €15.10
Description
Myocardial infarction, Blood pressure, Hypertension (high blood pressure), Heart failure
Patients over 18 years
- Arterial hypertension.
- Cronic heart failure (NYHA II-IV) in patients receiving standard therapy with one or more drugs from the following groups: diuretics, cardiac glycosides, and ACE inhibitors or beta-adrenoblockers. The use of each of these drugs is optional.
- All patients with acute myocardial infarction complicated by left ventricular failure and/or left ventricular systolic dysfunction have improved survival with stable hemodynamic parameters.
Patients from 6 to 18 years
- Arterial hypertension in 6- to 18-year-olds.
.
Active ingredient
Active ingredient
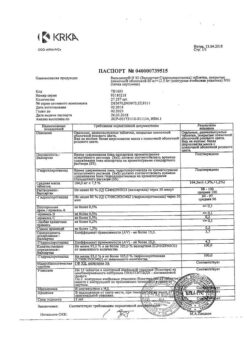
Composition
Composition
1 film-coated tablet contains:
Core:
Active substance:
Valsartan 320.00 mg
Excipients:
Lactose monohydrate, microcrystalline cellulose, povidone K-25, croscarmellose sodium, colloidal silicon dioxide, magnesium stearate
Shell film:
Hypromellose, titanium dioxide (E171), iron oxide yellow dye (E172), iron oxide red dye (E172), macrogol-4000
How to take, the dosage
How to take, the dosage
Overly, regardless of the time of meals, without chewing, once a day.
Patients over 18 years
Arterial
The use of Valsacor® is possible in doses of 40 mg, 80 mg, 160 mg, 320 mg.
The recommended starting dose is 80 mg once daily regardless of race, age or sex.The antihypertensive effect develops within 2 weeks of therapy and reaches its maximum after 4 weeks.In patients who do not achieve optimal BP control the daily dose of Valsacor® may be gradually increased up to maximum daily dose of 320 mg.
Cronic heart failure (II-IVFcclassification NYHA)
The recommended starting dose of Valsacor® is 40 mg2 times daily. The dose should be gradually increased over at least 2 weeks to 80 mg twice daily, and if well tolerated, to 160 mg twice daily. The maximum daily dose is 320 mg in two doses. In this case, it may be necessary to reduce the dose of concomitantly taken diuretics. It is possible to use simultaneously with other drugs intended for treatment of CHF. However, the combination of ACE inhibitor, beta-adrenoblocker and valsartan is not recommended. Renal function should always be evaluated in patients with CHF.
Elevation of survival in patients with acute myocardial infarction
In patients with stable hemodynamics, treatment should be started as early as 12 hours after myocardial infarction. The initial dose is 20 mg (1/2 tablet of Valsacor® 40 mg) 2 times daily, further the dose is increased by titration method up to 40 mg, 80 mg 2 times daily during several weeks until the target dose of 160 mg 2 times daily is reached. Dose increases depend on tolerability of valsartan during the titration period. The maximum daily dose is 320 mg in 2 doses.
As a rule, taking into account tolerability of therapy, it is recommended to increase the dose to 80 mg 2 times daily by the end of the 2nd week of therapy and to the maximum target dose of 160 mg 2 times daily – by the end of the 3rd month of therapy. In case of symptomatic arterial hypotension or renal dysfunction it is reasonable to consider reducing the dose.
Valsacor® can be used in patients after myocardial infarction against therapy with other drugs, including thrombolytics, acetylsalicylic acid as an antiaggregant, beta-adrenoblockers, HMG-CoA reductase inhibitors (statins) and diuretics. It is not recommended to use Valsacor® concomitantly with ACE inhibitors and other drugs inhibiting the RAAS.
In patients with myocardial infarction, renal function should always be evaluated.
special patient groups
special patient groups
Interaction
Interaction
Double RAAS blockade
In some patients, dual RAAS blockade was accompanied by the development of arterial hypotension, syncope, hyperkalemia, and impaired renal function, including ARF.
Caution is required when concomitant use of ARA II, including valsartan, with drugs that affect the RAAS, such as ACE inhibitors or aliskiren.
The concomitant use of ARA II, including valsartan, with drugs containing aliskiren is contraindicated in patients with diabetes and/or moderate to severe renal function impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
Simultaneous use of ARA II with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Lithium
Simultaneous use with lithium preparations is not recommended because of possible reversible increase of lithium concentration in blood plasma and development of intoxication. Concomitant use of valsartan with diuretics and lithium may further increase lithium concentrations and increase the risk of intoxication. If concomitant use with lithium preparations is necessary, plasma lithium concentrations should be monitored carefully.
Kalice-saving diuretics (spironolactone, eplerenone, triamterene, amiloride), potassium preparations, potassium-containing supplements and other drugs and substances that can increase serum potassium (e.g., heparin)
When concomitant use with drugs that affect potassium content is necessary, it is recommended to monitor the plasma potassium content.
Non-steroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors, acetylsalicylic acid at a dose greater than 3 g/day andunselective NSAIDs
With concomitant use, the antihypertensive effect may be weakened, the risk of renal dysfunction and increased plasma potassium may increase. At the beginning of therapy it is recommended to assess renal function, as well as to correct the water-electrolyte balance disorders.
Transfer protein inhibitors
invitro studies on liver cultures have shown that valsartan is a substrate for the OATP1B1/OATP1B3 and MRP2 transporter proteins. The clinical significance of this finding is unknown. Concomitant use of OATP1B1/OATP1B3 transporter protein inhibitors (eg, rifampicin, cyclosporine) and MRP2 (eg, ritonavir) may increase the systemic exposure of valsartan (Cmax and AUC). This should be considered both at the beginning of combined therapy with these drugs and at the end of it.
No clinically significant interactions have been identified with the following drugs: cimetidine, warfarin, furosemide, digoxin, atenolol, indomethacin, GHTZ,amlodipine and glibenclamide.
Directions for use
Directions for use
Take orally in a dose of 80 mg once daily or 40 mg twice daily, daily.
In the absence of adequate effect, the daily dose may be gradually increased.
The maximum daily dose is 320 mg in 2 doses.
Special Instructions
Special Instructions
Severe renal dysfunction in patients over 18 years of age (CKR less than 10 ml/min) (no clinical data), renal dysfunction in patients 6 to 18 years of age (CKR less than 30 ml/min), including those on hemodialysis, aortic and/or mitral valve stenosis, hypertrophic obstructive cardiomyopathy (HCMP), CHF (NYHA II-IV), post kidney transplantation, hemodialysis, hyponatremia, diet with restriction of table salt intake, bilateral renal artery stenosis or artery stenosis of a single kidney, hyperkalemia, primary hyperaldosteronism, conditions accompanied with a decrease in the volume of circulating blood (including diarrhea, vomiting, treatment with high doses of diuretics), in patients with hereditary angioedema, or edema against a background of previous therapy with ARA II or ACE inhibitors, concomitant use of ARA II with other drugs that inhibit the renin-angiotensin-aldosterone system (RAAS), such as ACE inhibitors and drugs containing aliskiren.
The use of ARAs II, including valsartan, simultaneously with ACE inhibitors is not recommended because their simultaneous use has no advantage over valsartan or ACE inhibitor monotherapy with respect to overall mortality rates.
It is contraindicated in children under the age of 6 years for arterial hypertension and under 18 years for other indications.
Patients 6 to 18 years
.Arterial hypertension
The recommended starting dose of Valsacor® in children and adolescents 6 to 18 years of age is 40 mg if the child weighs less than 35 kg and 80 mg if the child weighs more than 35 kg. It is recommended to adjust the dose taking into account the decrease of BP. Maximum recommended daily doses are shown in the table below. Use of higher doses is not recommended.
Body weight
Maximum recommended daily dose
⥠8 kg < 35 kg
80 mg
⥠35kg < 80kg
160 mg
⥠80 kg ⤠160 kg
320 mg
CHF and acute myocardial infarction
Valsacor® is not recommended for the treatment of CHF and acute myocardial infarction in patients younger than 18 years.
Special patient groups
Kidney function disorder
The safety of valsartan in children 6 to 18 years of age on hemodialysis or with a CK of less than 30 mL/min has not been studied. Therefore, the use of Valsacor® in such patients is not recommended. No dose adjustment of Valsacor® is required in children 6 to 18 years of age with a CK of more than 30 ml/min. Renal function and serum potassium should be monitored carefully.
Liver function impairment
The drug Valsacor® is contraindicated in children from 6 to 18 years old with liver dysfunction, biliary cirrhosis and cholestasis, as. because the maximum daily dose of valsartan in these patients should not exceed 80 mg.
Elderly patients (>65 years)
No dose adjustment is necessary for elderly patients.
Renal dysfunction
Dose adjustment of valsartan is not required in patients with renal dysfunction with a CKR greater than 10 ml/min. There are currently no data on the use of valsartan in patients with a FFR less than 10 mL/min.
Liver function impairment
Patients with hepatic dysfunction, biliary cirrhosis and cholestasis are contraindicated with Valsacor® in a dosage of 320 mg because. because the maximum daily dose should not exceed 80 mg.
The administration of Valsacor® in hypertensive patients does not require a regular control of laboratory values.
Double RAAS blockade
In some patients double RAAS blockade was accompanied by development of severe arterial hypotension, syncope, stroke, hyperkalemia and renal dysfunction (including ARF).
The concomitant use of ARA II, including valsartan, with drugs that affect the RAAs, such as ACE inhibitors or aliskiren, is not recommended and BP, renal function, and plasma electrolytes should be carefully controlled if this therapy is necessary.
The concomitant use of ARA II, including valsartan, with drugs containing aliskiren is contraindicated in patients with diabetes and/or moderate to severe renal function impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
Simultaneous use of ARA II with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Hyponatremia and/or dehydration
In patients with severe hyponatremia and/or dehydration, such as due to high doses of diuretics, in rare cases arterial hypotension with clinical manifestations may develop at the beginning of therapy with Valsacor®. Before the start of treatment it is recommended to restore the sodium content and/or replenish the blood circulation, particularly by reducing the doses of diuretics.
In case of arterial hypotension with clinical manifestations the patient should be placed horizontally and, if necessary, 0.9% sodium chloride solution should be infused intravenously. The therapy with Valsacor® can be continued only after hemodynamic stabilization.
Hyperkalemia
The concomitant use of potassium-saving diuretics (spironolactone, eplerenone, triamterene, amiloride), potassium drugs, potassium-containing supplements, or other drugs that can increase serum potassium levels (such as heparin) is not recommended. It is necessary to monitor the content of potassium in blood plasma.
Renal artery stenosis
Long-term use of valsartan in patients with renovascular hypertension secondary to unilateral renal artery stenosis was not accompanied by significant changes in renal hemodynamic parameters, serum creatinine or urea nitrogen concentrations. Since other drugs acting on the RAAS may increase serum concentrations of urea and creatinine in patients with bilateral renal artery stenosis or arterial stenosis of the uniciliary artery, continuous monitoring of these parameters is recommended as a precaution.
Condition after undergoing kidney transplantation
The safety of Valsacor® in patients who have recently undergone a kidney transplant has not been established.
Primary hyperaldosteronism
Patients with primary hyperaldosteronism are resistant to hypotensive drugs that affect the RAAS, so use of Valsacor® is not recommended in such patients.
Aortic and/or mitral valve stenosis, GOCMP
Valsacor® should be used with caution in patients with hemodynamically significant aortic and/or mitral valve stenosis or with GOCMP.
Renal dysfunction
In patients with renal dysfunction, no change in drug dosages is required because there is no data about using Valsacor in patients with severe renal insufficiency (CKD less than 10 ml/min or 0.167 ml/s) and in patients on hemodialysis; in such cases the drug is recommended to be used with caution.
The concomitant use of ARA II, including valsartan, or ACE inhibitors with aliskiren is contraindicated in patients with impaired renal function (FFR less than 60 ml/min/1.73 m2 body surface area).
Liver function impairment
Patients with hepatic dysfunction, biliary cirrhosis and cholestasis, Valsacor® in a dosage of 320 mg is contraindicated because. because the maximum daily dose should not exceed 80 mg.
Angeoneurotic edema in history
Among patients with angioedema (laryngeal and vocal cord edema causing airway obstruction and/or edema of the face, lips, pharynx, and/or tongue), there have been cases of a history of developing angioedema during therapy with Valsacor®, including when taking ACE inhibitors. In case of angioedema development the drug should be immediately discontinued and the possibility of its repeated use should be excluded.
Arterial hypertension
In AH, Valsacor® can be used in monotherapy or simultaneously with other hypotensive agents, particularly diuretics.
CHF/increased survival of patients with acute myocardial infarction
The use of Valsacor® in combination with other drugs used in acute myocardial infarction (thrombolytics, acetylsalicylic acid as an antiplatelet agent, beta-adrenoblockers and HMG-CoA reductase inhibitors (statins)) is possible. Simultaneous use of Valsacor® and ACE inhibitors in this category of patients is not recommended because this combined therapy does not lead to additional clinical effect and is accompanied by an increased risk of NSD compared to the therapy with two drugs separately.
The triple combination therapy (with Valsacor®, ACE inhibitor and beta-adrenoblocker) is not recommended in patients with CHF because it does not increase additional clinical effect and is associated with an increased risk of NS.
The use of Valsacor® in patients with CHF or acute myocardial infarction often results in a slight decrease of BP. Generally, there is no need to discontinue the drug if the dosing instructions are followed.
In patients whose renal function may depend on RAAS activity (e.g., patients with NYHA class II-IV CHF), therapy with ACE inhibitors and ARA II is associated with oliguria and/or azotemia and rarely with ARF and/or mortality. Since valsartan is an ARA II, the possibility of worsening of renal function when using it cannot be excluded.
The initiation of therapy in patients with CHF or acute myocardial infarction should be cautious. When examining patients, renal function should always be evaluated.
Special information on excipients
The drug Valsacor® contains lactose, so the drug is contraindicated in patients with lactase deficiency, lactose intolerance, and glucose-galactose malabsorption syndrome.
We should use caution when driving a vehicle and engaging in potentially dangerous activities requiring high concentration and quick psychomotor reactions because dizziness or weakness with arterial hypotension may develop.
Synopsis
Synopsis
Oval, biconvex tablets with a rib on one side, covered with a film coating of light brown color.
Features
Features
Valsartan is rapidly absorbed from the gastrointestinal tract after oral administration; the degree of absorption varies individually. Absolute bioavailability averages 23%. Pharmacokinetic curve of valsartan has multiexponential character (T1/2 in α-phase < 1 h and T1/2 in β-phase – about 9 h), kinetics are linear.
There were no changes in pharmacokinetic parameters when administered as a course.
The AUC is decreased by 48% when valsartan is taken with food, with plasma concentrations of valsartan being similar in patients taken with food and on an empty stomach approximately 8 hours after ingestion. The decrease in AUC is not accompanied by a clinically significant decrease in therapeutic effect.
If valsartan is taken once daily, there is little cumulation. Plasma concentrations of valsartan in women and men were similar.
Binding to plasma proteins, predominantly to albumin, is 94-97%. Vd in equilibrium is about 17 liters.
The plasma clearance of valsartan is about 2 L/h. It is excreted with the feces – 70% and with urine – 30%, mostly unchanged.
In biliary cirrhosis or biliary obstruction, the AUC of valsartan increases approximately 2-fold.
Contraindications
Contraindications
Side effects
Side effects
The incidence of NS is comparable to placebo. There are no data on dose- or duration-of-treatment relationships or on patients’ age, gender, or race. The safety profile of valsartan in patients with AH aged 6 to 18 years does not differ from the safety profile of valsartan in patients with AH over 18 years.
World Health Organization (WHO) recommended side effect frequency classification:
very frequently â¥1/10
often â¥1/100 to < 1/10
infrequently â¥1/1000 to < 1/100
rarely from â¥1/10000 to < 1/1000
very rarely from < 1/10000
frequency is unknown cannot be estimated from available data.
All valsartan NNIs identified in clinical practice and in the analysis of laboratory parameters cannot be attributed to any frequency of occurrence, so they are categorized as “frequency unknown.”
Arterial hypertension
Blood and lymphatic system disorders:
incidence unknown: decreased hemoglobin, hematocrit, neutropenia, thrombocytopenia.
Immune system disorders:
incidence unknown: hypersensitivity reactions, including serum sickness.
Metabolic and nutritional disorders:
incidence unknown: increased serum potassium, hyponatremia.
Hearing organ and labyrinth disorders:
infrequent: vertigo.
vascular disorders:
frequency unknown: vasculitis.
Respiratory system, thoracic and mediastinal organs:
infrequent: cough.
Gastrointestinal tract disorders:
infrequent: abdominal pain.
Liver and biliary tract disorders:
incidence unknown: liver function disorders, including increased plasma bilirubin concentration.
Skin and subcutaneous tissue disorders:
very rare: Angioneurotic edema, skin rash, skin itching;
frequency unknown: bullous dermatitis.
Musculoskeletal and connective tissue disorders:
frequency unknown: myalgia.
Renal and urinary tract disorders:
incidence unknown: impaired renal function, increased serum creatinine concentration.
General disorders and disorders at the site of administration:
infrequent: increased fatigue.
Also during clinical studies, the following ONs have been observed in patients with AH (causal relationship with taking the drug has not been established): arthralgia, asthenia, back pain, diarrhea, dizziness, insomnia, decreased libido, nausea, peripheral edema, pharyngitis, rhinitis, sinusitis, upper respiratory infections, viral infections.
In adult patients with acute myocardial infarction and/or CHF, the safety profile in clinical trials is somewhat different from that of patients with AH. This may be related to the disease itself.
CHF(II-IVFKby classification NYHA)and nincreased survival of patients with acute myocardial infarction
Blood and lymphatic system disorders:
frequency unknown: thrombocytopenia.
Immune system disorders:
frequency unknown: hypersensitivity reactions, including serum sickness.
Metabolic and nutritional disorders:
infrequent: hyperkalemia;
frequency unknown: increased serum potassium, hyponatremia.
Nervous system disorders:
often: dizziness, orthostatic (postural) dizziness;
infrequently: syncope, headache.
Hearing organ and labyrinth disorders:
infrequently: vertigo.
Cardiac disorders:
infrequent: aggravation of CHF symptoms.
vascular disorders:
often: marked BP decrease, orthostatic hypotension;
frequent unknown: vasculitis.
Respiratory, thoracic and mediastinal disorders:
infrequent: cough.
Gastrointestinal tract disorders:
infrequently: nausea, diarrhea.
Liver and biliary tract disorders:
frequency unknown: impaired liver function, increased activity of “liver” transaminases in blood plasma.
Skin and subcutaneous tissue disorders:
very rare: Angioneurotic edema;
frequency unknown: skin rash, pruritus, bullous dermatitis, urticaria.
Musculoskeletal and connective tissue disorders:
rarely: rhabdomyolysis;
frequency unknown: myalgia.
Kidney and urinary tract disorders:
often: impaired renal function;
infrequently: Acute renal failure (ARF), increased serum creatinine concentration;
frequent unknown: increased serum urea residual nitrogen concentration.
General disorders and disorders at the site of administration:
infrequent: asthenia, increased fatigue.
Also in clinical studies in patients after acute myocardial infarction and/or in CHF, the following NIs have been observed (causal relationship to valsartanan administration has been established): Arthralgia, abdominal pain, back pain, asthenia, insomnia, decreased libido, neutropenia, peripheral edema, pharyngitis, rhinitis, sinusitis, upper respiratory tract infections, and viral infections.
Overdose
Overdose
Symptoms:a marked decrease in BP, which may lead to impaired consciousness, collapse and/or shock.
Treatment: symptomatic, the nature of which depends on the time elapsed since taking the drug and the severity of symptoms. In case of accidental overdose, vomiting should be induced (if the drug was taken recently) or gastric lavage should be performed.
When the blood pressure is significantly decreased, the patient should be transferred into the supine position with the legs raised, and then the measures should be taken to maintain the cardiovascular and respiratory systems functions, to refill the circulatory pressure with 0.9 % sodium chloride solution (IV) and to control the daily diuresis.
hemodialysis is ineffective.
Pregnancy use
Pregnancy use
Pregnancy
Pregnancy
Similarities
Similarities
Additional information
| Shelf life | 5 years. Do not use the drug after the expiration date. |
|---|---|
| Conditions of storage | At the temperature not more than 25 ºС, in the original package. Keep out of reach of children. |
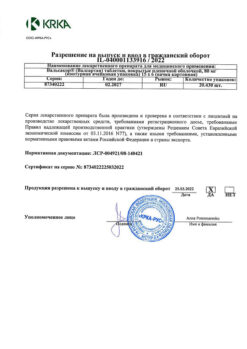
| Manufacturer | KRKA-RUS, Russia |
| Medication form | pills |
| Brand | KRKA-RUS |
Other forms…
Related products
Buy Valsacor, 320 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.