No products in the cart.
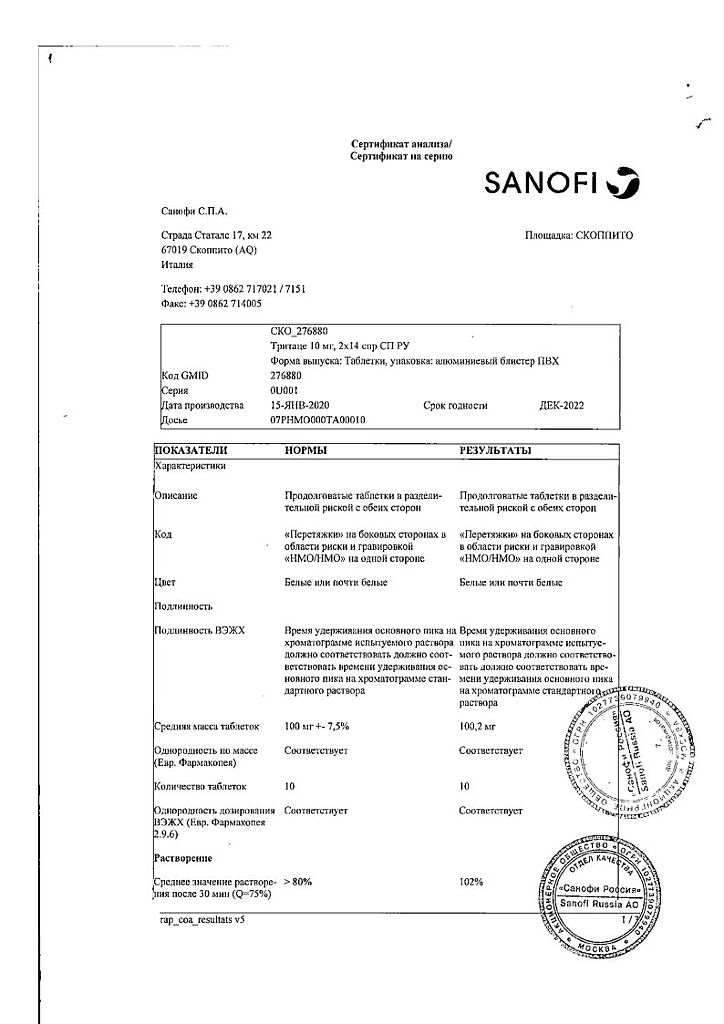
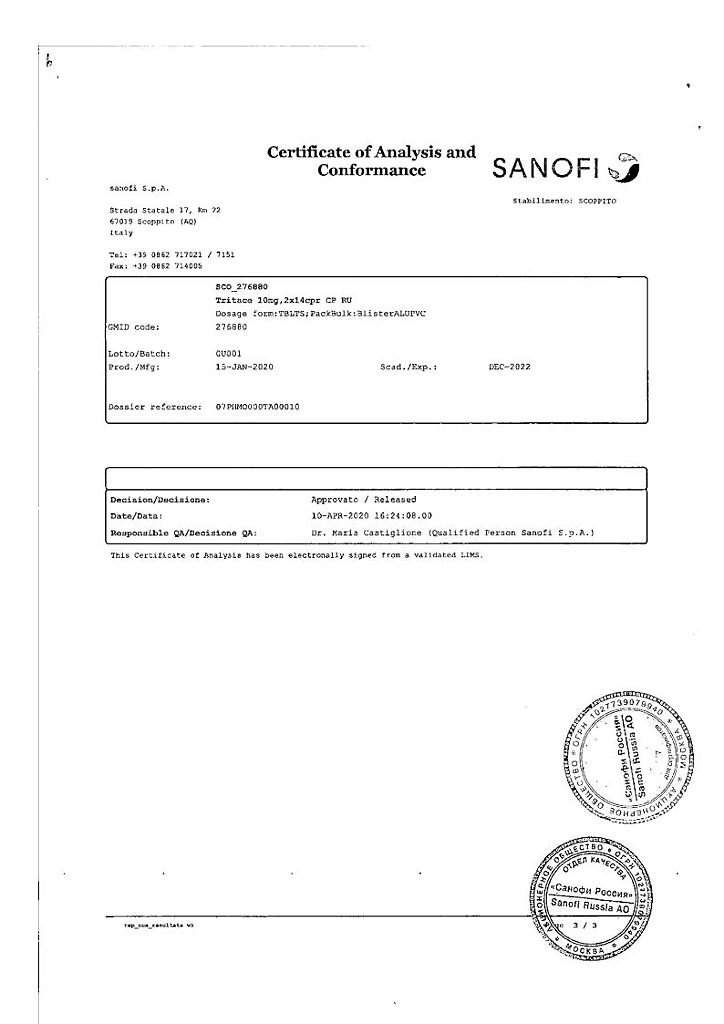
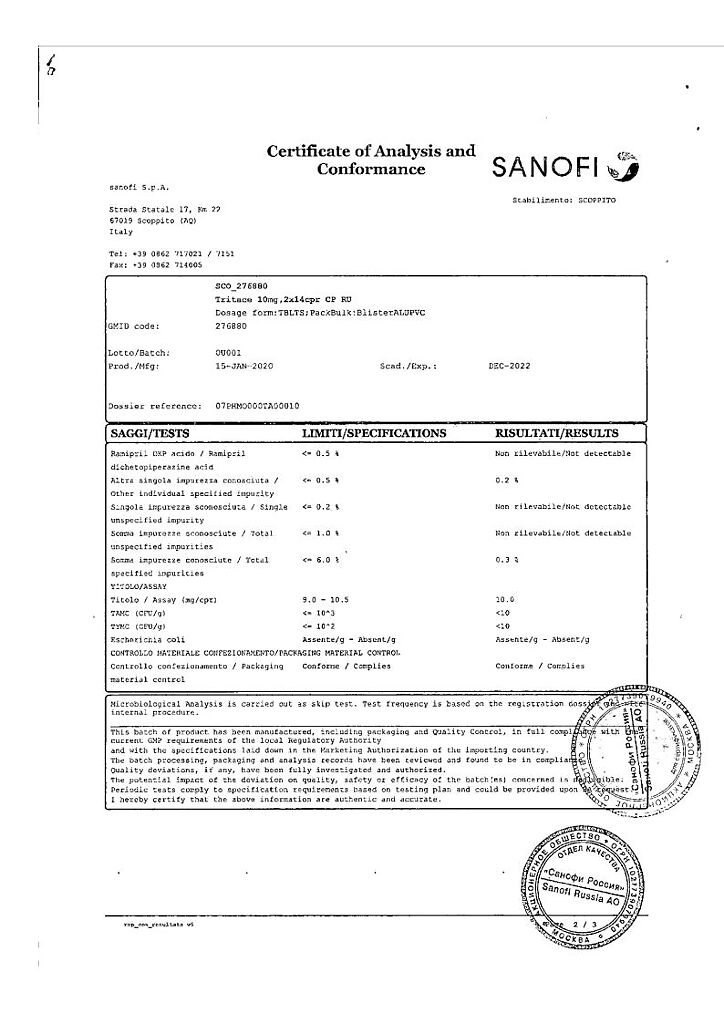
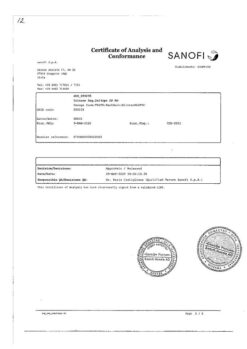
Tritace, 10 mg tablets 28 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Tritace is an antihypertensive drug, an ACE inhibitor. Ramiprilat, the active metabolite of ramipril, is a long-acting ACE inhibitor. In blood plasma and tissues this enzyme catalyzes the transition of angiotensin I into angiotensin II (active vasoconstrictor) and the cleavage of the active vasodilator bradykinin.
Decreasing angiotensin II formation and increasing bradykinin activity leads to vasodilation and contributes to the cardioprotective and endothelioprotective effects of ramipril. Angiotensin II stimulates the release of aldosterone, in this regard, ramipril causes reduction of aldosterone secretion.
The administration of ramipril leads to a significant decrease in RPS, generally without causing changes in renal blood flow and glomerular filtration rate.
The administration of ramipril causes a decrease in BP in both the supine and standing positions without a compensatory increase in HR. Hypotensive effect starts 1-2 h after oral administration of a single dose of the drug and lasts for 24 h.
The maximal antihypertensive effect of Tritace usually develops by 3-4 weeks of continuous drug administration and is maintained for a long time. Sudden discontinuation of the drug does not lead to a rapid and significant increase in BP.
The use of the drug reduces mortality (including sudden death), the risk of development of severe heart failure, reduces the number of hospitalizations of patients with clinical signs of chronic heart failure after acute myocardial infarction.
In patients with diabetic and nondiabetic clinically significant nephropathy the drug decreases rate of progression of renal failure, and in preclinical stage of diabetic and nondiabetic nephropathy ramipril decreases albuminuria. The drug favorably influences carbohydrate metabolism and lipid profile, causes reduction of marked myocardial and vascular wall hypertrophy.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
1 tablet contains:
ramipril 5 mg.
Excipients:
Hypromellose,
Pregelatinized starch,
microcrystalline cellulose,
sodium stearyl fumarate,
red iron oxide dye.
How to take, the dosage
How to take, the dosage
Arterial hypertension: oral, initial dose is 2.5 mg, once, in the morning, on an empty stomach or twice daily.
In case of insufficient hypotensive effect, the dose is gradually increased every 2-3 weeks.
The maximum daily dose is 10 mg, the maintenance dose is 2.5-5 mg.
In case of absence of optimal BP lowering diuretic drugs are prescribed additionally. CHF: the initial dose is 1.25 mg/day; if necessary, increase the dose to 2.5 mg for 1-2 weeks.
When treating patients who have had a myocardial infarction, the initial dose is 2.5 mg twice daily (in case of poor tolerance, 1.25 mg for the first 2 days).
Renal failure (CKD 30-60 ml/min), age over 65 years, diabetes mellitus: initial dose is 1.25 mg, maintenance dose is 2.5 mg; maximum dose is 5 mg/day.
Interaction
Interaction
In concomitant use with Tritace of potassium salts, potassium-saving diuretics (e.g., amiloride, triamterene, spironolactone) hyperkalemia is observed (serum potassium control is necessary).
The concomitant use of Tritace with antihypertensive agents (in particular diuretics) and other drugs that reduce BP leads to increased effect of ramipril.
Concomitant use with hypnotics, opioids and analgesics may cause a sharp decrease in BP.
Vasopressor sympathomimetic drugs (epinephrine) and estrogens may cause attenuation of the action of ramipril.
When Tritace is used concomitantly with allopurinol , procainamide, cytostatic agents, immunosuppressants, systemic GCS and other drugs that may change the blood count, a decrease in the number of leukocytes in the blood may occur.
Concomitant use with lithium preparations may increase the concentration of lithium in plasma, which leads to increased cardio- and neurotic effects of lithium.
In concomitant use of Tritace with oral hypoglycemic agents (sulfonylurea derivatives, biguanides), insulin an increase in hypoglycemia occurs. NSAIDs (indomethacin, acetylsalicylic acid) may decrease the effectiveness of ramipril.
Concomitant use with heparin may increase the concentration of potassium in the blood serum.
Baking salt decreases the effectiveness of ramipril. Ethanol increases the hypotensive effect of ramipril.
Special Instructions
Special Instructions
After the first dose, as well as when increasing the dose of diuretic and/or ramipril, patients should be under medical supervision for 8 hours to avoid the development of an uncontrolled hypotensive reaction.
In patients with CHF the use of the drug may lead to the development of severe arterial hypotension, which in some cases is accompanied by oliguria or azotemia and rarely by the development of acute renal failure.
The lower limit of systolic BP for therapy in early myocardial infarction is 100 mm Hg.
Patients with malignant arterial hypertension or concomitant decompensated CHF should start treatment in a hospital setting.
Before and during therapy with ACE inhibitors, total leukocyte count and leukocyte formula determination are necessary (up to once a month during the first 3-6 months of treatment in patients with increased risk of neutropenia – with impaired renal function, systemic connective tissue diseases or those receiving high doses, as well as during first signs of infection).
In case of confirmation of neutropenia (neutrophil count is less than 2,000/μL) therapy with ACE inhibitors should be stopped.
Prenatal blood pressure, renal function (creatinine, urea), K+ and other electrolytes in plasma, Hb, activity of liver enzymes in blood should be monitored before and during treatment.
We should be careful when prescribing the drug to patients on low-salt or no-salt diet (increased risk of arterial hypotension).
In patients with decreased circulatory blood pressure (as a result of diuretic therapy), with restriction of salt intake, during dialysis, with diarrhea and vomiting the development of symptomatic hypotension is possible.
Transient hypotension is not contraindication for continuation of treatment after BP stabilization.
In case of recurrence of severe hypotension, the dose should be reduced or the drug should be discontinued.
The use of AN69 dialysis membranes in combination with ACE inhibitors is not recommended (because of the possibility of anaphylactoid reactions in patients).
If a history of angioedema unrelated to ACE inhibitors is indicated, there is still an increased risk of developing it when taken in such patients.
Safety and efficacy in pediatric practice: In newborns who have had intrauterine exposure to ACE inhibitors, close monitoring is recommended to detect hypotension, oliguria, and hyperkalemia.
In oliguria, BP and renal perfusion should be maintained by administration of appropriate fluids and vasoconstrictors. Newborns and infants are at risk for oliguria and neurologic impairment, possibly due to decreased renal and cerebral blood flow due to decreased BP caused by ACE inhibitors (received by pregnant women and after delivery); lower initial doses and close monitoring are recommended.
Caution should be exercising or in hot weather because of the risk of dehydration and arterial hypotension due to reduced fluid volume.
Ethanol is not recommended. The surgeon/anesthesiologist should be warned about the use of ACE inhibitors before surgical procedures (including dentistry).
At the time of treatment, caution should be exercised when driving motor transport and engaging in other potentially dangerous activities requiring increased concentration and rapid psychomotor reactions (dizziness is possible, especially after the initial dose of ACE inhibitor in patients taking diuretic drugs).
Contraindications
Contraindications
Hypersensitivity to ramipril or other ACE inhibitors. ACE inhibitors, history of angioedema on ACE inhibitor therapy, hereditary or idiopathic angioedema, bilateral renal artery stenosis, single renal artery stenosis, post renal transplantation, hemodynamically significant aortic or mitral stenosis, GOCMP, primary hyperaldosteronism, pregnancy, lactation.
With caution.
Severe lesions of coronary and cerebral arteries (danger of decreased blood flow with excessive BP reduction), unstable angina pectoris, severe ventricular rhythm disorders, end-stage CHF, decompensated “pulmonary” heart, diseases requiring GCS and immunosuppressants (no clinical experience) – including.including systemic connective tissue diseases, renal and/or hepatic insufficiency, hyperkalemia, hyponatremia (including with diuretics and diet limiting Na+ intake), conditions accompanied with BOD reduction (including diarrhea, vomiting), elderly age, age 18 years (safety and effectiveness of use have not been studied).
Side effects
Side effects
The following adverse effects are given in accordance with the following gradations of their frequency of occurrence: very often (â¥10%), often (â¥1%
Cardiovascular system: frequent – excessive BP decrease, impaired orthostatic regulation of vascular tone (orthostatic hypotension), syncopal states; sometimes – myocardial ischemia, including development of angina attack or myocardial infarction, tachycardia, arrhythmias (appearance or increase), palpitation, peripheral edema, blood flushes to the face; rare – occurrence or exacerbation of circulatory disorders against the background of stenotic vascular lesions, vasculitis; frequency is unknown – Raynaud’s syndrome.
CNS disorders: frequent – headache, feeling of “lightness” in the head; sometimes – dizziness, agueusia (loss of taste sensitivity), dysgeusia (impaired taste sensitivity), depressed mood, anxiety, nervousness, motor anxiety, sleep disorders, including drowsiness; rarely – tremor, balance disorder, confusion; frequency unknown – cerebral ischemia, including ischemic stroke and transient cerebral circulation disorder, psychomotor reactions, paresthesia (burning sensation), parosmia (smell perception disorder), attention disorder.
Sides of the visual organ: sometimes – visual disorders, including blurred vision; rarely – conjunctivitis.
Hearing organ: rare – hearing disorders, tinnitus.
Respiratory system: often – dry cough (increasing at night and when lying down), bronchitis, sinusitis, shortness of breath; sometimes – bronchospasm, including aggravation of bronchial asthma, nasal congestion.
The digestive system: often – inflammatory reactions in the stomach and intestines, digestive disorders, abdominal discomfort, dyspepsia, diarrhea, nausea, vomiting; sometimes – pancreatitis, including death. with fatal outcome (cases of pancreatitis with fatal outcome while taking ACE inhibitors were extremely rarely observed), increased pancreatic enzyme activity in blood plasma, intestinal angioneurotic edema, abdominal pain, gastritis, constipation, dry oral mucosa; rarely – glossitis; frequency is unknown – aphthous stomatitis (inflammatory reaction of oral mucosa).
Hepatobiliary system: sometimes – increase of liver enzymes activity and concentration of conjugated bilirubin in blood plasma; rarely – cholestatic jaundice, hepatocellular lesions; frequency is unknown – acute liver failure, cholestatic or cytolytic hepatitis (lethal outcome was observed extremely rarely).
Renal and urinary tract disorders: sometimes – renal dysfunction, including development of acute renal failure, increased urine excretion, increased pre-existing proteinuria, increased concentration of urea and creatinine in blood.
Reproductive system and mammary glands: sometimes – transient impotence due to erectile dysfunction, decreased libido; frequency unknown: gynecomastia.
Hematopoietic system: sometimes – eosinophilia; rarely – leukopenia, including neutropenia and agranulocytosis, decrease of erythrocytes in peripheral blood, decrease of hemoglobin concentration, thrombocytopenia; frequency of unknown – suppression of medullar hemopoiesis, pancytopenia, hemolytic anemia.
Skin and mucous membranes: frequently – skin rash (maculopapular); sometimes – angioedema, including lethal. with fatal outcome (laryngeal edema can cause airway obstruction, leading to death), skin itching, hyperhidrosis; rarely – exfoliative dermatitis, urticaria, onycholysis; very rare – photosensitization reactions; frequency unknown – toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme, pemphigus, worsening the course of psoriasis, psoriasis-like dermatitis, pemphigoid or lichenoid (lichen-like) exanthema or enanthema, alopecia.
Muscular system disorders: often – muscle cramps, myalgia; sometimes – arthralgia.
Disorders of metabolism, nutrition and laboratory parameters: frequent – increased blood potassium concentration; sometimes – anorexia, decreased appetite; frequency unknown – decreased blood sodium concentration.
Immune system disorders: frequency unknown – anaphylactic or anaphylactoid reactions (when ACE inhibition increases the number of anaphylactic or anaphylactoid reactions to insect venoms), increased concentration of antinuclear antibodies.
General disorders: often – chest pain, feeling of fatigue; sometimes – increase in body temperature; rarely – asthenia (weakness).
Overdose
Overdose
Symptoms: marked BP decrease, shock, marked bradycardia, disorders of water-electrolyte balance, acute renal failure, stupor.
Treatment: gastric lavage, adsorbents, sodium sulfate administration (if possible during the first 30 minutes). If arterial hypotension develops, the therapy for the replenishment of the blood circulation volume and restoration of salt balance may be supplemented by administration of alpha 1-adrenergic stimulants (norepinephrine, dopamine) and angiotensin II (angiotensinamide).
Similarities
Similarities
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | Sanofi S.p.A., Italy |
| Medication form | pills |
| Brand | Sanofi S.p.A. |
Other forms…
Related products
Buy Tritace, 10 mg tablets 28 pcs with delivery to USA, UK, Europe and over 120 other countries.