No products in the cart.
Uronormin-F, 3 g 8 g 2 pcs
€30.41 €25.34
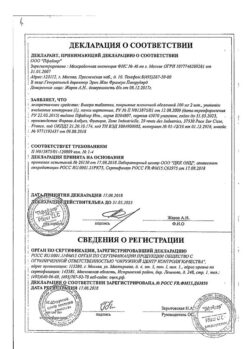
Description
URONORMIN-F contains phosphomycin [mono (2-ammonium-2-hydroxymethyl-1,3-propanediol)(2R-cis)-(3-methyloxyranil) phosphonate] – a broad spectrum antibacterial agent, a phosphonic acid derivative designed to treat urinary tract infections.
The mechanism of action is associated with inhibition of the first stage of synthesis of the bacterial cell wall. Being a structural analogue of phosphoenolpyruvate it competitively inhibits irreversibly the enzyme UDF-N-acetylglucosamienolpyruviltransferase which catalyzes the reaction of formation of UDF-N-acetyl-3-O-(1-carboxyvinyl)-D-glucosamine from phosphoenolpyruvate and UDF-N-acetyl-D-glucosamine. The drug is also able to reduce bacterial adhesion to the bladder mucosa, which may play the role of a predisposing factor for recurrent infections.
The mechanism of action of the drug explains the absence of cross-resistance with other classes of antibiotics and the mutual reinforcement of action with antibiotics of other classes, such as beta-lactam antibiotics.
Phosphomycin is active against a wide range of Gram-positive and Gram-negative microorganisms commonly isolated in urinary tract infections, such as Escherichia coli, Citrobacterspp., Klebsiellaspp., Proteusspp., Serratiaspp., Pseudomonasaeruginosa, Enterrococcusfaecalis.
The emergence of resistance in the laboratory is explained by mutations in the glpT and uhp genes, which control L-alpha-glycerophosphate and glucose phosphate transport, respectively.
Pharmacokinetics:
Intake:
In oral administration phosphomycin is well absorbed from the intestine and achieves bioavailability of about 50%. Maximal concentration in plasma is observed 2-2.5 hours after oral administration and is 22-32 mg/l. The plasma elimination half-life is 4 hours. Intake with food slows absorption without affecting the concentration in the urine.
Distribution:
Phosphomycin is distributed in the kidneys, bladder wall, prostate and seminal glands. A steady urinary concentration of fosfomycin exceeding the Minimum Bacteriostatic Concentration (MBc) is reached 24-48 hours after oral administration. Fosfomycin does not bind to plasma proteins and crosses the placental barrier. After a single administration, fosfomycin is excreted into breast milk in small amounts.
Fosfomycin is excreted unchanged, mainly by the kidneys, through glomerular filtration (40-50 % of the dose taken is found in the urine), with a half-life of about 4 hours, and, to a lesser extent, with the feces (18-28 % of the dose). The occurrence of a second peak serum concentration 6 and 10 hours after drug administration suggests that the drug is subject to intestinal hepatic recirculation.
Pharmacokinetic properties of fosfomycin are independent of age and pregnancy. The drug cumulates in patients with renal insufficiency; a linear relationship between pharmacokinetic parameters of fosfomycin and glomerular filtration rate has been established.
Indications
Indications
Treatment of infectious and inflammatory diseases (caused by microorganisms sensitive to the drug) of the lower urinary tract, incl. acute bacterial cystitis, exacerbation of chronic recurrent bacterial cystitis, acute bacterial urovesical syndrome, bacterial nonspecific urethritis, asymptomatic massive bacteriuria (during pregnancy), postoperative urinary tract infection.
Prevention of urinary tract infections during surgical interventions and transurethral diagnostic examinations.
Pharmacological effect
Pharmacological effect
URONORMIN-F contains fosfomycin [mono (2-ammonium-2-hydroxymethyl-1,3-propanediol)(2R-cis)-(3-methyloxiranyl) phosphonate] – a broad-spectrum antibacterial agent, a phosphonic acid derivative, intended for the treatment of urinary tract infections.
The mechanism of action is associated with the suppression of the first stage of bacterial cell wall synthesis. Being a structural analogue of phosphoenolpyruvate, it competitively and irreversibly inhibits the enzyme UDP-N-acetylglucosamienolpyruvyltransferase, which catalyzes the formation of UDP-N-acetyl-3-O-(1-carboxyvinyl)-D-glucosamine from phosphoenolpyruvate and UDP-N-acetyl-D-glucosamine. The drug is also able to reduce the adhesion of bacteria to the mucous membranes of the bladder, which can play the role of a predisposing factor for recurrent infections.
The mechanism of action of the drug explains the lack of cross-resistance with other classes of antibiotics and the mutual enhancement of action with antibiotics of other classes, for example with beta-lactam antibiotics.
Fosfomycin is active against a wide range of gram-positive and gram-negative microorganisms usually isolated during urinary tract infections, such as Escherichiacoli, Citrobacter spp., Klebsiellas pp., Proteus spp., Serratias pp., Pseudomonasaeruginosa, Enterrococcus faecalis.
The emergence of resistance in laboratory conditions is explained by mutations in the glpT and uhp genes, which control the transport of L-alpha-glycerophosphates and glucose phosphates, respectively.
Pharmacokinetics:
Suction:
When taken orally, fosfomycin is well absorbed from the intestine and reaches a bioavailability of about 50%. The maximum concentration in plasma is observed after
2-2.5 hours after oral administration and is 22-32 mg/l. The plasma half-life is 4 hours. Taking with food slows down absorption without affecting urinary concentrations.
Distribution:
Fosfomycin is distributed in the kidneys, bladder walls, prostate and seminal glands. A constant concentration of fosfomycin in urine exceeding the Minimum Bacteriostatic Concentration (MBC) is achieved 24-48 hours after oral administration. Fosfomycin is not bound to plasma proteins and crosses the placental barrier. After a single dose, fosfomycin is excreted into breast milk in small quantities.
Removal:
Fosfomycin is excreted unchanged, mainly by the kidneys, by glomerular filtration (40-50% of the dose taken is found in the urine), with an elimination half-life of about 4 hours, and to a lesser extent in feces (18-28% of the dose). The occurrence of a second peak serum concentration 6 and 10 hours after dosing suggests that the drug is subject to enterohepatic recirculation.
Pharmacokinetic properties
fosfomycin does not depend on age and pregnancy. The drug accumulates in
patients with renal failure; between pharmacokinetic parameters
fosfomycin and glomerular filtration rate were found to be linear
addiction.
Special instructions
Special instructions
Hypersensitivity reactions, including anaphylaxis and anaphylactic shock, which can be life-threatening, may occur during treatment with fosfomycin. In such cases, it is necessary to exclude repeated use of fosfomycin and carry out adequate treatment.
The use of almost all antibacterial agents, including fosfomycin, can lead to antibiotic-associated diarrhea. Its severity can range from mild diarrhea to fatal colitis.
Diarrhea, especially severe, persistent and/or bloody diarrhea, observed during or after treatment with fosfomycin (including several weeks after treatment), may be a symptom of pseudomembranous colitis caused by Clostridium difficile.
If a diagnosis of pseudomembranous colitis is suspected or confirmed, treatment should be started immediately. Drugs that suppress intestinal motility are contraindicated in this clinical situation.
Use for renal failure: the concentration of fosfomycin in the urine remains for 48 hours after taking the usual dose if the creatinine clearance is above 10 ml/min. The drug is contraindicated in patients undergoing hemodialysis.
Patients with diabetes mellitus should take into account that 1 package of the drug with a dosage of 2 g or 3 g of fosfomycin contains 2.100 g or 2.213 g of sucrose, respectively.
This drug is contraindicated in patients with rare hereditary diseases such as fructose intolerance, glucose-galactose malabsorption or sucrase-isomaltase deficiency.
Impact on the ability to drive vehicles and machinery
Patients should be warned about the possibility of developing dizziness, and if dizziness occurs, they should refrain from performing these activities.
Active ingredient
Active ingredient
Fosfomycin
Composition
Composition
Active ingredient:
Fosfomycin trometamol – 5.631 g
in terms of fosfomycin – 3.0 g
Excipients:
Sucrose – 2.213 g
Tangerine flavor – 0.070 g
Orange flavor – 0.070 g
Sodium saccharinate – 0.016 g
Weight of package contents – 8,000 g
Pregnancy
Pregnancy
During pregnancy, the drug is prescribed only when the potential benefit to the mother outweighs the potential risk to the fetus.
Data from the limited number of pregnancies studied do not show any adverse effects on the pregnancy, the fetus, or the health of the newborn.
If it is necessary to prescribe the drug during breastfeeding, breastfeeding should be stopped for the duration of treatment.
Contraindications
Contraindications
– Hypersensitivity to fosfomycin and other components of the drug;
– severe renal failure (creatinine clearance < 10 ml/min);
– children up to 5 years of age (for a dosage of 2 g), children up to 12 years of age (for a dosage of 3 g);
– hemodialysis;
– sucrase/isomaltase deficiency;
– fructose intolerance;
– glucose-galactose malabsorption.
Side Effects
Side Effects
The most common adverse reactions to a single dose of fosfomycin are gastrointestinal disorders, most often diarrhea. These reactions are short-lived and resolve spontaneously.
The following are adverse reactions that have been reported with fosfomycin during clinical trials or post-marketing surveillance.
The frequency of reactions is indicated as follows: very often (≥ 1/10); often (≥ 1/100 – < 1/10); uncommon (≥ 1/1,000 - < 1/100); rare (≥ 1/10,000 - < 1/1,000); very rare (<1/10,000); unknown - the incidence of adverse reactions cannot be estimated based on available data.
In each group, adverse reactions are presented in descending order of severity.
Infectious and parasitic diseases:
Uncommon: vulvovaginitis
Rare: superinfection
Immune system disorders:
Not known: anaphylactic reactions, including anaphylactic shock, hypersensitivity
Nervous system disorders:
Uncommon: headache, dizziness
Rare: paresthesia
Cardiac disorders:
Very rare: tachycardia
Disorders of the respiratory system, chest and mediastinal organs:
Unknown: asthma, bronchospasm, shortness of breath
Gastrointestinal disorders:
Uncommon: diarrhea, nausea, dyspepsia
Rarely: abdominal pain, vomiting
Unknown: antibiotic-associated colitis, decreased appetite
Skin and subcutaneous tissue disorders:
Rarely: rash, urticaria, itching
Unknown: angioedema
General disorders and disorders at the injection site:
Rare: fatigue
Vascular disorders:
Unknown: decreased blood pressure, petechiae
Liver and biliary tract disorders:
Unknown: transient increase in alkaline phosphatase and liver transaminases
Blood and lymphatic system disorders:
Rare: aplastic anemia
Unknown: eosinophilia, thrombocytosis (petechiae).
Interaction
Interaction
When used together with fosfomycin, metoclopramide reduces the concentration of fosfomycin in serum and urine.
The simultaneous use of antacids or calcium salts leads to a decrease in the concentration of fosfomycin in the blood plasma and urine. Drugs that increase motor activity (motility) of the gastrointestinal tract can cause a similar effect (decreasing the concentration of fosfomycin in blood plasma and urine).
There may be specific problems associated with changes in the international normalized ratio (INR). Numerous cases of increased antivitamin K antagonist activity have been reported in patients receiving antibiotics.
In the presence of risk factors such as severe infection, inflammation, age, or poor general health, changes in INR may be due to both the infectious disease and its treatment. Such changes are considered more typical for the following classes of antibiotics: fluoroquinolones, macrolides, cyclines, cotrimoxazole and some cephalosporins.
Overdose
Overdose
Data regarding oral overdose of fosfomycin are limited. In patients who took an excessive dose of the drug, the following reactions were observed: dysfunction of the vestibular apparatus, hearing impairment, a “metallic” taste in the mouth, as well as a general decrease in taste perception.
Treatment for overdose is symptomatic and supportive.
In case of overdose, it is recommended to take fluids orally to increase diuresis.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
2 years.
Manufacturer
Manufacturer
Pharmstandard-Leksredstva, Russia
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25 ° C. Keep out of reach of children. |
| Manufacturer | Pharmstandard-Leksredstva, Russia |
| Medication form | oral solution |
| Brand | Pharmstandard-Leksredstva |
Other forms…
Related products
Buy Uronormin-F, 3 g 8 g 2 pcs with delivery to USA, UK, Europe and over 120 other countries.