No products in the cart.
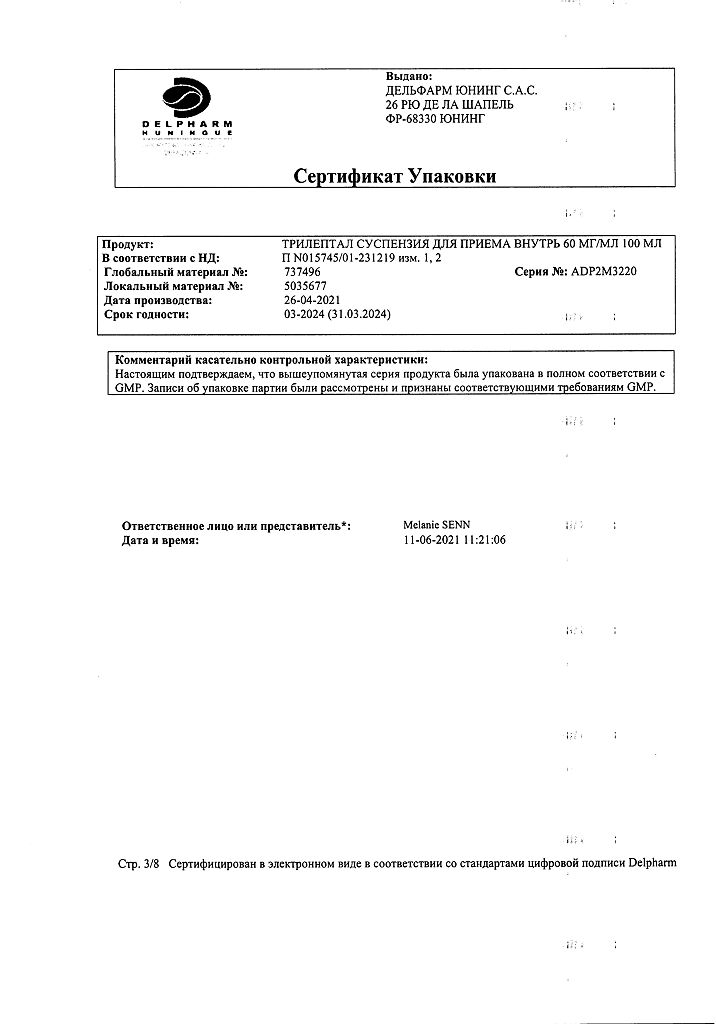
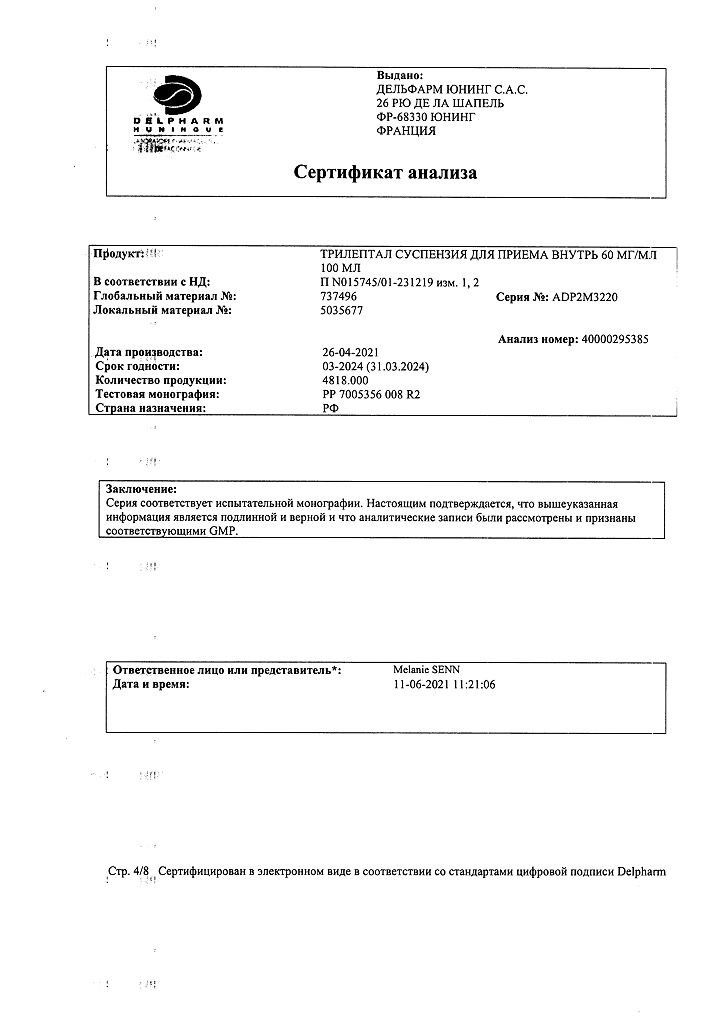
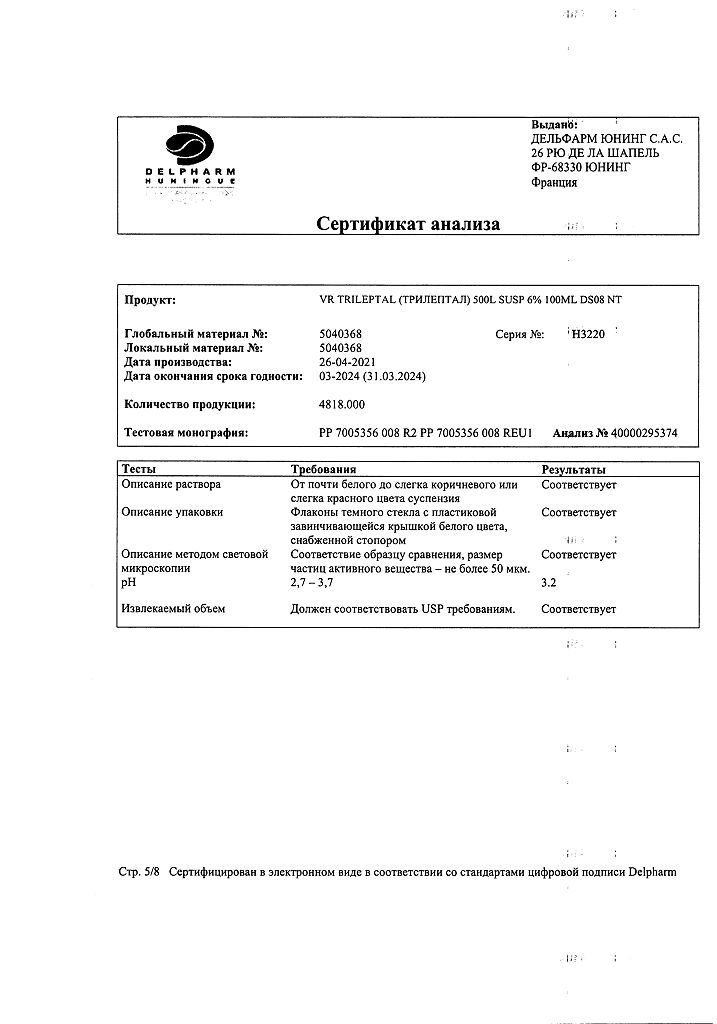
Trileptal, 60 mg/ml 100 ml
€9.78 €8.15
Description
The pharmacological activity of Trileptal® (oxcarbazepine) is primarily due to the action of its metabolite – monohydroxy derivative (MND). The mechanism of action of oxcarbazepine and its MND is mainly related to the blockade of potential-dependent sodium channels, resulting in the stabilization of overexcited neuronal membranes, inhibition of serial neuronal discharges and reduction of synaptic impulse conduction.
The realization of the anticonvulsant action of the drug is promoted by increasing the conductance of potassium ions and modulation of calcium channels activated by the high membrane potential. In the study of the drug no significant interactions with brain neuromediators or binding to receptors were observed.
In experimental studies, oxcarbazepine and MNP have been shown to have significant anticonvulsant effects.
The clinical efficacy of Trileptal® for epileptic seizures has been demonstrated both with monotherapy and when using Trileptal as part of combination therapy in children and adults.
Trileptal may be used as a substitute for other antiepileptic drugs when satisfactory therapeutic response to treatment is not achieved with the latter.
Pharmacokinetics
Intake
After oral administration oxcarbazepine in tablet form is rapidly and almost completely (>95%) is absorbed in the gastrointestinal tract and is largely metabolized to form the pharmacologically active metabolite, 10-monohydroxy derivative (MGD). After a single administration of Trileptal® in the form of coated tablets at a dose of 600 mg in healthy volunteers on an empty stomach, the average Cmax in plasma MND is 31.5 μmol/L, the average time to reach it (Tmax ) is about 5 hours.
After a single administration of the drug Trileptal® in suspension form at a dose of 600 mg in healthy volunteers on an empty stomach, the average Cmax of IHL in plasma is 24.9 μmol/l, the average maximum time of its achievement – about 6 hours. Film-coated tablets and oral suspension are bioequivalent, as the geometric mean ratio of Cmax and AUC of MND when using a single dose of oxcabazepine in tablet form and in suspension form and in equilibrium was in the range of 0.85 to 1.06 (90% confidence interval).
Pharmacokinetic studies have shown that 2% of unchanged oxcarbazepine and 70% of MGP are detected in plasma; the remainder is due to secondary metabolites that are rapidly eliminated from plasma.
Eating does not affect the rate and degree of absorption of oxcarbazepine.
Binding to plasma proteins and distribution
The apparent Vd of MND is 49 l. Approximately 40% of MND is bound to plasma proteins, mainly to albumin. In the therapeutic range the degree of binding is independent of the drug concentration in serum. Oxcarbazepine and MNP do not bind to α1-acid glycoprotein.
Metabolism
Occarbazepine is rapidly metabolized by hepatic cytosolic enzymes to the pharmacologically active metabolite MND, which accounts for the pharmacological effect of the drug. MND undergoes further conjugation with glucuronic acid. Minor amounts of MND (about 4% of the dose) are oxidized to form an inactive metabolite (10,11-dihydroxy derivative (DHD)).
Elevation
Occarbazepine is excreted mainly as metabolites, mainly by the kidneys. More than 95% of the dose is excreted by the kidneys as metabolites, less than 1% – unchanged. About 4% of the dose is excreted with feces. Approximately 80% of the dose is excreted as MND, both as glucuronides (49%) and as unchanged MND (27%); inactive DGP is about 3%, oxcarbazepine conjugates are about 13% of the dose. About 4% of the dose is excreted with the feces.
Occarbazepine is rapidly excreted from plasma, the apparent T1/2 is 1.3 to 2.3 h. In contrast to oxcarbazepine, the apparent T1/2 of MHP averages 9.3±1.8 h.
The Css of MGP in plasma is reached by 2-3 days when Trileptal® is taken 2 times/day. In equilibrium, the pharmacokinetic parameters of MND are linear and dose-dependent in the range of daily doses of 300 mg-2400 mg.
Pharmacokinetics in Special Clinical Cases
Children
The weight-adjusted clearance of MND decreases in children with increasing age and body weight, approaching that of adults. Weight-adjusted clearance in children aged 1 month to 4 years is on average 93% higher than in adults. Thus, it is expected that the AUC of IHL in children of this age group is half that of adults when using the same doses (when adjusted by body weight). Weight-adjusted clearance in children aged 4 to 12 years is on average 43% higher than in adults. Estimated AUC of IHL in children of this age group is 2/3 of that in adults when using the same doses (when adjusted by body weight). It is assumed that in children aged 13 years and older due to weight gain, MND clearance adjusted by body weight corresponds to MND clearance in adults.
Pregnant patients
A number of physiological changes occur in the body during pregnancy that can lead to a gradual decrease in plasma IHL levels during this period.
Elderly patients
After administration of Trileptal® once (at a dose of 300 mg) and again (at a dose of 600 mg/day) in older volunteers aged 60-82 years Cmax and AUC values for IHL were 30-60% higher compared to the same values in younger volunteers (18-32 years old), which is associated with age-related CK decrease.
Paired
No differences in pharmacokinetic parameters were observed by sex in childhood, adulthood, or old age.
Patients with hepatic impairment
Pharmacokinetic parameters and metabolism of oxcarbazepine and MGP after a single oral dose of 900 mg were evaluated in healthy volunteers and in patients with hepatic impairment. Mild to moderate hepatic dysfunction does not affect pharmacokinetic parameters of oxcarbazepine and MND. Pharmacokinetics in severe hepatic impairment have not been studied.
Patients with impaired renal function
There is a linear dependence of renal clearance of MND on CK. In patients with impaired renal function (CKR less than 30 ml/min) after a single administration of 300 mg oxcarbazepine the T1/2 MGP is increased by 60-90% (up to 16-19 h) and AUC is increased 2-fold.
Indications
Indications
Simple and complex partial epileptic seizures with or without secondary generalization in adults and children aged 1 month and older.
Generalized tonic-clonic epileptic seizures in adults and children aged 2 years and older.
Pharmacological effect
Pharmacological effect
The pharmacological activity of the drug Trileptal® (oxcarbazepine) is primarily due to the action of its metabolite – a monohydroxy derivative (MHD). The very mechanism of action of oxcarbazepine and its MGP is associated mainly with the blockade of voltage-dependent sodium channels, resulting in the stabilization of overexcited neuronal membranes, inhibition of the occurrence of serial neuronal discharges and a decrease in synaptic conduction of impulses.
The implementation of the anticonvulsant effect of the drug is facilitated by an increase in the conductivity of potassium ions and modulation of calcium channels activated by high membrane potential. When studying the drug, no significant interactions with brain neurotransmitters or binding to receptors were observed.
Experimental studies have shown that oxcarbazepine and MGP have a pronounced anticonvulsant effect.
Clinical effectiveness
The effectiveness of Trileptal® in epileptic seizures has been demonstrated both in monotherapy and when Trileptal is used as part of combination therapy in children and adults.
The drug Trileptal can be used to replace other antiepileptic drugs in cases where the use of the latter does not achieve a satisfactory therapeutic response to treatment.
Pharmacokinetics
Suction
After oral administration, oxcarbazepine in tablet form is quickly and almost completely (>95%) absorbed into the gastrointestinal tract and is largely metabolized to form a pharmacologically active metabolite, the 10-monohydroxy derivative (MHD). After a single dose of Trileptal® in the form of film-coated tablets at a dose of 600 mg by healthy volunteers on an empty stomach, the average Cmax in the blood plasma of the MGP is 31.5 µmol/l, the average time to achieve it (Tmax) is about 5 hours.
After a single dose of Trileptal® in the form of a suspension at a dose of 600 mg by healthy volunteers on an empty stomach, the average Cmax of MHP in blood plasma is 24.9 µmol/l, the average maximum time to achieve it is about 6 hours. Film-coated tablets and oral suspension are bioequivalent, since the geometric mean ratio of Cmax and AUC of MHP when using a single dose for oxabazepine tablets and suspension and at steady state ranged from 0.85 to 1.06 (90% confidence interval).
Pharmacokinetic studies have shown that 2% of unchanged oxcarbazepine and 70% of MGP are determined in the blood plasma; the rest is secondary metabolites that are quickly cleared from the blood plasma.
Food intake does not affect the rate and extent of absorption of oxcarbazepine.
Plasma protein binding and distribution
The apparent Vd of the IHL is 49 l. Approximately 40% of MHD is bound to plasma proteins, mainly albumin. In the therapeutic range, the degree of binding does not depend on the concentration of the drug in the blood serum. Oxcarbazepine and MGP do not bind to α1-acid glycoprotein.
Metabolism
Oxcarbazepine is rapidly metabolized by cytosolic liver enzymes to the pharmacologically active metabolite MGP, which determines the pharmacological effect of the drug. MPG undergoes further conjugation with glucuronic acid. Minor amounts of MHP (about 4% of the dose) are oxidized to form an inactive metabolite (10,11-dihydroxy derivative (DHP)).
Removal
Oxcarbazepine is excreted from the body mainly in the form of metabolites, mainly by the kidneys. More than 95% of the dose is excreted by the kidneys in the form of metabolites, less than 1% – unchanged. About 4% of the dose is excreted in the feces. Approximately 80% of the dose is excreted as MGP, both as glucuronides (49%) and unchanged MGP (27%); inactive DHP makes up about 3%, oxcarbazepine conjugates make up about 13% of the dose. About 4% of the dose is excreted in the feces.
Oxcarbazepine is rapidly cleared from blood plasma, the apparent T1/2 is 1.3 – 2.3 hours. In contrast to oxcarbazepine, the apparent T1/2 of MGP is on average 9.3±1.8 hours.
Css MGP in blood plasma is achieved on days 2-3 when taking the drug Trileptal® 2 times a day. At steady state, the pharmacokinetic parameters of MHD are linear and dose-dependent in the range of daily doses of 300 mg-2400 mg.
Pharmacokinetics in special clinical situations
Children
The clearance of MHD, adjusted for body weight, decreases in children with increasing age and body weight, approaching the clearance of adults. Weight-adjusted clearance in children aged 1 month to 4 years is on average 93% higher than in adults. Thus, it is assumed that the AUC of MHD in children of this age group is expected to be 2 times less than that in adults when using the same doses (when adjusted for body weight). Weight-adjusted clearance in children aged 4 to 12 years is on average 43% higher than in adults. The estimated AUC of MHD in children of this age group is 2/3 of that in adults when using the same doses (when adjusted for body weight). It is assumed that in children aged 13 years and older, due to increased body weight, the weight-adjusted clearance of MHD is similar to the clearance of MHD in adults.
Pregnant patients
During pregnancy, a number of physiological changes occur in the body, which can lead to a gradual decrease in the level of MHD in the blood plasma during this period.
Elderly patients
After taking the drug Trileptal® once (at a dose of 300 mg) and repeatedly (at a dose of 600 mg/day) in elderly volunteers aged 60-82 years, Cmax and AUC values for MHD were 30-60% higher compared with the same indicators in young volunteers (18-32 years), which is associated with an age-related decrease in CC.
Floor
There were no differences in pharmacokinetic parameters depending on gender in childhood, adulthood or the elderly.
Patients with liver dysfunction
The pharmacokinetic parameters and metabolism of oxcarbazepine and MHD after a single oral dose of 900 mg were assessed in healthy volunteers and in patients with impaired liver function. Mild and moderate liver dysfunction does not affect the pharmacokinetic parameters of oxcarbazepine and MHD. Pharmacokinetics in severe liver dysfunction have not been studied.
Patients with impaired renal function
There is a linear relationship between the renal clearance of MHD and CC. In patients with impaired renal function (creatinine clearance less than 30 ml/min), after a single dose of 300 mg of oxcarbazepine, T1/2 MLP increases by 60-90% (up to 16-19 hours), and AUC increases by 2 times.
Special instructions
Special instructions
There are reports of a risk of worsening the course of epileptic seizures when using the drug Trileptal®. An increased risk of worsening seizures has been observed, mainly in children, but can also occur in adults. If, while using the drug Trileptal®, there is a worsening of the course of epileptic seizures, the use of the drug should be discontinued.
Hypersensitivity reactions
When using the drug Trileptal® in clinical practice, in isolated cases (post-marketing reports), the development of immediate type hypersensitivity reactions (type I), including rash, itching, urticaria, angioedema and anaphylactic reactions, was observed. Hypersensitivity reactions can cause the development of disorders of the skin, liver, blood and lymphatic system and other organs, both individually and as part of a systemic reaction. Angioedema and anaphylactic reactions affecting the larynx, vocal folds (glottis area), tongue, lips, and eyelids developed both during the first and repeated doses of the drug Trileptal®. If immediate hypersensitivity develops, Trileptal® should be discontinued immediately and alternative therapy should be prescribed.
The drug should be used with caution in patients with known hypersensitivity to carbamazepine, because in this group of patients, in approximately 25-30% of cases, hypersensitivity reactions to oxcarbazepine may develop. In patients who do not have a history of hypersensitivity to carbamazepine, it is also possible to develop hypersensitivity reactions to the drug, including multiple organ disorders. If signs and symptoms of hypersensitivity reactions occur, Trileptal® should be discontinued immediately.
Hyponatremia
Hyponatremia (serum sodium less than 125 mmol/l) was observed in 2.7% of patients receiving Trileptal®, which was usually not accompanied by clinical manifestations and did not require adjustment of therapy. The sodium content is normalized upon discontinuation (dose reduction) of the drug Trileptal® or conservative treatment (restriction of fluid intake). In patients with a history of impaired renal function and low serum sodium levels (for example, in patients with syndrome of inappropriate antidiuretic hormone secretion), or in patients receiving concomitant treatment with drugs that promote sodium excretion from the body (diuretics, drugs that affect the secretion of antidiuretic hormone), serum sodium levels should be determined before starting therapy with Trileptal®. In the future, serum sodium levels should be monitored 2 weeks after the start of therapy and then monthly for 3 months or as needed. Particular attention should be paid to these risk factors in elderly patients. If it is necessary to use diuretics and other drugs that reduce serum sodium levels in patients receiving therapy with Trileptal®, the same recommendations should be followed. If clinical symptoms of hyponatremia appear, the sodium content in the blood serum should be determined. For other patients, serum sodium levels can be determined during routine blood tests.
It is necessary to monitor body weight in all patients with heart failure to promptly diagnose fluid retention. If fluid retention occurs or as symptoms of heart failure progress, serum sodium levels should be determined. If hyponatremia occurs, the amount of fluid consumed should be limited. Because When using oxcarbazepine, cardiac conduction disturbances may occur in very rare cases; careful monitoring of patients with previous conduction disturbances (atrioventricular block, arrhythmia) receiving Trileptal® is necessary.
Hematological changes
According to post-marketing reports, when treated with Trileptal®, patients in very rare cases experienced the development of agranulocytosis, aplastic anemia and pancytopenia. Given the low incidence of agranulocytosis, aplastic anemia and pancytopenia, as well as associated factors (for example, concomitant use of other medications, the presence of concomitant diseases), a cause-and-effect relationship between the development of these adverse events and the use of the drug cannot be established. If symptoms of severe suppression of bone marrow hematopoiesis develop, it is necessary to consider discontinuing the drug.
Suicidal thoughts and behavior
Episodes of suicidal behavior and suicidal thoughts have been reported in patients receiving anticonvulsants. The results of a meta-analysis of randomized placebo-controlled trials showed a small increase in the risk of developing suicidal behavior in patients receiving anticonvulsants. The mechanism for increasing the risk of suicide in this category of patients has not been established. Therefore, at all stages of treatment, careful monitoring of patients receiving treatment with the drug is necessary. Patients and medical personnel should be warned about the risk of suicidal thoughts and episodes in patients receiving therapy with Trileptal®.
Dermatological reactions
When using the drug Trileptal®, the development of serious dermatological reactions, such as Stevens-Johnson syndrome, toxic epidermal necrolysis (Lyell’s syndrome), exudative erythema multiforme, has been very rarely reported. Patients with the above dermatological reactions may require hospitalization due to the development of life-threatening conditions; very rarely lethal outcomes are possible. When using the drug Trileptal®, dermatological reactions were observed in both children and adults, and developed on average 19 days after starting the drug. There are isolated reports of cases of recurrence of serious skin reactions when taking Trileptal® is resumed. If skin reactions develop while using the drug Trileptal®, you should consider discontinuing the drug and using another antiepileptic drug.
Correlation with HLA-B*1502
There is considerable evidence to support the role of human leukocyte antigen (HLA) alleles in the development of serious skin reactions in patients predisposed to such conditions. Due to the similarity in the chemical structure of oxcarbamazepine and carbamazepine, there is a possibility of developing Stevens-Johnson syndrome and Lyell’s syndrome in patients with the HLA-B*1502 allele in the genome taking oxcarbazepine.
In patients of Chinese and Thai nationality, there was a clear connection between the development of Stevens-Johnson syndrome and Lyell’s syndrome when using carbamazepine and the presence of the human leukocyte antigen HLA-B*1502 allele in their genome.
The frequency of occurrence of this allele in patients of Chinese nationality is 2-12%, in Thai patients – about 8%, among some groups of the Malaysian population – more than 15%. The prevalence of the HLA-B*1502 allele in Korea and India is 2% and 6%, respectively. The prevalence of this allele in people of Caucasian, Negroid races, Latin Americans, Indians and Japanese is insignificant (
These allele frequencies represent the percentage of chromosomes in specific populations that carry the allele. This means that the percentage of patients carrying a copy of the allele on at least one of their two chromosomes is almost twice the frequency of the allele. Thus, the percentage of patients who may be at risk is almost twice the allele frequency.
When using the drug Trileptal® in possible carriers of the HLA-B*1502 allele, it is recommended to carry out genotyping for this allele. The drug should be used in carriers of this allele only if the expected benefit from therapy outweighs the possible risk. The presence of this allele in people of Chinese nationality taking other antiepileptic drugs increases the risk of developing severe dermatological reactions. In patients with the HLA-B*1502 allele, it is necessary to avoid the use of drugs that lead to the development of Stevens-Johnson syndrome or Lyell’s syndrome, with possible replacement with alternative drugs. Genotyping for the HLA-B*1502 allele before using Trileptal® is not necessary in patients belonging to populations with a low frequency of occurrence of this allele, as well as in patients already receiving therapy with this drug, since severe skin reactions in most cases were observed in the first months of treatment (regardless of the presence of HLA-B*1502).
Correlation with HLA-B*3101
The presence of the HLA-A*3101 allele may be a risk factor for the development of severe skin lesions (Stevens-Johnson syndrome, Lyell’s syndrome, drug rash with eosinophilia and systemic manifestations, acute generalized exanthematous pustulosis and macular nodular rash) when using carbamazepine. The frequency of occurrence of the HLA-A*3101 allele of the human leukocyte antigen (HLA) gene may differ among different ethnic groups: about 2-5% in the European population, about 10% in the Japanese, and about 6.7% in the Western European population, depending on the geographic region. The allele frequency is less than 5% in the populations of Australia, Asia, Africa and North America, with exceptions ranging from 5% to 12%. A frequency of more than 15% has been found in some ethnic groups of South America (Argentina and Brazil), indigenous people of North America (Navajo and Sioux tribes, in Mexico – Sanora Seri), South India (Tamil Nadu), and 10-15% among other indigenous inhabitants of these regions.
These allele frequencies represent the percentage of chromosomes in specific populations that carry the allele. This means that the percentage of patients carrying a copy of the allele on at least one of their two chromosomes is almost twice the frequency of the allele. Thus, the percentage of patients who may be at risk is almost twice the allele frequency.
There is no sufficient basis to recommend genotyping for this allele in patients before starting oxcarbazepine therapy. For patients already receiving therapy with Trileptal®, genotyping for this allele is not recommended, since skin reactions in most cases were observed in the first months of drug use (regardless of the presence of HLA-A*3101).
However, the results of genotyping should not affect the degree of control of the patient’s condition and the doctor’s alertness regarding severe skin reactions. The development of severe skin lesions is possible in patients negative for these alleles. Also, in many cases, in patients positive for the HLA-B*1502 or HLA-A*3101 alleles, the development of severe skin syndromes was not observed when using the drug Trilertal®.
When genotyping for the HLA-B*1502 allele, preference should be given to methods with high resolution. The test is considered positive if at least one of the alleles is detected, negative if no allele is detected. The same recommendations should be followed when genotyping for the HLA-A*3101 allele. The influence of other factors, such as the dose of anticonvulsants, patient compliance, concomitant therapy with other drugs, concomitant diseases, or the level of control of dermatological reactions, on the incidence and prevalence of severe skin reactions has not been established.
Liver dysfunction
There are reports of very rare cases of hepatitis, which in most cases resolved safely. If hepatitis is suspected, discontinuation of the drug should be considered.
Hypothyroidism
Hypothyroidism is an extremely rare adverse event with oxcabazepine. Considering the influence of thyroid hormones on the development of children, in this category of patients, especially under the age of two, it is recommended to determine the concentration of thyroid hormones before starting drug therapy, and also to monitor this indicator during the use of the drug Trileptal®.
Simultaneous use of oral contraceptives
Women of childbearing age taking oral contraceptives concomitantly with Trileptal should be warned about the possible decrease in the effectiveness of oral contraceptives. For this category of patients receiving Trileptal®, additional use of non-hormonal methods of contraception is recommended.
Withdrawal syndrome
As with other antiepileptic drugs, abrupt cessation of therapy with Trilertal should be avoided due to the risk of increased frequency of seizures.
Persons taking alcohol during therapy with Trileptal® should be warned of a possible increase in sedative effect.
The drug Trileptal® in the form of an oral suspension contains ethanol in an amount of less than 100 mg per dose. The suspension also contains parabens, which may cause allergic reactions (possibly delayed).
The oral suspension contains sorbitol, therefore Trileptal® in suspension form should not be used in patients with hereditary impaired fructose tolerance.
Influence on the performance of potentially hazardous activities that require special attention and quick reactions
Due to the possibility of developing such undesirable effects as dizziness, drowsiness, ataxia, diplopia, blurred vision, visual disturbances, hyponatremia, and depression of consciousness or other disorders of the central nervous system during the use of the drug Trileptal®, especially at the beginning of treatment or during dose selection, patients should be careful when driving vehicles or operating machinery during the period of use of the drug.
If the described adverse events occur, you should refrain from performing these activities.
Active ingredient
Active ingredient
Oxcarbazepine
Composition
Composition
1 ml
oxcarbazepine
60 mg
Excipients:
propyl parahydroxybenzoate – 0.3 mg,
sodium saccharinate – 0.5 mg,
sorbic acid – 0.5 mg,
macrogol 400 stearate – 1 mg,
methyl parahydroxybenzoate – 1.2 mg,
ascorbic acid – 10 mg,
dispersible cellulose (microcrystalline cellulose and sodium carmellose) – 15 mg,
yellow plum-lemon aroma 39K020 (is a solution containing 36% ethanol and 16% propylene glycol) – 2.5 mg,
distilled propylene glycol – 25 mg,
sorbitol 70% liquid – 250 mg,
purified water – 717 mg.
Pregnancy
Pregnancy
Children of patients with epilepsy are more often than others predisposed to developmental disorders, incl. birth defects.
Experience with the use of Trileptal® during pregnancy is limited. Available reports indicate a possible connection between taking the drug during pregnancy and the development of congenital malformations (CMD). The most common malformations in children whose mothers received Trileptal® therapy during pregnancy were: atrial septal defect, atrioventricular septal defect, cleft palate and upper lip, Down syndrome, hip dysplasia (both unilateral and bilateral), tuberous sclerosis and ear malformations.
According to the North American Pregnancy Registry, the incidence of gross malformations, defined as structural abnormalities requiring surgical, medical or cosmetic correction, diagnosed within 12 weeks after birth was 2.0% (95% confidence interval 0.6 to 5.1%) among pregnant women taking oxcarbazepine monotherapy in the first trimester. Compared with pregnant women who were not treated with any antiepileptic drugs during pregnancy, the relative risk of developing malformations in children is 1.6 with a 95% confidence interval of 0.46 to 5.7.
Patients of childbearing age should use reliable methods of contraception during therapy with Trileptal® (optimally, intrauterine contraceptives), since when used simultaneously with oral contraceptives containing ethinyl estradiol or levonorgestrel, the effectiveness of these drugs may be reduced.
If the patient is planning a pregnancy or pregnancy is diagnosed while using the drug, as well as if the question arises about using the drug Trileptal® during pregnancy, it is necessary to carefully compare the expected benefits of therapy and the possible risk to the fetus, especially in the first trimester of pregnancy.
During pregnancy, the minimum effective dose of the drug should be used. If clinical efficacy is sufficient in women of childbearing age, Trileptal® should be used in monotherapy.
The patient should be warned about possible developmental disorders of the fetus and the need for antenatal diagnosis.
During pregnancy, effective antiepileptic treatment should not be interrupted, since progression of the disease may have a negative effect on the mother and fetus. It is known that folic acid deficiency develops during pregnancy. Antiepileptic drugs can enhance this deficiency, which is one of the possible causes of fetal development disorders, therefore additional intake of folic acid is recommended.
When using the drug during pregnancy, it is necessary to take into account that the physiological changes that occur in the body during pregnancy can lead to a gradual decrease in the level of 10-monohydroxy derivatives (MHD) in the blood plasma. To achieve maximum control over the symptoms of the disease in pregnant patients, it is necessary to regularly evaluate the clinical effect of the drug and determine the concentration of MHD in the blood plasma.
Determination of the level of MHD in blood plasma is also recommended in the postpartum period, especially if the dose of the drug was increased during pregnancy.
There are reports that the use of antiepileptic drugs during pregnancy may lead to increased bleeding in newborns. As a precautionary measure, the use of vitamin K1 is recommended in the last few weeks of pregnancy, as well as in newborns whose mothers received Trileptal®.
Oxcarbazepine and MGP penetrate the placental barrier. Oxcarbazepine and MGP are excreted in breast milk. The concentration ratio in milk and plasma was 0.5 for both substances. Since the effect on newborns of oxcarbazepine and MHD supplied through breast milk is unknown, Trileptal® should not be used during breastfeeding.
Use in children under 1 month of age
There is no data on the safety and effectiveness of Trileptal® in children under 1 month of age.
Effect on fertility
There is no data on the effect of the drug on fertility in humans. Animal studies have shown no effects of oxcarbazepine and MGP on fertility in either sex at daily doses of 150 and 450 mg/kg, respectively. When using maximum doses of MHD in females, however, there was a disruption of the astral cycle, a decrease in the number of luteal bodies, a decrease in the number of implantations and the number of living embryos.
Contraindications
Contraindications
children up to 1 month;
hypersensitivity to oxcarbazepine or any other components of the drug.
The drug should be prescribed with caution to patients with known hypersensitivity to carbamazepine, because In this group of patients, approximately 25–30% of cases may develop hypersensitivity reactions to oxcarbazepine. In patients who do not have a history of hypersensitivity to carbamazepine, it is also possible to develop hypersensitivity reactions to the drug, including multiple organ disorders.
The use of Trileptal® in patients with impaired liver function has not been studied, so the drug should be used with caution in this category of patients.
Use for liver dysfunction
No dosage adjustment is required in patients with mild to moderate liver dysfunction. Caution must be exercised when used in patients with severe liver dysfunction.
Use for renal impairment
For patients with impaired renal function (creatinine clearance less than 30 ml/min), the recommended initial dose is 300 mg/day; The dose should be increased slowly, at intervals of at least 1 week, until the desired therapeutic response is achieved. Careful monitoring of patients is necessary during dose selection.
Use in children
Application is possible according to the dosage regimen.
Contraindicated in children under 1 month of age.
Use in elderly patients
Special adjustment of the dosage regimen in this category of patients is necessary if renal function is impaired (creatinine clearance less than 30 ml/min). If there is a risk of developing hyponaremia, careful monitoring of sodium levels in the blood plasma is necessary.
Side Effects
Side Effects
The most frequently reported adverse reactions were: drowsiness, headache, dizziness, diplopia, nausea, vomiting, fatigue (more than 10% of patients).
Clinical studies have shown that undesirable effects are usually mild or moderate, transient in nature and observed mainly at the beginning of therapy.
The data below summarizes the information on adverse reactions (ARs) recorded during clinical trials, as well as data on the safety profile of the drug obtained during its use in clinical practice. HPs are grouped according to the MedDRA classification of organs and organ systems, and are listed in descending order of importance.
Criteria for assessing the incidence of adverse events: very often (≥1/10), often (≥1/100,
From the blood and lymphatic system: infrequently – leukopenia; very rarely – suppression of bone marrow hematopoiesis, agranulocytosis, aplastic anemia, neutropenia, pancytopenia, thrombocytopenia.
From the immune system: very rarely – anaphylactic reactions, hypersensitivity reactions (including multiple organ disorders), which are characterized by phenomena such as rash and increased body temperature. Possible damage to the circulatory and lymphatic systems (eosinophilia, thrombocytopenia, leukopenia, lymphadenopathy, splenomegaly), liver (hepatitis, changes in liver function indicators), damage to muscles and joints (myalgia, swelling in the joints, arthralgia), nervous system (hepatic encephalopathy), kidneys (renal failure, interstitial nephritis, proteinuria), lungs (pulmonary edema, bronchospasm, bronchial asthma, interstitial inflammation, shortness of breath), angioedema.
From the endocrine system: very rarely – hypothyroidism.
Metabolism and nutrition: often – hyponatremia (more often observed in patients aged >65 years); very rarely – clinically significant hyponatremia (sodium concentration). This condition can lead to the development of such manifestations and symptoms as seizures, encephalopathy, decreased level of consciousness, confusion, visual disturbances (including blurred vision), hypothyroidism, vomiting, nausea, folic acid deficiency.
From the mental side: often – agitation (including nervousness), emotional lability, confusion, depression, apathy.
From the nervous system: very often – drowsiness (22.5%), headache (14.6%), dizziness (22.6%); often – ataxia, tremor, nystagmus, impaired attention, amnesia.
From the organ of vision: very often – diplopia (13.9%); often – blurred vision, visual disturbances.
From the organ of hearing and labyrinthine disorders: often – systemic dizziness.
From the heart: very rarely – AV block, arrhythmias.
From the side of blood vessels: very rarely – arterial hypertension.
From the digestive system: very often – vomiting (11.1%), nausea (14.1%); often – diarrhea, abdominal pain, constipation; very rarely – pancreatitis.
From the liver and biliary tract: very rarely – hepatitis.
From the skin and subcutaneous tissues: often – rash, alopecia, acne; infrequently – urticaria; very rarely Stevens-Johnson syndrome, toxic epidermal necrolysis (drug-induced Lyell’s syndrome), angioedema, erythema multiforme, systemic lupus erythematosus.
General disorders and disorders at the injection site: very often – feeling of fatigue (12%); often – asthenia.
Laboratory and instrumental data: infrequently – increased activity of liver enzymes, alkaline phosphatase; very rarely – increased activity of amylase and lipase.
In clinical studies conducted in children aged 1 month to 4 years, somnolence was most commonly observed (in 11% of patients). With a frequency >1%-
Adverse reactions identified in the post-marketing period based on anecdotal reports and cases described in the literature.
Since data on adverse reactions in the post-marketing period were obtained from voluntary reports from a population of unknown size, it is impossible to estimate the frequency of their occurrence (frequency unknown). Adverse reactions are classified by organ system; within each organ system, adverse reactions are arranged in decreasing order of severity.
From the side of the track and subcutaneous tissues
Drug rash with eosinophilia and systemic manifestations, acute generalized exanthematous pustulosis.
From the musculoskeletal and connective tissue side
There have been reports of decreased bone mineral density, osteopenia, osteoporosis and fractures in patients receiving long-term treatment with Trileptal®. The mechanism of the effect of oxcarbazepine on bone metabolism is not clear.
Metabolism and nutrition
Syndrome of inappropriate secretion of antidiuretic hormone, manifested by lethargy, nausea, dizziness, decreased plasma osmolality, vomiting, headache, confusion and other symptoms of the nervous system.
Injuries, intoxications and complications of manipulations
Fall.
From the nervous system
Speech disorders (including dysarthria), especially during dose selection.
Interaction
Interaction
Enzyme inhibition
Oxcarbazepine and its pharmacologically active metabolite MGP are inhibitors of cytochrome CYP2C19. Thus, the simultaneous use of Trileptal® in high doses and drugs that are metabolized with the participation of the CYP2C19 isoenzyme (for example, phenobarbital, phenytoin) may lead to their interaction. Some patients may require a dose reduction of drugs that are CYP2C19 substrates. Oxcarbazepine and MHD have been shown to have little or no interaction with the following microsomal isoenzymes: CYP1A2, CYP2A6, CYP2C9, CYP2D9, CYP2E1, CYP4A4 and CYP4C11.
Enzyme induction
Being weak inducers of cytochromes CYP3A4 and CYP3A5, they reduce plasma concentrations of drugs metabolized by these enzymes: dihydropyridine calcium antagonists, oral contraceptives and antiepileptic drugs (for example, carbamazepine). When used simultaneously with Trileptal®, it is also possible to reduce the plasma concentrations of other drugs that are substrates of the CYP3A4 and CYP3A5 isoenzymes (for example, drugs from the group of immunosuppressants – cyclosporine).
Because oxcarbazepine and MGP are weak inducers of uridine diphosphate-glucuronyl transferase in vitro, they are unlikely to have a clinically significant effect in vivo on the metabolism of drugs excreted as glucuronic acid conjugates (e.g., valproic acid and lamotrigine). But, taking into account even the weak inducing ability of oxcarbazepine and MGP, it may be necessary to increase the doses of concomitantly used drugs that are metabolized with the participation of the CYP3A4 isoenzyme or uridine diphosphate-glucuronyl transferase. If Trileptal® is discontinued, it may be necessary to reduce the dose of these drugs based on clinical and laboratory monitoring. In vitro studies have confirmed the weak inducing ability of oxcarbazepine and MGP against isoenzymes of the CYP2B and CYP3A4 enzyme subsystems. The inducing effect of oxcarbazepine and MHD on other CYP isoenzymes is unknown.
Antiepileptic drugs (AEDs)
Possible interactions between Trileptal® and other antiepileptic drugs were assessed in clinical studies. The effects of these interactions on AUC and trough concentration Cmin are summarized in the table:
PEP
Effect of the drug Trileptal® on PEP
Cmin
Influence of AEDs on MPG
AUC
Carbamazepine
0-22% decrease (30% increase in carbamazepine-10,11-epoxide)
40% reduction
Clobazam
Not studied
Does not affect
Felbamate
Not studied
Does not affect
Phenobarbital
14-15% increase
30-31% reduction
Phenytoin
0-40% increase
29-35% reduction
Valproic acid
Does not affect
0-18% reduction
The concentration of phenytoin in the blood plasma increases to 40% with simultaneous administration of the drug Trileptal® at a dose of 1200 mg/day or higher. Therefore, when using the drug Trileptal® in the above doses, it may be necessary to reduce the dose of phenytoin.
The increase in the concentration of phenobarbital in the blood plasma when used simultaneously with the drug Trileptal® is insignificant (15%).
With the simultaneous use of strong cytochrome P450 inducers (i.e., carbamazepine, phenytoin and phenobarbital), the concentration of MHD in the blood plasma decreases (by 29-40%). Thus, the concentration of MHD in the blood plasma should be monitored and, if necessary, the dose of the drug should be adjusted when oxcarbazepine is used simultaneously with one or more of the above drugs.
The drug Trileptal® did not exhibit any autoinduction phenomena.
Hormonal contraceptives
The interaction of the drug Trileptal® with the components of oral contraceptives: ethinyl estradiol and levonorgestrel has been proven. Their average AUC values decreased by 48-52% and 32-52%, respectively. There have been no studies of the interaction of Trileptal® with other oral or implantable contraceptives. Thus, the simultaneous use of Trileptal® and hormonal contraceptives may lead to a decrease in the effectiveness of the latter, and therefore additional use of reliable non-hormonal methods of contraception is recommended for patients receiving treatment with Trileptal®.
Calcium channel blockers
Concomitant use of Trileptal® and felodipine may result in a decrease in felodipine AUC by 28%, although plasma concentrations remain within the therapeutic range.
On the other hand, when used simultaneously with verapamil, it is possible to reduce the concentration of MHD in the blood plasma by 20%. This decrease in MPG concentration is not clinically significant.
Interaction with other drugs
Cimetidine, erythromycin, dextropropoxyphene do not affect the pharmacokinetic parameters of MGP; viloxazine has little effect on plasma MHD concentrations (MHD concentrations increase by 10% after repeated co-administration). There was no interaction with warfarin when taking either single or multiple doses of Trileptal®.
There were no interactions with warfarin, either with a single simultaneous dose or with repeated doses of Trileptal®.
Trileptal® may enhance the sedative effect of ethanol.
Overdose
Overdose
There are isolated reports of drug overdose. The maximum dose reported was approximately 48,000 mg.
Symptoms:
Water and electrolyte imbalance: hyponatremia.
From the organ of vision: diplopia, miosis, blurred vision.
From the digestive system: nausea, vomiting, hyperkinesia.
General disorders and administration site disorders: fatigue.
Laboratory and instrumental data: decreased respiratory rate, prolongation of the QTc interval.
From the nervous system: drowsiness, dizziness, ataxia, nystagmus, tremor, loss of coordination, convulsions, headache, coma, loss of consciousness, dyskinesia.
Mental disorders: aggression, agitation, confusion.
Vascular disorders: decreased blood pressure.
From the respiratory system, chest and mediastinal organs: shortness of breath.
Treatment. There is no specific antidote. Symptomatic and supportive treatment is carried out. It should be borne in mind that to reduce the absorption of oxcarbazepine, gastric lavage may be performed and activated charcoal may be prescribed. Vital functions of the body should be monitored, paying special attention to disturbances in water and electrolyte balance, cardiac conduction and disorders of the respiratory system.
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Delpharm Younging S.A.S, France
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Delpharm Uning S.A.S., France |
| Medication form | oral solution |
| Brand | Delpharm Uning S.A.S. |
Related products
Buy Trileptal, 60 mg/ml 100 ml with delivery to USA, UK, Europe and over 120 other countries.