No products in the cart.
Trimetazidine MB-Teva, 35 mg 60 pcs
€13.64 €11.37
Description
Pharmacotherapeutic group: antihypoxant
ATX code: C01EB15
Pharmacological properties
Pharmacodynamics
Trimetazidine prevents intracellular decrease in adenosine triphosphatase (ATP) activity under conditions of ischemia and hypoxia, preserving energy metabolism and ensuring cell homeostasis by ensuring normal functioning of cell membrane ion channels and transmembrane sodium-potassium flow. It inhibits beta-oxidation of fatty acids by selectively blocking the enzyme 3-ketoacyl-CoA-thiolase, which enhances glucose oxidation. Cells in ischemia require less oxygen for energy in the process of glucose oxidation than in the process of beta-oxidation of fatty acids.
The switch of cellular energy metabolism from fatty acid oxidation to glucose oxidation underlies the pharmacological effects of trimetazidine. Under experimental conditions it has been shown that the drug:
- maintains the energy metabolism of the heart and neurosensory tissues under ischemia;
- reduces the severity of intracellular acidosis and changes in transmembrane ion flux occurring during ischemia;
- reduces the size of myocardial damage;
- does not adversely affect hemodynamic parameters.
In patients with ischemic heart disease, trimetazidine acts as a metabolic agent, maintaining sufficient intracellular high-energy phosphate activity in the myocardium. The anti-ischemic effect is achieved without affecting hemodynamics.
In patients with stenocardia trimetazidine:
- increases coronary reserve, thereby delaying the onset of exercise-induced ischemia beginning on day 15 of therapy;
- limits exercise-induced blood pressure fluctuations without significant changes in heart rate;
- reduces the frequency of angina attacks and the need for short-acting nitroglycerin;
- improves left ventricular contractile function in patients with coronary dysfunction.
Pharmacokinetics
When taken orally, trimetazidine is rapidly absorbed from the gastrointestinal (GI) tract, with maximum plasma concentration reached in an average of 5 hours. For more than 24 hours, the plasma concentration of trimetazidine is maintained at levels greater than or equal to 75% of maximum.
The equilibrium state of the drug concentration in blood is reached after 60 hours. Food intake has no effect on the pharmacokinetic properties of trimetazidine. The volume of distribution is 4.8 l/kg. The binding to plasma proteins is low and in vitro is 16%.
Trimetazidine is mainly excreted by the kidneys, mainly unchanged. When administered orally at a dose of 35 mg, the half-life in young healthy volunteers is on average 7 hours; in patients over 65 years of age, it is 12 hours.
The total renal clearance of trimetazidine directly correlates with creatinine clearance (CK), hepatic clearance decreases with age.
Patients over 75 years
In patients over 75 years of age, increased plasma exposure to trimetazidine may be observed as a result of age-related decline in renal function. No differences have been found regarding the safety of the drug in patients over 75 years of age compared to the general population.
Patients with impaired renal function
. Plasma exposure to trimetazidine was increased approximately 2.4-fold in patients with moderate renal dysfunction (CK 30-60 mL/min), and approximately 4-fold in patients with severe renal dysfunction (CK less than 30 mL/min) compared with healthy volunteers with normal renal function.
There were no findings regarding the safety of the drug in patients with impaired renal function compared to the general population.
Application in children and adolescents
The pharmacokinetics of trimetazidine in children and adolescents less than 18 years have not been studied.
Indications
Indications
Long-term therapy of coronary heart disease: prevention of attacks of stable angina pectoris as monotherapy or as part of combination therapy.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antihypoxic agent
ATX code: C01EB15
Pharmacological properties
Pharmacodynamics
Trimetazidine, under conditions of ischemia and hypoxia, prevents the intracellular decrease in adenosine triphosphatase (ATP) activity, preserving energy metabolism and ensuring cell homeostasis by ensuring the normal functioning of ion channels of cell membranes and transmembrane sodium-potassium flow. It inhibits beta-oxidation of fatty acids by selectively blocking the enzyme 3-ketoacyl-CoA thiolase, which enhances glucose oxidation. Cells in a state of ischemia require less oxygen to obtain energy from glucose oxidation than from beta-oxidation of fatty acids.
The switching of cellular energy metabolism from fatty acid oxidation to glucose oxidation underlies the pharmacological effects of trimetazidine. Under experimental conditions it has been shown that the drug:
supports energy metabolism of the heart and neurosensory tissues under ischemic conditions;
reduces the severity of intracellular acidosis and changes in the transmembrane ion flow that occur during ischemia;
reduces the migration and infiltration of polynuclear neutrophils in ischemic and reperfused cardiac tissues;
reduces the size of myocardial damage;
does not have an adverse effect on hemodynamic parameters.
In patients with coronary heart disease, trimetazidine acts as a metabolic agent, maintaining sufficient intracellular activity of high-energy phosphates in the myocardium. The anti-ischemic effect is achieved without affecting hemodynamics.
In patients with angina, trimetazidine:
increases coronary reserve, thereby slowing down the onset of ischemia caused by physical activity, starting from the 15th day of therapy;
limits exercise-induced blood pressure fluctuations without significant changes in heart rate;
reduces the frequency of angina attacks and the need for short-acting nitroglycerin;
improves contractile function of the left ventricle in patients with ischemic dysfunction.
Pharmacokinetics
When taken orally, trimetazidine is rapidly absorbed from the gastrointestinal tract (GIT), its maximum concentration in blood plasma is achieved on average within 5 hours. For more than 24 hours, trimetazidine plasma concentrations are maintained at levels greater than or equal to 75% of the maximum.
The equilibrium state of drug concentration in the blood is achieved after 60 hours. Food intake does not affect the pharmacokinetic properties of trimetazidine. The volume of distribution is 4.8 l/kg. The binding to plasma proteins is low and in vitro is 16%.
Trimetazidine is excreted mainly by the kidneys, mainly unchanged. When taken orally at a dose of 35 mg, the half-life in young healthy volunteers averages 7 hours, in patients over 65 years of age – 12 hours.
Total renal clearance of trimetazidine directly correlates with creatinine clearance (CC), and hepatic clearance decreases with age.
Patients over 75 years of age
In patients over 75 years of age, increased plasma exposure of trimetazidine may occur as a result of age-related decreases in renal function. No differences were found regarding the safety of the drug in patients over 75 years of age compared to the general population.
Patients with impaired renal function
Plasma exposure of trimetazidine was increased approximately 2.4-fold in patients with moderate renal impairment (creatinine clearance 30-60 ml/min), and approximately 4-fold in patients with severe renal impairment (creatinine clearance less than 30 ml/min) compared with healthy volunteers with normal renal function.
No differences were found regarding the safety of the drug in patients with impaired renal function compared to the general population.
Use in children and adolescents
The pharmacokinetics of trimetazidine in children and adolescents under 18 years of age have not been studied.
Special instructions
Special instructions
If you miss one or more doses of Trimetazidine MB-Teva, you should not take a higher dose at the next dose.
Trimetazidine MB-Teva is not intended for the relief of angina attacks, nor is it indicated as an initial treatment for unstable angina or myocardial infarction. It should not be taken before hospitalization or during the first days of hospitalization.
During an attack of angina, the pathology of the coronary vessels should be re-evaluated and the treatment used adjusted (medication and possibly revascularization).
The drug Trimetazidine MB-Teva can cause symptoms of parkinsonism (tremor, akinesia, increased muscle tone) or worsen their course. The condition of patients should be regularly monitored, especially in old age. In doubtful cases, the patient should be referred to a neurologist for appropriate examination.
The development of movement disorders, such as symptoms of parkinsonism, restless legs syndrome, tremor, unsteadiness when walking, may lead to discontinuation of trimetazidine.
The incidence of motor disorders is low, they are reversible and disappear after stopping the drug. If symptoms of parkinsonism persist more than 4 months after discontinuation of the drug, consultation with a neurologist is necessary.
With unsteady walking or low muscle tone, especially when using antihypertensive therapy, the patient may fall (see section “Side effects”).
Trimetazidine should be prescribed with caution to patients who may have increased exposure:
with moderate renal impairment (see section “Method of administration and dosage”);
in elderly patients over 75 years of age (see section “Method of administration and dosage”);
in case of severe liver dysfunction (see section “With caution”).
Impact on the ability to drive vehicles and machinery
Due to the possible development of dizziness and other side effects, caution should be exercised when driving vehicles and engaging in other activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Trimetazidine
Composition
Composition
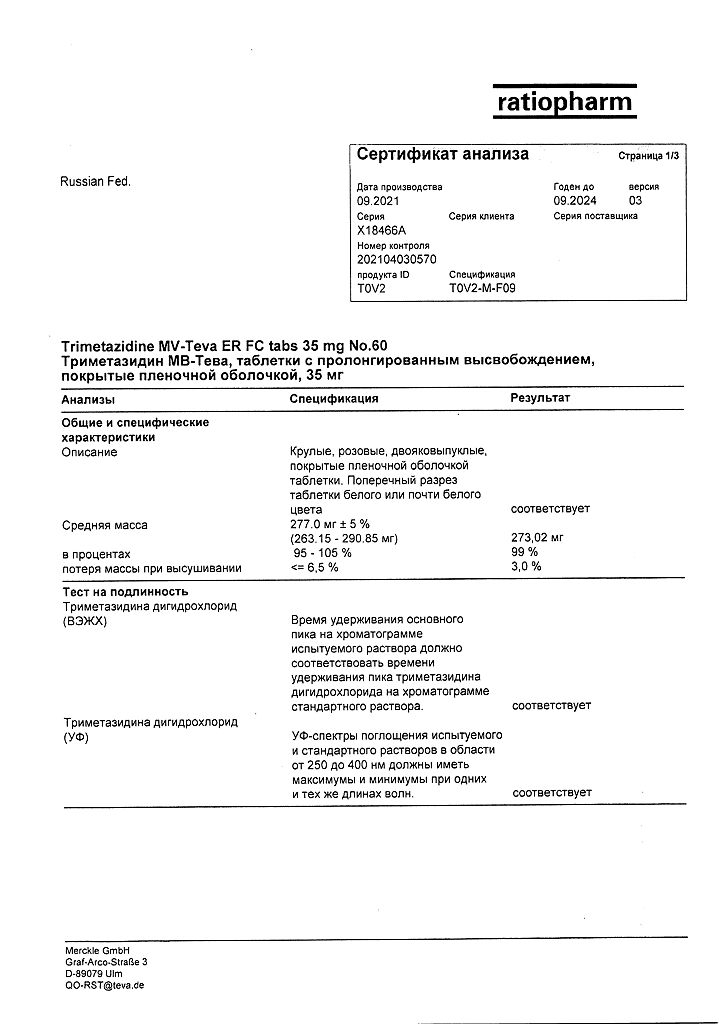
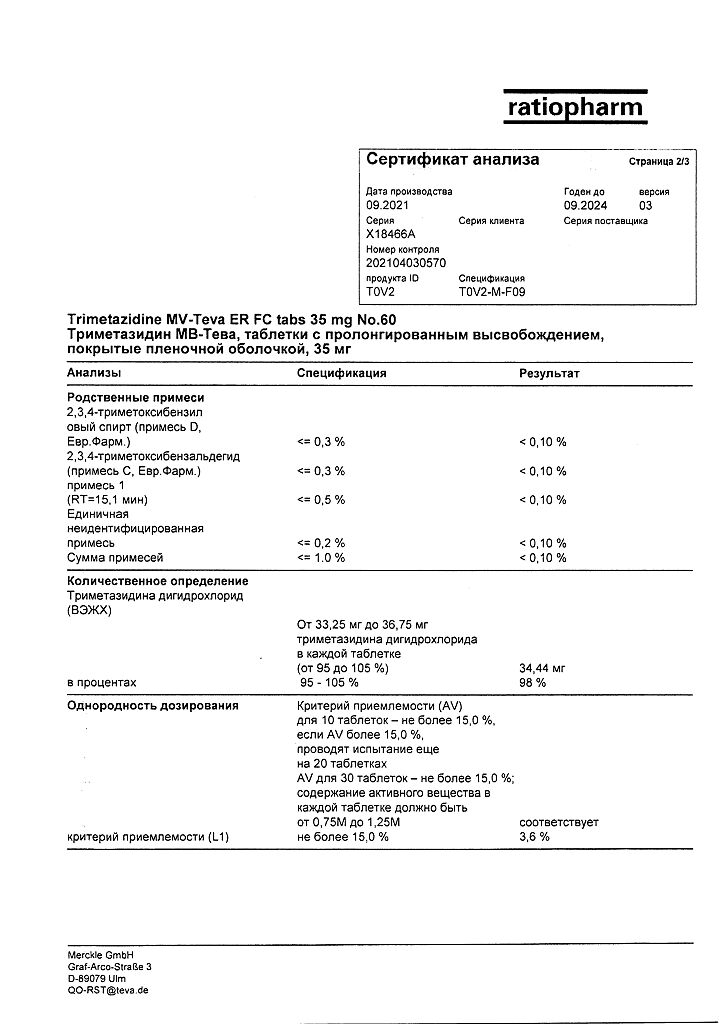
1 tablet contains: active ingredient trimetazidine dihydrochloride 35.00 mg; excipients (core): hypromellose 90.00 mg, calcium hydrogen phosphate dihydrate 141.00 mg, magnesium stearate 3.00 mg, colloidal silicon dioxide 1.00 mg; excipients (shell): water gloss pink* 7.00 mg.
*- hypromellose 60.00%, stearic acid 5.00%, macrogol-6000 3.00%, glycerol 5.00%, titanium dioxide 26.75%, red iron oxide dye 0.25%.
Pregnancy
Pregnancy
There are no data on the use of trimetazidine in pregnant women. Animal studies have not revealed the presence of a teratogenic effect. The potential risk of use in pregnant women is unknown. Trimetazidine MB-Teva is contraindicated during pregnancy.
It is not known whether trimetazidine is excreted in breast milk, therefore, if it is necessary to use the drug Trimetazidine MB-Teva during lactation, breastfeeding should be discontinued.
Reproductive toxicity studies in animals have not demonstrated the effect of trimetazidine on fertility.
Contraindications
Contraindications
hypersensitivity to any of the components of the drug;
severe renal dysfunction (creatinine clearance less than 30 ml/min);
Parkinson’s disease, symptoms of parkinsonism, tremor, restless legs syndrome and other symptoms associated with movement disorders;
pregnancy;
breastfeeding period;
children under 18 years of age (efficacy and safety have not been established).
With caution
Patients with severe hepatic impairment, moderate renal impairment and elderly patients over 75 years of age (increased trimetazidine exposure may occur).
Side Effects
Side Effects
To assess the incidence of side effects, the following criteria were used: very often (≥1/10); often (≥1/100, <1/10); uncommon (≥1/1000, <1/100); rare (≥1/10000, <1/1000); very rare (< 1/10000), frequency unknown - frequency cannot be estimated based on available data.
Blood and lymphatic system disorders: frequency unknown – agranulocytosis, thrombocytopenia, thrombocytopenic purpura.
Nervous system disorders: often – dizziness, headache; frequency unknown – symptoms of parkinsonism (tremor, akinesia, increased tone), unsteady gait, restless legs syndrome, other associated movement disorders (usually reversible after cessation of therapy), sleep disorders (insomnia, drowsiness).
Hearing and labyrinthine disorders: frequency unknown – vertigo.
Cardiac disorders: rarely – palpitations, extrasystole, tachycardia.
Vascular disorders: rarely – arterial hypotension, orthostatic hypotension, which may be accompanied by general weakness, dizziness or loss of balance (falls), especially when taking antihypertensive drugs at the same time, “flushing” of blood to the face.
Gastrointestinal disorders: often – abdominal pain, diarrhea, dyspepsia, nausea, vomiting; frequency unknown – constipation.
Liver and biliary tract disorders: frequency unknown – hepatitis.
Skin and subcutaneous tissue disorders: often – skin rash, itching, urticaria; frequency unknown – acute generalized eczematous pustulosis, angioedema.
General disorders and disorders at the injection site: often – asthenia.
Interaction
Interaction
Cases of drug interactions have not been described.
Trimetazidine can be used simultaneously with heparin, low molecular weight heparins, indirect anticoagulant agents, drugs used for lipid metabolism disorders, acetylsalicylic acid, beta-blockers, blockers of “slow” calcium channels, cardiac glycosides.
Overdose
Overdose
No cases of drug overdose have been reported. In case of overdose, symptomatic therapy should be carried out.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25°C.
Keep out of the reach of children!
Shelf life
Shelf life
3 years.
Do not use after expiration date.
Manufacturer
Manufacturer
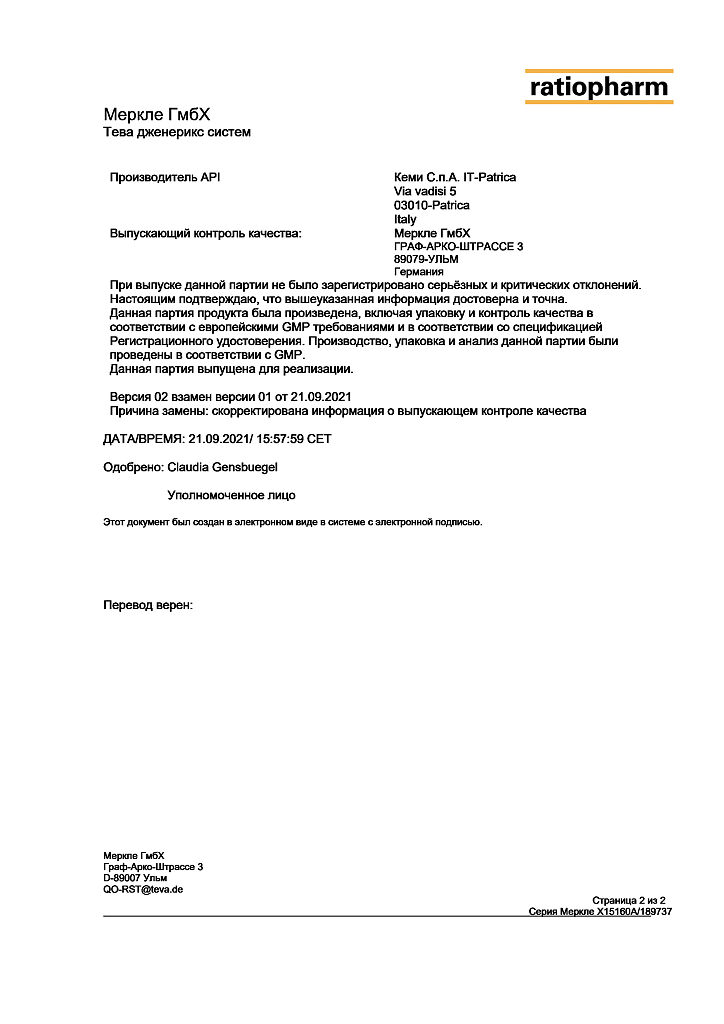
Merkle GmbH, Germany
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25°C. Keep out of reach of children! |
| Manufacturer | Merkle GmbH, Germany |
| Medication form | sustained release tablets |
| Brand | Merkle GmbH |
Related products
Buy Trimetazidine MB-Teva, 35 mg 60 pcs with delivery to USA, UK, Europe and over 120 other countries.