No products in the cart.
Trimectal CF, 35 mg 120 pcs
€34.22 €27.99
Description
Pharmacotherapeutic group Antianginal agent.
ATC code
C01EB15
Pharmacological properties
Pharmacodynamics
Mechanism of action
Trimetazidine prevents a decrease in intracellular adenosine triphosphate (ATP) concentration by maintaining cellular energy metabolism under hypoxia. Thus, the drug ensures normal functioning of membrane ion channels, transmembrane transport of potassium and sodium ions and preservation of cellular homeostasis.
Trimetazidine inhibits fatty acid oxidation through selective inhibition of the enzyme 3-ketoacyl-CoA-thiolase (3-CAT) mitochondrial long-chain fatty acid isoform, which leads to increased glucose oxidation and accelerated glucose-oxidized glycolysis, resulting in myocardial protection from ischemia. The switch of energy metabolism from fatty acid oxidation to glucose oxidation underlies the pharmacological properties of trimetazidine.
Pharmacodynamic properties:
- maintains energy metabolism of the heart and neurosensory tissues during ischemia;
- reduces the severity of intracellular acidosis and changes in transmembrane ion flow occurring during ischemia;
- reduces the size of myocardial damage;
- does not directly affect hemodynamic parameters.
In patients with angina pectoris, trimetazidine:
- increases coronary reserve, thereby delaying the onset of exercise-induced ischemia from day 15 of therapy;
- limits exercise-induced blood pressure (BP) fluctuations without significant changes in heart rate;
- significantly reduces the frequency of angina attacks and the need for short-acting nitroglycerin;
- improves left ventricular contractile function in patients with ischemic dysfunction.
The results of clinical studies have confirmed the efficacy and safety of trimetazidine in patients with stable angina pectoris both in monotherapy and in combination therapy when other antianginal drugs have insufficient effect.
In a study involving 426 patients with stable angina pectoris (TRIMPOL-II), the addition of trimetazidine (60 mg/day) to therapy with metoprolol 100 mg/day (50 mg twice daily) for 12 weeks statistically significantly improved exercise test scores and clinical symptoms compared to placebo: total duration of exercise tests, total time to exercise, time to development of ST-segment depression by 1 mm, time to development of an angina attack, number of angina attacks per week, and consumption of short-acting nitrates per week, with no hemodynamic changes.
In a study involving 223 patients with stable angina (Sellier), the addition of trimetazidine at a dose of 35 mg (2 times daily) to therapy with atenolol at 50 mg (once daily) for 8 weeks resulted in an increase in time to development of ST-segment ischemic depression by 1 mm on loading tests in a subgroup of patients compared with placebo. A significant difference was also shown for the time to development of angina attacks. No significant differences were found between groups for other secondary endpoints (total duration of exercise tests, total loading time, and clinical endpoints).
In a study involving 1962 patients with stable angina (Vasco), trimetazidine (70 mg/day and 140 mg/day) was added to therapy with atenolol 50 mg/day compared with placebo. In the general population, including both asymptomatic and symptomatic patients with angina, trimetazidine showed no benefit on ergometric and clinical endpoints. However, in a retrospective analysis in a subgroup of patients with symptomatic angina, trimetazidine (140 mg) significantly improved overall exercise test time and time to angina attack.
Pharmacokinetics
Extraction
. After oral administration, trimetazidine is rapidly absorbed and reaches maximum plasma concentration in approximately 5 hours.
After 24 hours, the plasma concentration remains at a level greater than 75% of the concentration determined after 11 hours.
The equilibrium state is reached after 60 hours. Food intake does not affect the bioavailability of trimetazidine.
Distribution
. The volume of distribution is 4.8 l/kg, which indicates good distribution of trimetazidine in tissues (the degree of binding to blood plasma proteins is quite low, about 16% in vitro).
Elimation
Trimetazidine is excreted mainly by the kidneys, mainly unchanged.
The elimination half-life in young healthy volunteers is about 7 h, in patients over 65 years of age it is about 12 h.
The renal clearance of trimetazidine directly correlates with creatinine clearance (CK),hepatic clearance decreases with patient age.
Pharmacokinetics in special patient groups<
Patients with impaired renal function
Trimetazidine exposure was on average 1.7-fold increased in patients with moderate renal impairment (CKD 30-60 mL/min) and on average 3.1-fold increased in patients with severe renal impairment (CKD less than 30 mL/min) compared with healthy volunteers with normal renal function.
No differences were found regarding safety in this patient population compared to the general population.
Elderly Patients
A special clinical study conducted in a population of elderly patients using a dose of trimetazidine MB 35 mg 2 tablets daily (2 doses) showed increased plasma levels of the drug according to a population pharmacokinetic analysis.
Elderly patients may have increased exposure to trimetazidine due to age-related decreased renal function. A special pharmacokinetic study involving elderly (75-84 years) or very elderly (≥85 years) patients showed that moderate renal impairment (CK 30-60 ml/min) increased trimetazidine exposure 1.0 and 1.3-fold, respectively, compared with younger patients (30-65 years) with moderate renal impairment.
Children and adolescents
The pharmacokinetics of trimetazidine in children and adolescents younger than 18 years have not been studied.
Indications
Indications
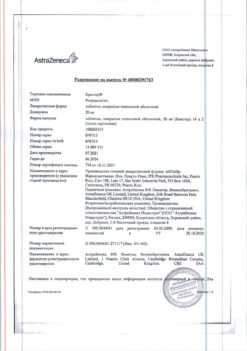
Active ingredient
Active ingredient
Composition
Composition
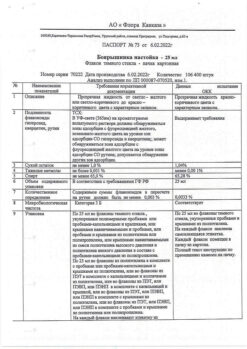
One film-coated, modified-release tablet contains:
acting substance: trimetazidine dihydrochloride – 35.0 mg;
excipients: collidone SR (polyvinyl acetate 80%, povidone 19%, sodium lauryl sulfate 0.8%, silicon dioxide 0.2%) – 137.5 mg; calcium hydrophosphate dihydrate – 73.8 mg; magnesium stearate – 2.5 mg; colloidal silicon dioxide – 1.2 mg;
film coating: [hypromellose – 4.80 mg, talc – 1.60 mg, titanium dioxide – 0.88 mg, macrogol 4000 (polyethylene glycol 4000) – 0.72 mg] or [dry film coating mixture containing hypromellose (60%), talc (20%), titanium dioxide (11%), macrogol 4000 (polyethylene glycol 4000) (9%)] – 8.0 mg.
How to take, the dosage
How to take, the dosage
The tablets should be taken whole, without chewing, with water.
Overly, 1 tablet 2 times a day, morning and evening, with meals.
The benefits of treatment should be evaluated after 3 months of taking the drug.
Trimetazidine should be discontinued if there is no improvement during this time.
The duration of treatment is according to the doctor’s recommendation.
Special patient groups
Patients with impaired renal function
. In patients with moderate renal impairment
(CKR 30-60 ml/min), the daily dose is 35 mg (1 tablet), in the morning with breakfast.
Elderly patients
In elderly patients there may be increased exposure to trimetazidine due to age-related decreased renal function (see section on Pharmacological properties). In patients with moderate renal impairment (CKD 30-60 ml/min), the recommended daily dose is 35 mg (1 tablet), in the morning with breakfast.
The dose in patients over 75 years of age should be adjusted with caution (see section “Special Precautions”).
Interaction
Interaction
Special Instructions
Special Instructions
The drug is not intended to control angina attacks and is not indicated for initial therapy of unstable angina or myocardial infarction in the pre-hospital phase or during the first days of hospitalization.
In the event of an angina attack, the degree of coronary artery damage should be reassessed and, if necessary, treatment should be adapted (drug therapy or revascularization procedure).
Trimetazidine may cause or worsen symptoms of parkinsonism (tremor, akinesia, increased tone), therefore patients, especially elderly patients, should be monitored regularly. In doubtful cases, patients should be referred to a neurologist for appropriate evaluation.
Trimetazidine should be permanently withdrawn if movement disorders, such as parkinsonian symptoms, restless legs, tremor, unsteady gait, occur.
These cases are rare, and symptoms usually disappear after discontinuation of therapy: most patients have symptoms within 4 months of discontinuation. If the parkinsonian symptoms persist longer than 4 months after discontinuation, a neurologist should be consulted.
There may be cases of falls associated with unsteady gait or arterial hypotension, especially in patients taking hypotensive medications (see section “Side effects”).
Trimetazidine should be used with caution in patients with possible increased exposure in mild renal dysfunction (see sections “Pharmacological properties” and “Administration and dosing”) and in elderly patients older than 75 years (see section “Administration and dosing”).
Influence on driving and operating ability
In clinical studies there was no effect of trimetazidine on hemodynamic parameters, but there were cases of dizziness and somnolence during post-registration use (see section “Side effects”). Side effects), which may affect the ability to drive vehicles and perform work requiring increased speed of physical and mental reactions.
Synopsis
Synopsis
Contraindications
Contraindications
With caution
Side effects
Side effects
Classification of the frequency of side effects according to the recommendations of the World Health Organization (WHO):
very often ⥠1/10;
often from ⥠1/100 to < 1/10;
infrequently from ⥠1/1000 to < 1/100;
rarely from ⥠1/10000 to < 1/1000;
very rarely < 1/10000, including individual reports;
frequency is unknown – it is not possible to determine the frequency of occurrence from the available data.
Blood and lymphatic system disorders:
frequency unknown – agranulocytosis, thrombocytopenia, thrombocytopenic purpura.
Nervous system disorders:
often – dizziness, headache;
frequency unknown – symptoms of parkinsonism (tremor, akinesia, increased tone), unsteady gait, restless legs syndrome, other related movement disorders, usually reversible after discontinuation of therapy; sleep disorders (insomnia, somnolence).
Hearing and labyrinth disorders:
frequency unknown – vertigo.
Cardiac disorders:
rarely – sensation of palpitations, extrasystole, tachycardia.
Vascular disorders:
rarely – arterial hypotension, orthostatic hypotension, which may be accompanied by general malaise, dizziness or falling, especially with the simultaneous use of hypotensive drugs, “flushes” of blood to the face.
Gastrointestinal disorders:
often – abdominal pain, diarrhea, dyspepsia, nausea, vomiting;
frequency unknown – constipation.
Liver and biliary tract disorders:
frequency unknown – hepatitis.
Dermal and subcutaneous tissue disorders:
often – skin rash, skin itching, urticaria;
frequency unknown – acute generalized exanthematous pustulosis (OGEP), angioedema.
General disorders and reactions at the site of administration:
often – asthenia.
Overdose
Overdose
Pregnancy use
Pregnancy use
Pregnancy
There are no data on the use of trimetazidine in pregnant women. Animal studies have shown no direct or indirect adverse effects on reproduction.
The use of trimetazidine during pregnancy is contraindicated.
Breastfeeding
No data on excretion of trimetazidine or its metabolites into breast milk. The risk to the newborn/infant cannot be excluded. Breast-feeding should be discontinued if it is necessary to use the drug during lactation.
Fertility
Reproductive toxicity studies have shown no effect of trimetazidine in rats of either sex.
Similarities
Similarities
Additional information
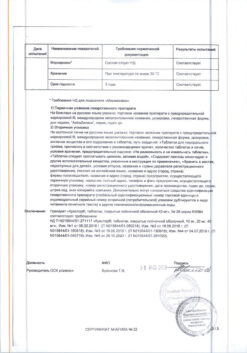
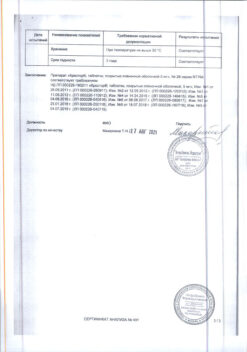
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store at the temperature not more than 25 ºC. Keep out of reach of children. |
| Manufacturer | Vertex, Russia |
| Medication form | controlled release tablets |
| Brand | Vertex |
Other forms…
Related products
Buy Trimectal CF, 35 mg 120 pcs with delivery to USA, UK, Europe and over 120 other countries.