No products in the cart.
Triplixam, 10 mg+2, 5 mg+10 mg 30 pcs
€27.12 €22.60
Description
Triplixam® is a combination drug that includes three antihypertensive components, each of which complements the action of the others to control BP in patients with arterial hypertension. Amlodipine is a “slow” calcium channel blocker (CMCB), a dihydropyridine derivative, indapamide is a sulfonamide diuretic, perindopril arginine is an inhibitor of the enzyme that converts angiotensin I to angiotensin II (ACE inhibitor).
The pharmacological properties of Triplixam® combine the properties of each of its active ingredients. In addition, the combination of amlodipine, indapamide and perindopril arginine enhances the antihypertensive effect of each component.
The mechanism of action
Amlodipine is a DMARD, a dihydropyridine derivative. Amlodipine inhibits transmembrane transition of calcium ions in cardiomyocytes and smooth muscle cells of the vascular wall.
Indapamide refers to sulfonamide derivatives with an indole ring and has pharmacological properties similar to thiazide diuretics, which inhibit sodium ion reabsorption in the cortical segment of the nephron loop. The renal excretion of sodium and chlorine ions and, to a lesser extent, potassium and magnesium ions increases, which is accompanied by increased diuresis and antihypertensive effect.
Perindopril is an inhibitor of the enzyme that converts angiotensin I to angiotensin II (ACE inhibitor). ACE, or kininase II, is an exopeptidase that converts angiotensin I into the vasoconstrictor angiotensin II. In addition, the enzyme stimulates the production of aldosterone by the adrenal cortex and the degradation of bradykinin, which has a vasodilator effect, to an inactive heptapeptide. The result is perindopril:
– reduces aldosterone secretion;
– by the principle of negative feedback increases plasma renin activity;
– with prolonged use, it reduces RPS, which is mainly due to the effect on the vessels in the muscles and kidneys. These effects are not accompanied by retention of sodium ions or fluid or development of reflex tachycardia with long-term use.
Perindopril has antihypertensive effects in patients with both low and normal plasma renin activity.
Perindopril has therapeutic effect due to the active metabolite perindoprilat. Other metabolites have no pharmacological activity.
Perindopril normalizes heart function by reducing preload and postload due to:
– vasodilatory action on the veins, possibly related to activation of the prostaglandin system;
– a decrease in RPS.
In the study of hemodynamic parameters in patients with chronic heart failure (CHF) it was revealed:
– decreased filling pressure in the left and right ventricles of the heart;
– decreased PPSS;
– increased cardiac output and increased cardiac index;
– increased muscular peripheral blood flow.
There was also an increase in exercise tolerance.
Pharmacodynamic effects
Amlodipine
The antihypertensive effects of amlodipine are due to a direct effect on the smooth muscle cells of the vascular wall. The detailed mechanism by which amlodipine exerts antianginal action is not well established, but it is known that amlodipine reduces the overall coronary burden through two actions:
-causes peripheral arterioles to dilate, decreasing the ROSS (post-load). This reduction of cardiac load reduces energy expenditure, and myocardial oxygen demand;
– causes dilation of coronary arteries and arterioles in both ischemic and intact areas. At the same time in patients with coronary artery spasm (Prinzmetal’s angina) coronary blood flow and myocardial oxygen supply are improved.
In patients with arterial hypertension (AH), taking amlodipine once daily provides a clinically significant reduction in BP in the “standing” and “lying” position for 24 hours. The antihypertensive effect develops slowly, and therefore the development of acute arterial hypotension is uncommon.
Amlodipine has no adverse metabolic effects and does not affect indexes of lipid metabolism. It does not cause changes in hypolipidemic indexes of blood plasma and can be used in patients with concomitant bronchial asthma, diabetes mellitus and gout.
Indapamide
A 24-hour antihypertensive effect has been demonstrated when using indapamide in monotherapy. The antihypertensive effect is seen when the drug is used in doses that have minimal diuretic effect.
The antihypertensive activity of indapamide is associated with improvement of elastic properties of large arteries, reduction of arteriolar and total peripheral vascular resistance.
Indapamide reduces left ventricular hypertrophy.
The thiazide and thiazide-like diuretics reach a plateau of therapeutic effect at a certain dose, whereas the incidence of side effects continues to increase with further increasing of the drug dose. Therefore, do not increase the dose of the drug if the therapeutic effect is not achieved at the recommended dose.
In short-, medium-, and long-term studies involving patients with arterial hypertension, it has been shown that indapamide:
-does not affect lipid metabolism parameters, including triglyceride levels.including triglycerides, cholesterol, LDL and HDL levels;
– has no effect on parameters of carbohydrate metabolism, including in patients with diabetes mellitus.
Perindopril
Perindopril is effective in therapy of arterial hypertension of any degree of severity. Against the background of its use there is a decrease of both systolic and diastolic BP in “lying” and “standing” position.
The antihypertensive effect of the drug reaches the maximum 4-6 hours after a single oral administration and lasts for 24 hours.
24 hours after oral administration there is significant (about 80%) residual ACE inhibition.
In patients with a positive response to treatment, normalization of BP occurs within a month and persists without the development of tachycardia.
The cessation of treatment is not accompanied by the development of a “ricochet” effect.
Perindopril has a vasodilator effect, helps to restore elasticity of large arteries and vascular wall structure of small arteries, and reduces left ventricular hypertrophy.
The simultaneous administration of thiazide diuretics increases the severity of the antihypertensive effect.
In addition, combination of ACE inhibitor and thiazide diuretic also decreases the risk of hypokalemia when taking diuretics.
Perindopril/indapamide
In patients with arterial hypertension, regardless of age, the combination of perindopril and indapamide has a dose-dependent antihypertensive effect on both diastolic and systolic BP in standing and lying position. Clinical studies have shown a more pronounced antihypertensive effect with combined therapy with perindopril and indapamide compared to monotherapy with separate components.
Clinical efficacy and safety
The effect of Triplixam® on morbidity and mortality has not been studied.
The efficacy and safety of amlodipine at 2.5-10 mg/day, the ACE inhibitor lisinopril at 10-40 mg/day as a first-line drug and the thiazide diuretic chlorthalidone at 12.5-25 mg/d was studied in the 5-year ALLHAT trial (involving 33,357 patients aged 55 years or older) in patients with mild to moderate AH and at least one additional risk factor for coronary complications, such as myocardial infarction or stroke suffered more than 6 months before study inclusion or other confirmed cardiovascular disease of atherosclerotic genesis; type 2 diabetes mellitus; high-density lipoprotein cholesterol (HDL-C) concentration less than 35 mg/dL; left ventricular hypertrophy by ECG or echocardiography; smoking.
The main criterion for efficacy assessment is the combined rate of fatal outcomes from CHD and the rate of nonfatal myocardial infarction. No significant differences were found between amlodipine and chlorthalidone groups according to the main evaluation criterion. The incidence of heart failure was significantly higher in the amlodipine group than in the chlorthalidone group, 10.2% and 7.7%, but the overall incidence of death was not significantly different in the amlodipine and chlorthalidone groups.
Perindopril/indapamide
In a study involving patients with arterial hypertension and left ventricular hypertrophy (left ventricular mass index >120 g/m2 in men and >100 g/m2 in women) the efficacy of therapy with 2 mg perindopril tert-butylamine (corresponding to 2.5 mg perindopril arginine) in combination with 0.625 mg indapamide compared with monotherapy with 10 mg enalapril, when taken once daily for 1 year, was evaluated by echocardiography. If necessary, titration of doses of perindopril tertbutylamine to 8 mg (corresponding to 10 mg perindopril arginine) and indapamide to 2.5 mg once daily or enalapril to 40 mg once daily was performed to maintain adequate BP control. In the perindopril/indapamide group, no dose increase was required in 34% of patients compared with 20% in the enalapril group.
At the end of treatment, left ventricular mass index values decreased more significantly in the perindopril/indapamide group (-10.1 g/m2) compared with the enalapril group (-1.1 g/m2).
The best effect on left ventricular mass index values was achieved with higher doses of the combination of perindopril and indapamide.
In terms of BP values, the difference between the groups was 5.8 mmHg for systolic BP and 2.3 mmHg for diastolic BP, respectively, in favor of the perindopril/indapamide group.
A study involving patients with type 2 diabetes mellitus examined the effect of lowering BP on the incidence of macrovascular events (death from cardiovascular causes, nonfatal myocardial infarction, non
fatal stroke) and microvascular complications (occurrence or worsening of the course of nephropathy and eye disease) in patients taking perindopril/indapamide combination compared with placebo, on standard therapy, as well as those taking modified-release gliclazide compared with standard therapy to maintain blood glucose levels in the normal range.
After 4.3 years of therapy, the relative risk of macrovascular and microvascular complications was reduced by 9% in the group taking the perindopril/indapamide combination. The benefit was achieved by a significant reduction in the relative risk of mortality by 14%, death due to cardiovascular causes by 18%, and renal complications by 21% in the group of patients receiving the perindopril/indapamide combination compared with placebo.
The subgroup of patients with arterial hypertension showed a 9% significant reduction in the relative risk of combined incidence of macrovascular and microvascular complications in the group receiving perindopril/indapamide combination compared to placebo.
The relative risk of mortality (by 16%), death due to cardiovascular causes (by 20%), and renal complications (by 20%) was also significantly reduced in this group in patients receiving perindopril/indapamide combination compared to patients receiving placebo.
The benefits of hypotensive therapy were independent of the benefits achieved on intensive glycemic control.
Double RAAS blockade
There are data from clinical trials of combination therapy with an ACE inhibitor with ARA II.
There have been clinical studies involving patients with a history of cardiovascular or cerebrovascular disease, or type 2 diabetes with confirmed target organ damage, as well as studies involving patients with type 2 diabetes and diabetic nephropathy.
These studies found no significant positive effect on the occurrence of renal and/or cardiovascular complications and mortality rates in patients receiving combination therapy, while the risk of hyperkalemia, acute renal failure and/or arterial hypotension increased compared to patients receiving monotherapy.
Given the similar within-group pharmacodynamic properties of ACE inhibitors and ARA II, these results would be expected for any other drug interaction between ACE inhibitors and ARA II classes.
Therefore, ACE inhibitors and ARA II should not be used concomitantly in patients with diabetic nephropathy.
There are data from a clinical trial investigating the beneficial effects of adding aliskiren to standard therapy with an ACE inhibitor or ARA II in patients with type 2 diabetes and chronic kidney disease or cardiovascular disease, or with a combination of these conditions. The study was terminated early due to an increased risk of adverse outcomes. Cardiovascular death and stroke occurred more frequently in the group of patients receiving aliskiren compared to the placebo group. Also adverse events and serious adverse events of special interest (hyperkalemia, arterial hypotension and renal dysfunction) were registered more frequently in the aliskiren group than in the placebo group.
Indications
Indications
Triplixam ® is indicated for the treatment of arterial hypertension in patients who require treatment with perindopril, indapamide and amlodipine in a fixed dose combination.
Pharmacological effect
Pharmacological effect
Triplixam® is a combination drug that includes three antihypertensive components, each of which complements the action of the others in controlling blood pressure in patients with arterial hypertension. Amlodipine is a slow calcium channel blocker (SCBC), a dihydropyridine derivative, indapamide is a sulfonamide diuretic, perindopril arginine is an inhibitor of the enzyme that converts angiotensin I into angiotensin II (ACE inhibitor).
The pharmacological properties of Triplixam® combine the properties of each of its active ingredients. In addition, the combination of amlodipine, indapamide and perindopril arginine enhances the antihypertensive effect of each component.
Mechanism of action
Amlodipine is a BMCC, a dihydropyridine derivative. Amlodipine inhibits the transmembrane transition of calcium ions into cardiomyocytes and smooth muscle cells of the vascular wall.
Indapamide is a sulfonamide derivative with an indole ring and is similar in pharmacological properties to thiazide diuretics, which inhibit the reabsorption of sodium ions in the cortical segment of the nephron loop. At the same time, the kidneys excrete sodium and chloride ions and, to a lesser extent, potassium and magnesium ions, which is accompanied by an increase in diuresis and an antihypertensive effect.
Perindopril is an inhibitor of the enzyme that converts angiotensin I into angiotensin II (ACE inhibitor). ACE, or kininase II, is an exopeptidase that converts angiotensin I into the vasoconstrictor angiotensin II. In addition, the enzyme stimulates the production of aldosterone by the adrenal cortex and the destruction of bradykinin, which has a vasodilator effect, to an inactive heptapeptide. As a result, perindopril:
– reduces the secretion of aldosterone;
– according to the principle of negative feedback, it increases the activity of renin in the blood plasma;
– with long-term use, it reduces the peripheral vascular resistance, which is mainly due to the effect on the vessels in the muscles and kidneys. These effects are not accompanied by sodium or fluid retention or the development of reflex tachycardia with prolonged use.
Perindopril has an antihypertensive effect in patients with both low and normal plasma renin activity.
Perindopril has a therapeutic effect due to the active metabolite perindoprilat. Other metabolites do not have pharmacological activity.
Perindopril normalizes heart function, reducing preload and afterload thanks to:
– vasodilating effect on veins, possibly associated with activation of the prostaglandin system;
– decrease in OPSS.
When studying hemodynamic parameters in patients with chronic heart failure (CHF), it was revealed:
– decrease in filling pressure in the left and right ventricles of the heart;
– decrease in OPSS;
– increased cardiac output and increased cardiac index;
– increased muscle peripheral blood flow.
Exercise tolerance also increased.
Pharmacodynamic effects
Amlodipine
The antihypertensive effect of amlodipine is due to a direct effect on the smooth muscle cells of the vascular wall. The detailed mechanism by which amlodipine exerts its antianginal effect is not well established, but amlodipine is known to reduce overall ischemic burden through two actions:
– causes expansion of peripheral arterioles, reducing peripheral vascular resistance (afterload). This reduction in the load on the heart reduces energy consumption and the myocardium’s need for oxygen;
– causes expansion of the coronary arteries and arterioles in both ischemic and intact zones. At the same time, in patients with spasm of the coronary arteries (Prinzmetal’s angina), coronary blood flow and oxygen supply to the myocardium improves.
In patients with arterial hypertension (AH), taking amlodipine 1 time per day provides a clinically significant decrease in blood pressure in the standing and lying position for 24 hours. The antihypertensive effect develops slowly, and therefore the development of acute arterial hypotension is uncharacteristic.
Amlodipine does not have undesirable metabolic effects and does not affect lipid metabolism, does not cause changes in lipid-lowering parameters of blood plasma and can be used in patients with concomitant bronchial asthma, diabetes mellitus and gout.
Indapamide
When indapamide was used as monotherapy, a 24-hour antihypertensive effect was demonstrated. The antihypertensive effect occurs when the drug is used in doses that have a minimal diuretic effect.
The antihypertensive activity of indapamide is associated with an improvement in the elastic properties of large arteries, a decrease in arteriolar and total peripheral vascular resistance.
Indapamide reduces left ventricular hypertrophy.
Thiazide and thiazide-like diuretics at a certain dose reach a plateau of therapeutic effect, while the frequency of side effects continues to increase with further increases in the dose of the drug. Therefore, you should not increase the dose of the drug if a therapeutic effect is not achieved when taking the recommended dose.
In short-term, intermediate-term and long-term studies in patients with hypertension, indapamide has been shown to:
– does not affect lipid metabolism indicators, incl. on the level of triglycerides, cholesterol, LDL and HDL;
– does not affect carbohydrate metabolism, incl. in patients with diabetes mellitus.
Perindopril
Perindopril is effective in the treatment of arterial hypertension of any severity. Against the background of its use, there is a decrease in both systolic and diastolic blood pressure in the “lying” and “standing” positions.
The antihypertensive effect of the drug reaches its maximum 4-6 hours after a single oral dose and persists for 24 hours.
24 hours after oral administration, pronounced (about 80%) residual ACE inhibition is observed.
In patients with a positive response to treatment, normalization of blood pressure occurs within a month and is maintained without the development of tachycardia.
Discontinuation of treatment is not accompanied by the development of a rebound effect.
Perindopril has a vasodilating effect, helps restore the elasticity of large arteries and the structure of the vascular wall of small arteries, and also reduces left ventricular hypertrophy.
The simultaneous administration of thiazide diuretics increases the severity of the antihypertensive effect.
In addition, the combination of an ACE inhibitor and a thiazide diuretic also reduces the risk of hypokalemia while taking diuretics.
Perindopril/Indapamide
In patients with arterial hypertension, regardless of age, the combination of perindopril and indapamide has a dose-dependent antihypertensive effect on both diastolic and systolic blood pressure in the standing and lying position. Clinical studies have shown a more pronounced antihypertensive effect during combination therapy with perindopril and indapamide compared to monotherapy with the individual components.
Clinical efficacy and safety
The effect of Triplixam® on morbidity and mortality has not been studied.
Amlodipine
The effectiveness and safety of amlodipine at a dose of 2.5-10 mg/day, the ACE inhibitor lisinopril at a dose of 10-40 mg/day as a first-line drug, and the thiazide diuretic chlorthalidone at a dose of 12.5-25 mg/day was studied in the 5-year ALLHAT study (involving 33,357 patients aged 55 years and older) in patients with mild or moderate hypertension and at least one of the additional risk factors for coronary complications, such as: myocardial infarction or stroke suffered more than 6 months before inclusion in the study, or other confirmed cardiovascular disease of atherosclerotic origin; diabetes mellitus type 2; high-density lipoprotein cholesterol (HDL-C) concentration less than 35 mg/dL; left ventricular hypertrophy according to ECG or echocardiography; smoking.
The main criterion for assessing effectiveness is a combined indicator of the incidence of deaths from coronary artery disease and the incidence of non-fatal myocardial infarction. There were no significant differences between the amlodipine and chlorthalidone groups according to the main evaluation criterion. The incidence of heart failure in the amlodipine group was significantly higher than in the chlorthalidone group – 10.2% and 7.7%, but the overall incidence of death in the amlodipine and chlorthalidone groups did not differ significantly.
Perindopril/Indapamide
In a study involving patients with arterial hypertension and left ventricular hypertrophy (left ventricular mass index >120 g/m2 in men and >100 g/m2 in women), the effectiveness of therapy with 2 mg perindopril tertbutylamine (corresponding to 2.5 mg perindopril arginine) in combination with 0.625 mg indapamide compared with 10 mg enalapril monotherapy, when taken once a day for 1 year, assessed by echocardiography. If necessary, to maintain adequate control of blood pressure, doses of perindopril tertbutylamine were titrated to 8 mg (corresponding to 10 mg of perindopril arginine) and indapamide to 2.5 mg 1 time / day or enalapril to 40 mg 1 time / day. In the group of patients taking perindopril/indapamide, no dose increase was required in 34% of patients compared to 20% in the group taking enalapril.
At the end of treatment, left ventricular mass index values decreased more significantly in the perindopril/indapamide group (-10.1 g/m2) compared to the enalapril group (-1.1 g/m2).
The best effect on left ventricular mass index values was achieved with higher doses of the combination of perindopril and indapamide.
In terms of blood pressure reduction, the difference between the groups was 5.8 mmHg. for systolic pressure and 2.3 mm Hg. for diastolic pressure, respectively, in favor of the perindopril/indapamide group.
A study in patients with type 2 diabetes examined the effect of lowering blood pressure on the incidence of macrovascular events (death due to cardiovascular causes, non-fatal myocardial infarction, non
fatal stroke) and microvascular complications (emergence or worsening of nephropathy and eye diseases) in patients taking the perindopril/indapamide combination compared with placebo against the background of standard therapy, and also taking modified-release gliclazide compared with standard therapy aimed at maintaining normal blood glucose levels.
After 4.3 years of therapy, the relative risk of macro- and microvascular complications decreased by 9% in the group taking the perindopril/indapamide combination. The benefit was achieved due to a significant reduction in the relative risk of mortality by 14%, death due to cardiovascular causes by 18% and the development of renal complications by 21% in the group of patients receiving the perindopril/indapamide combination compared with placebo.
In the subgroup of patients with arterial hypertension, a significant 9% reduction in the relative risk of the combined incidence of macro- and microvascular complications was shown in the group taking the perindopril/indapamide combination compared with placebo.
This group also significantly reduced the relative risk of mortality (by 16%), death due to cardiovascular causes (by 20%), and renal complications (by 20%) in patients receiving the perindopril/indapamide combination compared with patients receiving placebo.
The benefits of antihypertensive therapy were independent of the benefits achieved with intensive glycemic control.
Double blockade of the RAAS
There are data from clinical studies of combination therapy using an ACE inhibitor with ARA II.
Clinical studies were conducted in patients with a history of cardiovascular or cerebrovascular disease, or type 2 diabetes mellitus accompanied by confirmed target organ damage, as well as studies in patients with type 2 diabetes mellitus and diabetic nephropathy.
These studies did not reveal a significant positive effect on renal and/or cardiovascular complications and mortality rates in patients receiving combination therapy, while the risk of hyperkalemia, acute renal failure and/or hypotension increased compared with patients receiving monotherapy.
Taking into account the similar intragroup pharmacodynamic properties of ACE inhibitors and ARB II, these results can be expected for the interaction of any other drugs, representatives of the classes of ACE inhibitors and ARA II.
Therefore, ACE inhibitors and ARB II should not be used simultaneously in patients with diabetic nephropathy.
There is clinical trial data examining the beneficial effects of adding aliskiren to standard therapy with an ACE inhibitor or angiotensin-converting enzyme II inhibitor in patients with type 2 diabetes mellitus and chronic kidney disease or cardiovascular disease, or a combination of these diseases. The study was stopped early due to an increased risk of adverse outcomes. Cardiovascular death and stroke occurred more frequently in the aliskiren group compared with the placebo group. Also, adverse events and serious adverse events of special interest (hyperkalemia, hypotension, and renal dysfunction) were reported more frequently in the aliskiren group than in the placebo group.
Special instructions
Special instructions
All the following reservations, for each component of the drug, also apply to the fixed combination of Triplixam ®.
Lithium. Concomitant use of lithium and the combination of perindopril/indapamide is usually not recommended.
Double blockade of renin-angiotensin (RAAS). There is evidence that concomitant use of ACE inhibitors, angiotensin II receptor blockers or aliskiren increases the risk of hypotension, hyperkalemia and decreased renal function (including acute renal failure). Therefore, double blockade of the RAAS by simultaneous administration of ACE inhibitors, angiotensin II receptor blockers or aliskiren is not recommended (see Section “Interaction with other drugs and other types of interactions”). If treatment with the simultaneous use of two RAAS blockers is considered absolutely necessary, it can only occur under specialist supervision and with frequent close monitoring of renal function, electrolyte levels and blood pressure. ACE inhibitors and angiotensin II receptor blockers should not be used concomitantly in patients with diabetic nephropathy.
Potassium-sparing drugs, nutritional supplements containing potassium, or salt substitutes with potassium.
Concomitant use of perindopril with potassium-sparing drugs or nutritional supplements containing potassium is not recommended.
Neutropenia / agranulocytosis / thrombocytopenia / anemia. Cases of neutropenia/agranulocytosis, thrombocytopenia and anemia have been reported among patients taking ACE inhibitors. In patients with normal renal function and in the absence of other risk factors, neutropenia rarely occurs. Perindopril should be prescribed very carefully to patients with collagen diseases, during therapy with immunosuppressants, allopurinol, procainamide, or a combination of these factors, especially if there is impaired renal function. In some of these patients, the development of serious infectious diseases was observed, in several cases resistant to intensive antibiotic therapy.
If perindopril is prescribed to such patients, it is recommended to periodically monitor the number of leukocytes in the blood. They also notify about any manifestation of an infectious disease (sore throat, fever) (see Section “Adverse Reactions”).
Hypersensitivity/angioedema. Rare cases of angioedema of the face, extremities, lips, tongue, glottis and/or larynx have been reported with the use of ACE inhibitors, including perindopril. This can happen at any time during treatment.
In such cases, it is necessary to urgently stop taking perindopril and establish the necessary monitoring of the patient’s condition until the symptoms disappear completely. If the swelling is limited to the face and lips, the patient’s condition usually improves without therapy, and antihistamines may be helpful to relieve symptoms.
Angioedema, accompanied by swelling of the larynx, can be fatal. In cases where swelling extends to the tongue, glottis or larynx with the possibility of airway obstruction, emergency treatment is urgently needed, which may include subcutaneous administration of a solution of epinephrine 1: 1000 (0.3-0.5 ml) and/or ensuring patency of the airway.
It has been reported that ACE inhibitors are more likely to cause angioedema in blacks compared to patients of other races.
After discontinuation of the ACE inhibitor, the symptoms of angioedema disappeared. When carrying out differential diagnosis of abdominal pain that occurs in patients while taking ACE inhibitors, it is necessary to take into account the likelihood of intestinal angioedema.
Anaphylactoid reactions during desensitizing therapy. Isolated cases of prolonged life-threatening anaphylactoid reactions have been reported in patients taking ACE inhibitors during desensitizing treatment with drugs containing bee and wasp venom. ACE inhibitors should be used with caution in patients with allergies after desensitization and should be avoided during immunotherapy with agents containing toxic substances of animal origin.
However, in patients requiring both ACE inhibitors and desensitization therapy, such reactions can be avoided by temporarily discontinuing the use of the ACE inhibitor at least 24 hours before desensitization.
Anaphylactoid reactions during low-density lipoprotein (LDL) plasmapheresis. Rarely, life-threatening anaphylactoid reactions have occurred in patients taking ACE inhibitors during LDL plasmapheresis using dextran sulfate. The development of the latter can be avoided if treatment with ACE inhibitors is temporarily stopped before each plasmapheresis.
Patients on hemodialysis. Cases of anaphylactoid reactions have been reported in patients taking ACE inhibitors while undergoing hemodialysis using high-flow polyacrylic membranes (eg AN 69 ® ). Such patients should be treated with a different type of dialysis membrane or a different class of antihypertensive drugs.
Hepatic encephalopathy. In patients with impaired liver function, the use of thiazide and thiazide-like diuretics can cause hepatic encephalopathy.
Patients with a history of angioedema that was not associated with the use of ACE inhibitors have an increased risk of its occurrence when taking ACE inhibitors.
Rare cases of intestinal angioedema have occurred in patients during treatment with ACE inhibitors. These patients experienced abdominal pain (with or without nausea and vomiting); in some cases, no preliminary angioedema of the face was observed, and the level of C-1 esterase was normal. The diagnosis of intestinal angioedema was made during computed tomography, ultrasound, or surgery.
In this case, the use of diuretics should be stopped immediately.
Photosensitivity. Cases of photosensitivity reactions have been reported in patients taking thiazide and thiazide-like diuretics. If such reactions occur, it is recommended to discontinue diuretic treatment. If it is necessary to resume taking diuretics, protect vulnerable areas from the sun or sources of artificial ultraviolet light.
Kidney function. Patients with severe renal failure (creatinine clearance ® containing a combination of perindopril / indapamide at a dose of 10 mg / 2.5 mg (i.e. Triplixam ® 10 mg / 2.5 mg / 5 mg and 10 mg / 2.5 mg / 10 mg). If a patient with hypertension without obvious signs of renal impairment has laboratory signs of renal failure, taking the drug is necessary stop; it is possible to resume treatment with a lower dose or one of the components of the drug. Such patients should undergo regular monitoring of potassium and creatinine: after 2 weeks from the start of treatment and subsequently every two months during the period of therapeutic stabilization, cases of renal failure were observed mainly in patients with severe heart failure or impaired renal function, including renal artery stenosis.
This combination is not recommended for use in patients with bilateral renal artery stenosis or arterial stenosis of a solitary kidney.
Risk of arterial hypotension and/or renal failure (in cases of heart failure, water and electrolyte deficiency): significant stimulation of renin-angiotensin has been observed during clearly defined water and electrolyte deficiency (strict salt-free diet or long-term diuretic treatment) in patients with low blood pressure, in cases of renal artery stenosis, congestive heart failure or in patients with cirrhosis of the liver with edema and ascites.
Blocking this system with an ACE inhibitor, especially during the first dose and during the first two weeks of treatment, can lead to a sharp decrease in blood pressure and/or an increase in plasma creatinine levels, which confirms the presence of functional renal failure.
Sometimes it can have an acute onset and appear at any time. In such cases, treatment should begin with a lower dose and gradually increase it. In patients with coronary heart disease or cerebrovascular disease, a significant decrease in blood pressure can lead to myocardial infarction or stroke.
Thiazide and thiazide-like diuretics show the greatest effectiveness if there is no or minor renal impairment (creatinine level approximately below 25 mg/l, i.e. 220 µmol/l in adults).
In elderly patients, plasma creatinine levels should be appropriate for age, weight and gender. Hypovolemia caused by loss of water and sodium due to diuretics at the beginning of treatment leads to a decrease in glomerular filtration rate. As a result, an increase in urea and creatinine levels in the blood may occur. Such transient functional renal failure has no consequences in patients with normal renal function, but may worsen existing renal failure.
Patients with renal failure can use amlodipine in normal doses. Fluctuations in the concentration of amlodipine in the blood plasma do not depend on the degree of renal failure.
Triplixam ® fixed combination has not been studied in patients with impaired renal function. For patients with renal failure, the dose of the fixed combination of Triplixam ® should correspond to the separately selected doses of the monocomponents.
Hypotension, water and electrolyte deficiency. There is a risk of a sudden decrease in blood pressure in patients with sodium deficiency (in particular in patients with renal artery stenosis). Therefore, it is necessary to systematically check for symptoms of water and electrolyte deficiency, which may occur with vomiting or diarrhea. In such patients, it is necessary to regularly monitor the level of electrolytes in the blood plasma.
If severe hypotension occurs, intravenous administration of an isotonic sodium chloride solution may be required. Transient arterial hypotension is not a contraindication for further use of the drug. After restoration of circulating blood volume (CBV) and normalization of blood pressure, treatment can be started with a low dose or one of the components of the drug.
Treatment with any diuretic may result in a decrease in plasma sodium levels, which is likely to have serious consequences. Initially, a decrease in sodium concentration may be asymptomatic, so laboratory monitoring of this indicator should be carried out regularly. More frequent monitoring is necessary for elderly patients and patients with liver cirrhosis.
Potassium level. Treatment with a combination of indapamide with perindopril and amlodipine does not exclude the possibility of hypokalemia, particularly in patients with diabetes mellitus or renal failure. As with any antihypertensive drug used together with a diuretic, plasma potassium levels should be regularly monitored.
In some patients, while taking ACE inhibitors, including perindopril, there was an increase in the concentration of potassium in the blood plasma. Risk factors for hyperkalemia include renal failure, impaired renal function, age over 70 years, diabetes mellitus, intercurrent conditions such as dehydration, acute cardiac decompensation, metabolic acidosis, and concomitant use of potassium-sparing diuretics (for example, spironolactone, eplerenone, triamterene or amiloride), dietary supplements containing potassium, or potassium salts with potassium; taking other drugs that cause an increase in the concentration of potassium in the blood plasma (for example, heparin). The use of potassium supplements, potassium-sparing diuretics, or potassium salt substitutes, especially in patients with renal impairment, may result in significant increases in plasma potassium levels. Hyperkalemia can lead to serious, sometimes fatal, arrhythmias. If concomitant use of perindopril and any of the above substances is considered appropriate, they should be used with caution and frequent monitoring of serum potassium levels.
Reduced plasma potassium levels and hypokalemia are the main risks when using thiazide and thiazide-like diuretics. In high-risk patients (elderly and/or malnourished patients, patients taking multiple medications, patients with liver cirrhosis accompanied by edema and ascites, patients with coronary artery disease and patients with heart failure), the occurrence of hypokalemia (< 3.4 mmol/l) should be prevented. In the event of hypokalemia, the cardiotoxicity of cardiac glycosides and the risk of rhythm disturbances increase. Patients who have a prolonged QT interval of congenital or iatrogenic origin are also at risk. Hypokalemia, like bradycardia, can contribute to the development of severe cardiac arrhythmias, including paroxysmal ventricular tachycardia of the “pirouette” type, which can be fatal.
Active ingredient
Active ingredient
Amlodipine, Indapamide, Perindopril
Composition
Composition
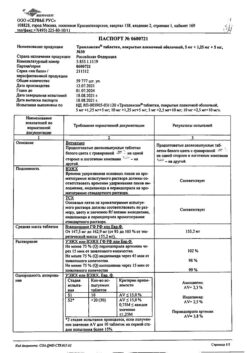
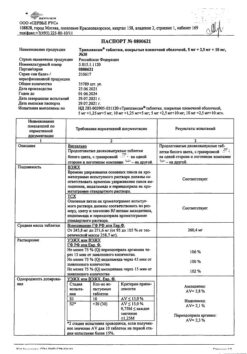
TRIPLIXAM 10 mg / 2.5 mg / 10 mg
active ingredients: 1 tablet contains perindopril arginine 10 mg (corresponding to 6.790 mg perindopril), indapamide 2.5 mg and amlodipine besylate 13.870 mg (corresponding to 10 mg amlodipine)
excipients: tablet: mixture of calcium carbonate and starch, microcrystalline cellulose, croscarmellose sodium, magnesium stearate, colloidal silicon dioxide, corn starch; film coating: glycerin, hypromellose, macrogol 6000, magnesium stearate, titanium dioxide (E 171).
Contraindications
Contraindications
Use in patients undergoing hemodialysis;
use in patients with untreated decompensated heart failure,
severe renal failure (creatinine clearance below 30 ml/min);
moderate renal failure (creatinine clearance below 60 ml/min) when taking the drug Triplixam ® containing a combination of active ingredients in doses of 10 mg / 2.5 mg / 5 mg or 10 mg / 2.5 mg / 10 mg
hypersensitivity to the active substances, other sulfonamide drugs, dihydropyridine derivatives, any other ACE inhibitor or to any excipients listed in the “Composition” section;
pregnant women or women planning to become pregnant;
breastfeeding period;
history of angioedema (Quincke’s edema) associated with previous treatment with ACE inhibitors
congenital or idiopathic angioedema
hepatic encephalopathy
severe liver dysfunction
hypokalemia
severe arterial hypotension
shock, including cardiogenic shock
left ventricular outlet obstruction (eg, severe aortic stenosis);
heart failure with unstable hemodynamics after acute myocardial infarction
simultaneous use with drugs containing the active substance aliskiren in patients with diabetes mellitus or renal failure (glomerular filtration rate 2).
Side Effects
Side Effects
The most common adverse reactions that were observed when using perindopril, indapamide and amlodipine separately are: dizziness, headache, paresthesia, vertigo, drowsiness, blurred vision, tinnitus, palpitation, hot flashes, arterial hypotension (and associated symptoms), cough, shortness of breath, gastrointestinal disorders (abdominal pain, constipation, diarrhea, dysgeusia, dyspepsia, nausea, vomiting), itching, skin rashes, maculopapular rashes, muscle spasms, asthenia, ankle swelling, edema and fatigue.
During treatment with perindopril, indapamide or amlodipine, the following adverse reactions were observed, which are distributed in frequency as follows: very often (≥ 1/10); often (≥ 1/100, 1/1000, 1/10000, < 1/1000); very rare (< 1/10000); frequency unknown (cannot be determined from available information).
Infections and infestations. Rhinitis: perindopril – very rarely, amlodipine – infrequently.
From the circulatory and lymphatic systems. Agranulocytosis: perindopril and indapamide – very rare; aplastic anemia: indapamide – very rare; pancytopenia: perindopril – very rare; leukopenia: perindopril, indapamide, amlodipine – very rare; neutropenia: perindopril – very rare; hemolytic anemia: perindopril, indapamide – very rarely; thrombocytopenia: perindopril, indapamide, amlodipine – very rare; eosinophilia: perindopril – uncommon*.
From the immune system. Hypersensitivity reactions: amlodipine – very rare, indapamide – uncommon.
From the side of metabolism and metabolism. Hyperkalemia, which disappears after discontinuation of the drug: perindopril – uncommon *; hyperglycemia: amlodipine – very rare; hypercalcemia: indapamide – very rare; hypoglycemia: perindopril – infrequently *; decreased potassium levels with hypokalemia, particularly severe in high-risk patients: indapamide – frequency unknown; hyponatremia: perindopril – uncommon * indapamide – frequency unknown.
From the mental point of view. Confusion: perindopril – very rare, amlodipine – rare; insomnia: amlodipine – infrequently; mood changes (including anxiety): amlodipine – infrequently, perindopril – infrequently; depression: amlodipine – infrequently; sleep disorders: perindopril – infrequently.
From the nervous system. Dizziness: perindopril and amlodipine – often; headache: perindopril and amlodipine – often, indapamide – rarely; paresthesia: perindopril – often, indapamide – rarely, amlodipine – infrequently; vertigo: perindopril – often, indapamide – rarely; confusion: perindopril – very rare; hypertension: amlodipine – very rare; peripheral neuropathy: amlodipine – very rare; hypoesthesia: amlodipine – infrequently; perversion of taste (dysgeusia): perindopril – often, amlodipine – infrequently; tremor: amlodipine – uncommon; fainting: perindopril – uncommon * indapamide – frequency unknown, amlodipine – uncommon; drowsiness: perindopril – infrequently * amlodipine – often, extrapyramidal disorders (extrapyramidal symptoms): amlodipine – frequency unknown; stroke, possibly due to an excessive decrease in blood pressure in high-risk patients: perindopril – very rare.
From the organs of vision. Visual impairment: perindopril – often, indapamide – frequency unknown, amlodipine – infrequently; double vision: amlodipine – infrequently; myopia: indapamide – frequency unknown; blurred vision: indapamide – frequency unknown.
From the organs of hearing and the labyrinth of the ear. Ringing in the ears: perindopril – often, amlodipine – infrequently.
From the side of the heart. Angina pectoris: perindopril – very rare; arrhythmia (including bradycardia, ventricular tachycardia and atrial fibrillation): perindopril, indapamide, amlodipine – very rarely; myocardial infarction may occur due to an excessive decrease in blood pressure in high-risk patients: perindopril and amlodipine – very rarely; palpitation: perindopril – infrequently * amlodipine – often; paroxysmal ventricular tachycardia of the “torsade de pointes” type, which can be fatal: indapamide – frequency unknown; tachycardia: perindopril – infrequently *.
From the vascular system. Hot flashes: amlodipine – often; hypotension (and associated symptoms): perindopril – often, indapamide – very rarely, amlodipine – infrequently; vasculitis: perindopril – uncommon * amlodipine – very rare.
From the respiratory system, chest and mediastinal organs. Cough: perindopril – often, amlodipine – very rarely; shortness of breath: perindopril – often, amlodipine – infrequently; bronchospasm: perindopril – infrequently; eosinophilic pneumonia: perindopril – very rare.
From the digestive system. Pain in the abdominal region: perindopril and amlodipine – often; constipation: perindopril – often, indapamide – rarely, amlodipine – infrequently; diarrhea: perindopril – often, amlodipine – infrequently; dyspepsia: perindopril – often, amlodipine – infrequently; nausea: perindopril and amlodipine – often, indapamide – rarely; vomiting: perindopril – often, indapamide and amlodipine – infrequently; dry mouth: perindopril and amlodipine – uncommon, indapamide – rare; change in the rhythm of bowel movements: amlodipine – infrequently; gum hyperplasia: amlodipine – very rare; pancreatitis perindopril, indapamide and amlodipine – very rare; gastritis: amlodipine – very rare.
From the digestive system. Hepatitis: perindopril and amlodipine – very rare, indapamide – frequency unknown; jaundice: amlodipine – very rare; liver dysfunction indapamide – very rare; in the presence of liver failure, hepatic encephalopathy may occur: indapamide – frequency unknown.
From the skin and subcutaneous tissue. Quincke’s edema: amlodipine – very rare; itching: perindopril – often, amlodipine – infrequently; rash: perindopril – often, amlodipine – infrequently; maculopapular rashes: indapamide – often; urticaria: perindopril – infrequently, indapamide and amlodipine – very rarely; angioedema: perindopril – infrequently, indapamide and amlodipine – very rarely; alopecia: amlodipine – uncommon; purpura: indapamide and amlodipine – uncommon; skin discoloration: amlodipine – uncommon; hyperhidrosis: perindopril and amlodipine – uncommon; exanthema: amlodipine – uncommon; erythema multiforme: perindopril and amlodipine – very rare; Stevens-Johnson syndrome: indapamide and amlodipine – very rare; exfoliative dermatitis: amlodipine – very rare; toxic epidermal necrolysis: indapamide – very rare; reactions and photosensitivity: perindopril – uncommon * indapamide – frequency unknown, amlodipine – very rare; possible increased manifestation of existing systemic lupus erythematosus: indapamide – frequency unknown; pemphigoid: perindopril – uncommon*.
From the musculoskeletal system and connective tissue. Muscle spasms: perindopril – often, amlodipine – infrequently; swelling of the ankles: amlodipine – often; arthralgia: perindopril – infrequently * amlodipine – infrequently; myalgia: perindopril – infrequently * amlodipine – infrequently; back pain: amlodipine – uncommon.
From the kidneys and urinary system. Impaired urination, nocturia, frequent urination: amlodipine – infrequently; acute renal failure: perindopril – very rare; renal failure: perindopril – uncommon, indapamide – very rare.
From the reproductive system and mammary glands. Erectile dysfunction: perindopril and amlodipine – uncommon; gynecomastia: amlodipine – uncommon.
General disorders. Asthenia: perindopril – often, amlodipine – infrequently; increased fatigue: indapamide – rarely, amlodipine – often; edema amlodipine – often; chest pain: perindopril – infrequently * amlodipine – infrequently; pain: amlodipine – infrequently; ailments: perindopril – infrequently * amlodipine – infrequently; peripheral edema perindopril – uncommon *; hyperthermia: perindopril – infrequently *.
Research. Increase/decrease in body weight: amlodipine – infrequently; increased bilirubin levels in the blood: perindopril – rarely; increased levels of liver enzymes: perindopril – rare, indapamide – frequency unknown, amlodipine – very rare; increased creatinine levels in the blood: perindopril – infrequently *; increased urea levels in the blood: perindopril – infrequently *; decrease in hemoglobin and hematocrit levels: perindopril – very rare; prolongation of the QT interval on the electrocardiogram: indapamide – frequency unknown; increased blood glucose levels: indapamide – frequency unknown; increased levels of uric acid in the blood: indapamide – frequency unknown.
Damage, poisoning and complications of administration. Fall: perindopril – uncommon*.
*Frequencies were calculated from clinical studies for adverse reactions that were detected based on spontaneous reports.
Report suspected adverse reactions. It is important to report suspected adverse reactions after drug registration. This will allow continued monitoring of the benefit/risk ratio. Healthcare professionals were asked to report suspected adverse reactions through the national reporting system.
Overdose
Overdose
There are no data on overdose of Triplixam ®.
For the perindopril/indapamide combination, a common adverse reaction in overdose is arterial hypotension, which can sometimes be accompanied by nausea, vomiting, convulsions, dizziness, drowsiness, confusion, oliguria, which can progress to anuria (due to hypovolemia). Disturbances in water and electrolyte balance may occur (decreased levels of potassium and sodium in the blood plasma).
First aid measures include rapid removal of the drug from the body: gastric lavage and/or administration of activated charcoal, and then restoration of water and electrolyte balance in a hospital setting until these indicators return to normal limits.
If significant hypotension occurs, the patient should be placed in a horizontal position with a low headboard. If necessary, an isotonic solution is administered intravenously or any other method of restoring blood volume is used.
Perindoprilat, the active form of perindopril, can be removed from the body by hemodialysis.
Data on deliberate overdose of amlodipine are limited.
Available data suggest that very large doses will result in excessive peripheral vasodilation and reflex tachycardia. Severe, possibly prolonged systemic hypotension and fatal shock have been reported.
Clinically significant hypotension caused by amlodipine overdose requires active cardiovascular care, in particular frequent monitoring of cardiac and respiratory function, elevation of the extremities, and monitoring of circulating blood volume and urination.
Prescribing a vasoconstrictor may be useful in restoring vascular tone and blood pressure if there are no contraindications.
Administration of calcium gluconate may help reverse the effects of calcium channel blockade.
In some cases, gastric lavage is advisable. A study in healthy volunteers showed that administration of activated charcoal 2 hours after taking 10 mg of amlodipine reduced the rate of absorption of amlodipine into the body. Since amlodipine has a high level of binding to blood proteins, hemodialysis is considered ineffective.
Manufacturer
Manufacturer
Servier Rus LLC, Russia
Additional information
| Manufacturer | Servier Rus LLC, Russia |
|---|---|
| Medication form | pills |
| Brand | Servier Rus LLC |
Other forms…
Related products
Buy Triplixam, 10 mg+2, 5 mg+10 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.