No products in the cart.
Utrogestan, 200 mg capsules 14 pcs
€15.84 €14.48
Description
Pharmacotherapeutic group: gestagen
ATX code: G03DA04
Pharmacological Properties
Pharmacodynamics
The active ingredient of Utrogestan® is progesterone, which is identical to the natural hormone of the corpus luteum of the ovary. It binds to receptors on the surface of target cells and penetrates the nucleus where, by activating DNA, it stimulates RNA synthesis. It promotes transition of uterine mucosa from the phase of proliferation caused by the follicular hormone estradiol to the secretory phase, and after fertilization to a state required for development of a fertilized egg.
It reduces the excitability and contractility of uterine muscles and fallopian tubes. Promotes the formation of normal endometrium. Stimulates the development of mammary gland terminal elements and induces lactation.
By stimulating protein lipase, increases fat reserves; increases glucose utilization; by increasing the concentration of basal and stimulated insulin, promotes glycogen accumulation in the liver; increases production of gonadotropic hormones of the pituitary; reduces azotemia, increases nitrogen excretion by the kidneys.
Pharmacokinetics
When taken orally.
Indications
Indications
Progesterone deficiency conditions in women:
For oral administration:
– threatened abortion or prevention of habitual abortion due to progesterone deficiency;
– infertility due to luteal insufficiency;
– premenstrual syndrome;
– menstrual cycle disorders due to ovulation or anovulation disorders;
– fibrocystic mastopathy;
– period of menopausal transition;
– menopausal (replacement) hormone therapy (MHT) in peri- and postmenopause (in combination with estrogen-containing drugs).
For intravaginal use:
– MHT in case of progesterone deficiency with non-functioning (absent) ovaries (egg donation);
– prevention (prophylaxis) of premature birth in women at risk (with shortening of the cervix and/or anamnestic data of premature birth and/or premature rupture of membranes);
– support of the luteal phase during preparation for in vitro fertilization;
– support of the luteal phase in a spontaneous or induced menstrual cycle;
premature menopause;
– MHT (in combination with estrogen-containing drugs);
– infertility due to luteal insufficiency;
– threatened abortion or prevention of habitual abortion due to progesterone deficiency.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: gestagen
ATX code: G03DA04
PHARMACOLOGICAL PROPERTIES
Pharmacodynamics
The active ingredient of Utrozhestan® is progesterone, which is identical to the natural hormone of the corpus luteum of the ovary. By binding to receptors on the surface of cells of target organs, it penetrates into the nucleus, where, activating DNA, it stimulates RNA synthesis. Promotes the transition of the uterine mucosa from the proliferation phase caused by the follicular hormone estradiol to the secretory phase, and after fertilization to the state necessary for the development of the fertilized egg.
Reduces the excitability and contractility of the muscles of the uterus and fallopian tubes. Promotes the formation of normal endometrium. Stimulates the development of the end elements of the mammary gland and induces lactation.
By stimulating protein lipase, it increases fat reserves; increases glucose utilization; increasing the concentration of basal and stimulated insulin, promotes the accumulation of glycogen in the liver; increases the production of gonadotropic hormones of the pituitary gland; reduces azotemia, increases nitrogen excretion by the kidneys.
Pharmacokinetics
When taken orally
Special instructions
Special instructions
Utrozhestan® should not be used for contraception.
The drug should not be taken with food, since food intake increases the bioavailability of progesterone.
The drug Utrozhestan® should be taken with caution in patients with diseases and conditions that may be aggravated by fluid retention (arterial hypertension, cardiovascular disease, chronic renal failure, epilepsy, migraine, bronchial asthma); in patients with diabetes mellitus; liver dysfunction of mild to moderate severity; photosensitivity.
Patients with a history of depression should be monitored, and if severe depression develops, the drug should be discontinued.
Utrozhestan® contains soy lecithin, which can cause hypersensitivity reactions (urticaria and anaphylactic shock).
Patients with concomitant cardiovascular diseases or a history of them should also be periodically observed by a doctor.
The use of Utrozhestan® after the first trimester of pregnancy may cause the development of cholestasis.
During long-term treatment with progesterone, regular medical examinations (including liver function tests) are necessary; Treatment should be discontinued if abnormal liver function tests or cholestatic jaundice occur.
When using progesterone, it is possible to reduce glucose tolerance and increase the need for insulin and other hypoglycemic drugs in patients with diabetes mellitus.
If amenorrhea occurs during treatment, pregnancy must be excluded.
If the course of treatment begins too early in the menstrual cycle, especially before the 15th day of the cycle, shortening of the cycle and/or acyclic bleeding is possible. In case of acyclic bleeding, the drug should not be used until the cause is determined, including a histological examination of the endometrium.
If there is a history of chloasma or a tendency to develop it, patients are advised to avoid UV irradiation.
More than 50% of spontaneous abortions in early pregnancy are caused by genetic disorders. In addition, the cause of spontaneous abortions in early pregnancy can be infectious processes and mechanical damage. The use of the drug Utrozhestan® in these cases can only lead to a delay in rejection and evacuation of a non-viable fertilized egg.
The use of the drug Utrozhestan® to prevent threatened abortion is justified only in cases of progesterone deficiency.
When conducting MHT with estrogens during perimenopause, it is recommended to use the drug Utrozhestan® for at least 12 days of the menstrual cycle.
With a continuous MHT regimen in postmenopause, it is recommended to use the drug from the first day of taking estrogen.
When conducting MHT, the risk of developing venous thromboembolism (deep vein thrombosis or pulmonary embolism), the risk of developing ischemic stroke, and coronary heart disease increases.
Due to the risk of developing thromboembolic complications, the use of the drug should be discontinued if: visual disturbances such as loss of vision, exophthalmos, double vision, vascular lesions of the retina occur; migraines; venous thromboembolism or thrombotic complications, regardless of their location.
If there is a history of thrombophlebitis, the patient should be closely monitored.
When using Utrozhestan® with estrogen-containing drugs, you must refer to the instructions for their use regarding the risks of venous thromboembolism.
The results of the Women Health Initiative Study (WHI) clinical study indicate a slight increase in the risk of breast cancer with long-term, more than 5 years, combined use of estrogen-containing drugs with synthetic gestagens. It is unknown whether there is an increased risk of breast cancer in postmenopausal women when undergoing MHT with estrogen-containing drugs in combination with progesterone.
The WHI study also found an increased risk of dementia when starting MHT after age 65 years.
Before starting MHT and regularly during it, a woman should be examined to identify contraindications to its implementation. If clinically indicated, a breast examination and gynecological examination should be performed.
The use of progesterone may affect the results of some laboratory tests, including liver and thyroid function tests; coagulation parameters; pregnanediol concentration.
Impact on the ability to drive vehicles and machinery
When using the drug orally, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Progesterone
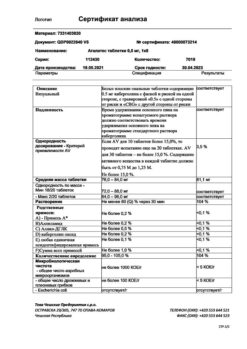
Composition
Composition
for 1 capsule:
Active ingredient:
micronized progesterone 100 or 200 mg.
Excipients:
sunflower oil 149 mg/298 mg,
soy lecithin 1 mg/2 mg;
capsule – gelatin 76.88 mg/153.76 mg,
glycerin 31.45 mg/62.9 mg,
titanium dioxide 1.67 mg/3.34 mg.
Contraindications
Contraindications
Hypersensitivity to progesterone or any of the excipients of the drug; deep vein thrombosis, thrombophlebitis; thromboembolic disorders (pulmonary embolism, myocardial infarction, stroke), intracranial hemorrhage or a history of these conditions/diseases; bleeding from the vagina of unknown origin; incomplete abortion; porphyria; established or suspected malignant neoplasms of the breast and genital organs; severe liver diseases (including cholestatic jaundice, hepatitis, Dubin-Johnson syndrome, Rotor syndrome, malignant liver tumors) currently or in history; children under 18 years of age (efficacy and safety have not been established); breastfeeding period.
With caution:
Diseases of the cardiovascular system, arterial hypertension, chronic renal failure, diabetes mellitus, bronchial asthma, epilepsy, migraine, depression, hyperlipoproteinemia, mild to moderate liver dysfunction; photosensitivity.
The drug should be used with caution in the second and third trimesters of pregnancy.
Side Effects
Side Effects
The following adverse events noted during oral administration of the drug are distributed according to the frequency of occurrence in accordance with the following gradation: often >1/100, 1/1000, 1/10000, <1/1000; very rarely <1/10000.
From the genital organs and mammary gland: often – menstrual irregularities, amenorrhea, acyclic bleeding; infrequently – mastodynia.
From the mental side: very rarely – depression.
From the nervous system: often – headache; infrequently – drowsiness, transient dizziness.
From the gastrointestinal tract: often – bloating; uncommon – vomiting, diarrhea, constipation; rarely – nausea.
From the liver and biliary tract: infrequently – cholestatic jaundice.
From the immune system: very rarely – urticaria.
From the skin and subcutaneous tissues: infrequently – itching, acne; very rarely – chloasma.
Drowsiness and transient dizziness are possible, as a rule, 1–3 hours after taking the drug. These side effects can be reduced by reducing the dose, using the drug at bedtime, or switching to the vaginal route of administration.
These unwanted effects are usually the first signs of an overdose. Drowsiness and/or transient dizziness are observed, in particular, in the case of concomitant hypoestrogenism. Reducing the dose or restoring higher estrogenization immediately eliminates these effects without reducing the therapeutic effect of progesterone.
If the course of treatment begins too early (in the first half of the menstrual cycle, especially before the 15th day), a shortening of the menstrual cycle or acyclic bleeding is possible.
Recorded changes in the menstrual cycle, amenorrhea or acyclic bleeding are characteristic of all progestogens.
Application in clinical practice
During post-marketing use, the following adverse events were noted with oral use of progesterone: insomnia; premenstrual syndrome; tension in the mammary glands; vaginal discharge; joint pain; hyperthermia; increased sweating at night; fluid retention; change in body weight; acute pancreatitis; alopecia, hirsutism; changes in libido; thrombosis and thromboembolic complications (when carrying out HRT in combination with estrogen-containing drugs); increase in blood pressure.
The drug contains soy lecithin, which can cause hypersensitivity reactions (urticaria and anaphylactic shock).
Vaginal method of application. Isolated cases of the development of reactions of local intolerance to the components of the drug (in particular soy lecithin) in the form of hyperemia of the vaginal mucosa, burning, itching, and oily discharge have been reported.
Systemic side effects with intravaginal use of the drug in recommended doses, in particular drowsiness or dizziness (observed with oral administration of the drug), were not observed.
Interaction
Interaction
For oral administration
Progesterone enhances the effect of diuretics, antihypertensive drugs, immunosuppressants, and anticoagulants. Reduces the lactogenic effect of oxytocin.
Concomitant use with drugs that induce microsomal liver enzymes CYP3A4, such as barbiturates, antiepileptic drugs (phenytoin, carbamazepine), rifampicin, phenylbutazone, spironolactone, griseofulvin, is accompanied by acceleration of progesterone metabolism in the liver.
Simultaneous use of progesterone with some antibiotics (penicillins, tetracyclines) can lead to a decrease in its effectiveness due to disruption of the enterohepatic recirculation of sex hormones due to changes in the intestinal microflora.
The severity of these interactions may vary in different patients, so predicting the clinical effects of these interactions is difficult.
Ketoconazole may increase the bioavailability of progesterone. Progesterone may increase the concentration of ketoconazole and cyclosporine.
Progesterone may reduce the effectiveness of bromocriptine.
Progesterone can cause a decrease in glucose tolerance, resulting in an increase in the need for insulin or other hypoglycemic drugs in patients with diabetes.
The bioavailability of progesterone may be reduced in patients who smoke and with excessive alcohol consumption.
For intravaginal use
The interaction of progesterone with other drugs when administered intravaginally has not been assessed. The simultaneous use of other drugs used intravaginally should be avoided to avoid interfering with the release and absorption of progesterone.
Overdose
Overdose
Symptoms: drowsiness, transient dizziness, euphoria, shortening of the menstrual cycle, dysmenorrhea.
In some patients, the average therapeutic dose may be excessive due to existing or emerging unstable endogenous secretion of progesterone, special sensitivity to the drug, or too low concentration of estradiol.
Treatment: in case of drowsiness or dizziness, it is necessary to reduce the daily dose or prescribe the drug before bedtime for 10 days of the menstrual cycle; in case of a shortening of the menstrual cycle or spotting, it is recommended to postpone the start of treatment to a later day of the cycle (for example, on the 19th instead of the 17th); in perimenopause and with postmenopausal MHT, it is necessary to ensure that the concentration of estradiol is optimal.
In case of overdose, symptomatic treatment is carried out if necessary.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years. Do not use after expiration date.
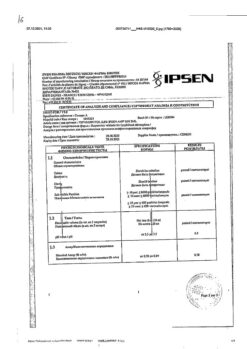
Manufacturer
Manufacturer
Bezen Manufacturing Rus LLC, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25 ° C. Store out of the reach of children. |
| Manufacturer | Bezen Manufacturing Rus LLC, Russia |
| Medication form | capsules |
| Brand | Bezen Manufacturing Rus LLC |
Other forms…
Related products
Buy Utrogestan, 200 mg capsules 14 pcs with delivery to USA, UK, Europe and over 120 other countries.