No products in the cart.
Travapress Duo, eye drops (5 mg+0.04 mg)/ml 2.5ml
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: Antiglaucoma combined agent (synthetic prostaglandin F2-alpha analogue + beta-adrenoblocker).
ATX code: S01ED51.
Pharmacological properties
Pharmacodynamics
The drug Travapress Duo contains two active ingredients: Timolol and Travoprost. Both reduce intraocular pressure. Because of their complementary mechanisms of action, the decrease in intraocular pressure is greater with the combination than with each of the components alone.
Timolol
. Timolol is a non-selective blocker of beta-adrenoreceptors without sympathomimetic activity, has no direct depressant effect on the myocardium, has no membrane-stabilizing activity.
When used topically, it reduces intraocular pressure by reducing aqueous humor formation and slightly increasing its outflow.
Travoprost
Travoprost, an analogue of prostaglandin F2-alpha, is a highly selective agonist of prostaglandin FP receptors and reduces intraocular pressure by increasing aqueous outflow. The main mechanism of action of travoprost is associated with an increase in uveoscleral outflow. It has no significant effect on the production of aqueous humor.
The intraocular pressure decreases approximately 2 hours after drug administration, and the maximum effect is achieved after 12 hours. Significant decrease in intraocular pressure may persist for up to 24 hours after a single application of the drug.
Pharmacokinetics
Absorption and pDistribution
Travoprost and timolol are absorbed through the cornea of the eye. In the cornea there is hydrolysis of travoprost to its biologically active form, free acid travoprost. Free hervoprost acid is rapidly eliminated from plasma within one hour – plasma concentrations fall below the detection threshold of less than 0.01 ng/ml (can vary from 0.01 to 0.03 ng/ml). The maximum plasma concentration (Cmax) of timolol is 1.34 ng/ml and persists to the detection threshold for 12 h, and the time to reach the maximum concentration (Tmax) of timolol is reached within 0.69 h after topical administration. The half-life (T1/2) of timolol is 4 h after topical administration of timolol+travoprost.
Metabolism and excretion
Metabolism is the major route of elimination of travoprost and free acid travoprost. The systemic metabolic pathways parallel those of endogenous prostaglandin F2a, which are characterized by reduction of the 13-14 double bond, oxidation of the 15-hydroxyl group, and P-oxidative cleavage of the upper side chain link. Free hervoprost acid and its metabolites are mostly excreted by the kidneys. Less than 2% of hervoprost is found as free acid in the urine.
Timolol and the resulting metabolites are excreted mainly by the kidneys. About 20% of timolol is excreted unchanged, the rest is excreted as metabolites.
Indications
Indications
Reduction of elevated intraocular pressure in open-angle glaucoma and intraocular hypertension in patients resistant to monotherapy with beta-blockers or prostaglandin analogues.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Combined antiglaucoma agent (synthetic prostaglandin F2-alpha analogue + beta-blocker).
ATX code: S01ED51.
Pharmacological properties
Pharmacodynamics
Travapress Duo contains two active ingredients: timolol and travoprost. Both components reduce intraocular pressure. Due to the complementary mechanisms of their action, the decrease in intraocular pressure under the influence of the combination is more significant than with the action of each of these components separately.
Timolol
Timolol is a non-selective beta-adrenergic receptor blocker without sympathomimetic activity, does not have a direct depressive effect on the myocardium, and does not have membrane-stabilizing activity.
When applied topically, it reduces intraocular pressure by reducing the formation of aqueous humor and slightly increasing its outflow.
Travoprost
Travoprost, a prostaglandin F2-alpha analog, is a highly selective prostaglandin FP receptor agonist and reduces intraocular pressure by increasing the outflow of aqueous humor. The main mechanism of action of travoprost is associated with an increase in uveoscleral outflow. Does not have a significant effect on the production of aqueous humor.
Intraocular pressure decreases approximately 2 hours after use of the drug, and the maximum effect is achieved after 12 hours. A significant decrease in intraocular pressure can persist for 24 hours after a single use of the drug.
Pharmacokinetics
Suction and distribution
Travoprost and timolol are absorbed through the cornea of the eye. In the cornea, travoprost is hydrolyzed to its biologically active form, travoprost free acid. Travoprost free acid is rapidly cleared from plasma within one hour – the plasma concentration decreases below the detection threshold – less than 0.01 ng/ml (can vary from 0.01 to 0.03 ng/ml). The maximum concentration (Cmax) of timolol in blood plasma is 1.34 ng/ml and remains up to the detection threshold for 12 hours, and the time to reach the maximum concentration (Tmax) of timolol is achieved within 0.69 hours after topical application. The half-life (T1/2) of timolol is 4 hours after topical administration of timolol + travoprost.
Metabolism and excretion
Metabolism is the primary route of elimination of travoprost and travoprost free acid. Systemic metabolic pathways parallel those of endogenous prostaglandin F2a, which are characterized by reduction of the 13-14 double bond, oxidation of the 15-hydroxyl group and P-oxidative cleavage of the upper side chain unit. Travoprost free acid and its metabolites are primarily excreted by the kidneys. Less than 2% of travoprost is found in urine as free acid.
Timolol and the resulting metabolites are excreted primarily by the kidneys. About 20% of timolol is excreted unchanged, the rest – in the form of metabolites.
Special instructions
Special instructions
Systemic effects
Like other topical ophthalmic drugs, timolol and travoprost are absorbed into the systemic circulation.
Due to the beta-adrenergic effect of the active substance – timolol – the same adverse reactions from the cardiovascular and respiratory systems can be observed as with the use of systemic beta-blockers.
Heart disorders
In patients with cardiovascular disease (eg, coronary artery disease, Prinzmetal’s angina, heart failure) and hypotension, treatment with beta-blockers should be critically assessed and the use of other drugs should be considered. Patients with cardiovascular diseases should be assessed for signs of worsening of these diseases and the development of HP. Since beta blockers have a negative effect on conduction time, they should be used with caution in patients with first degree atrioventricular block.
Vascular disorders
In patients with severe peripheral circulatory disorders (including severe forms of Raynaud’s disease or Raynaud’s syndrome), treatment should be carried out with caution.
Breathing disorders
The patient’s condition should be monitored before and during timolol therapy. After the use of certain ophthalmic drugs from the group of beta-blockers, cases of respiratory reactions, including death from bronchospasm, have been described in patients with bronchial asthma.
In patients with mild to moderate COPD, the combination of timolol + travoprost should be used with caution and only if the expected benefit outweighs the possible risk.
Hypoglycemia/diabetes mellitus
Beta blockers should be used with caution in patients prone to developing spontaneous hypoglycemia, as well as in patients with unstable diabetes mellitus, since beta blockers may mask the signs and symptoms of hypoglycemia.
Hyperthyroidism
Beta blockers may mask the symptoms of hyperthyroidism.
Muscle weakness
Beta blockers may potentiate muscle weakness, consistent with certain symptoms of myasthenia gravis (eg, diplopia, ptosis, and generalized muscle weakness).
Corneal diseases
Beta blockers for ophthalmic use may cause dry eyes. In patients with corneal diseases, the drug should be used with caution.
Choroidal detachment of the eye
In patients who used drugs that suppress the production of aqueous humor (for example, timolol and acetazolamide), cases of choroidal detachment were observed after fistulizing operations of the organ of vision.
Other beta blockers
When timolol is used in patients already taking systemic beta-blockers, the effect on intraocular pressure or other known effects of systemic beta-blockers may be enhanced. The response to therapy in such patients should be carefully monitored. The use of two beta-blockers for local use is not recommended (see section “Interaction with other drugs”).
Skin contact
Prostaglandins and prostaglandin analogs are biologically active substances that can be absorbed through the skin. Women during pregnancy, as well as women planning pregnancy, should take appropriate precautions to prevent direct contact of the contents of the bottle with the skin. If a significant portion of the contents of the bottle does come into contact with the skin (which is unlikely), the area of skin on which the drug has come into contact should be immediately washed with water.
Anaphylactic reactions
The use of timolol in patients with atopy or a history of severe anaphylactic reactions to various allergens may precipitate more severe reactions in response to allergen management. Such patients may respond poorly to normal doses of epinephrine (adrenaline) to relieve anaphylactic reactions.
Ophthalmic effects
When using travoprost, there may be a gradual change in eye color due to an increase in the number of melanosomes (pigment granules) in melanocytes. Before starting treatment, the patient should be informed about the possibility of irreversible changes in eye color. Treatment of only one eye can lead to irreversible heterochromia. The long-term effect on melanocytes and the consequences of this influence are currently unknown. The change in iris color occurs slowly and may not be noticeable for months or years. Discoloration is more common in patients with mixed iris colors (blue-brown, gray-brown, yellow-brown and green-brown), and a similar effect was observed in patients with brown eyes. In typical cases, brown pigmentation around the pupil extends concentrically to the periphery of the iris, causing the entire iris or parts thereof to become browner. At the end of therapy, there is no further accumulation of brown pigment in the iris.
Darkening of the skin of the periorbital area and/or eyelids has been reported with the use of travoprost.
Travoprost may gradually change the condition of the eyelashes in the treated eye(s); These changes include changes in length, thickness, pigmentation and/or number of eyelashes. The mechanism of these changes is currently unknown.
During treatment with prostaglandin F2α analogues, the development of macular edema was noted.
Travoprost should be used with caution in patients with neovascular, angle-closure, narrow-angle, pigmentary and congenital glaucoma; open-angle glaucoma with pseudophakia, pseudoexfoliative glaucoma, inflammatory diseases of the organ of vision, aphakia, pseudophakia with rupture of the posterior capsule of the lens or anterior chamber intraocular lens, as well as in patients with risk factors for the development of macular edema, iritis, uveitis.
When using prostaglandin analogues, changes in the periorbital area and eyelids were noted. Deepening of the eyelid sulcus was noted only in studies in monkeys, while clinical studies in humans did not provide data on this effect, which allowed it to be considered species-specific.
Anesthesia for surgical interventions
Ophthalmic drugs from the group of beta-blockers can suppress the beta-agonist effects, for example, of epinephrine. The anesthesiologist should be informed if the patient is using timolol. Excipients
Travapress Duo eye drops contain propylene glycol, which may cause skin irritation.
Travapress Duo eye drops contain macrogol glyceryl hydroxystearate, which can cause skin reactions.
Contact lenses
The patient should be warned about the need to remove contact lenses before instilling Travapress Duo and not to put them on for 15 minutes afterward.
Impact on the ability to drive vehicles and machinery
Temporary blurred vision or other visual disturbances after using the drug may affect the ability to drive vehicles or operate machinery. If blurred vision is noted after instillation, the patient must wait until clear vision is restored before operating vehicles or machinery.
Active ingredient
Active ingredient
Timolol, Travoprost
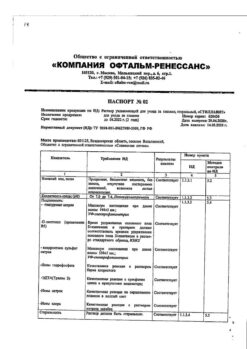
Composition
Composition
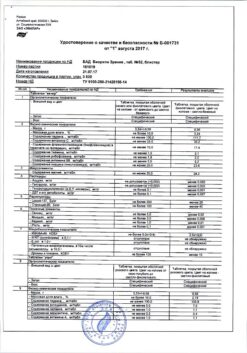
Composition per 1 ml of the drug:
active ingredients: travoprost 0.040 mg, timolol 5,000 mg (in the form of timolol maleate 6,800 mg);
excipients: boric acid 3,000 mg, sodium chloride 2,500 mg, mannitol 3,000 mg, macrogol glyceryl hydroxystearate (Kollifor RH40) 1,000 mg, propylene glycol 7,500 mg, 1 M hydrochloric acid solution or 1 M sodium hydroxide solution to pH 6.8 ± 0.1, purified water to 1.0 ml.
Pregnancy
Pregnancy
Pregnancy
Travoprost has a negative pharmacological effect both on the course of pregnancy and on the fetus or newborn. There are no or limited data on the use of the combination of travoprost + timolol or its individual components in pregnant women.
Animal studies of travoprost have shown reproductive toxicity. Epidemiological studies with oral use of beta-blockers have not revealed effects associated with malformations, but indicate a risk of intrauterine growth retardation. In addition, when systemic beta-blockers were used by the mother prior to delivery, signs and symptoms of beta-blockade (eg, bradycardia, hypotension, respiratory depression, and hypoglycemia) were observed in the neonate.
The use of Travapress Duo is contraindicated during pregnancy. If Travapress Duo is used before birth, the condition of the newborn should be carefully monitored in the first days of life.
Breastfeeding period
It is not known whether travoprost eye drop dosage form passes into breast milk in humans. Animal studies have shown that travoprost and its metabolites pass into breast milk. Timolol passes into breast milk, potentially causing serious adverse reactions (ADRs) in a breastfed infant. However, when timolol is used in therapeutic doses, it is unlikely that sufficient amounts will be present in breast milk to develop symptoms of beta-adrenergic receptor blockade in a child.
The use of the drug Travapress Duo during breastfeeding is contraindicated.
Fertility
There is no information on the effect of timolol + travoprost eye drops on fertility in humans. Animal studies have shown no effect on fertility of travoprost or timolol at doses greater than 250 times the maximum recommended dose for topical ophthalmic use in humans.
Women with preserved reproductive potential/contraception
Travapress Duo is not recommended for use by women with preserved reproductive potential, unless they are using reliable contraception.
Contraindications
Contraindications
Hypersensitivity to the active substances or to any of the excipients.
Hypersensitivity to other beta-blockers.
Reactive airway disease, including bronchial asthma (including a history), as well as severe chronic obstructive pulmonary disease (COPD).
Sinus bradycardia, sick sinus syndrome, including sinoatrial block, second or third degree atrioventricular block without a pacemaker.
Decompensated chronic heart failure.
Cardiogenic shock.
Severe allergic rhinitis.
Corneal dystrophy.
Pregnancy and breastfeeding period.
Children under 18 years of age (safety and effectiveness have not been established).
With caution
Neovascular, angle-closure, narrow-angle glaucoma; pigmentary and congenital glaucoma; open-angle glaucoma with pseudophakia; pseudoexfoliative glaucoma; acute inflammatory diseases of the organ of vision; in patients with pseudophakia due to rupture of the posterior capsule of the lens or in patients with an anterior chamber intraocular lens; in patients at risk of developing cystoid macular edema, iritis, uveitis; in patients with atopy or with a history of severe anaphylactic reactions to various allergens; in patients with labile diabetes mellitus and a tendency to hypoglycemia; in patients with hyperthyroidism, Prinzmetal’s angina; in patients planning to undergo surgery.
Side Effects
Side Effects
General information about the safety profile of timolol + travoprost
In clinical trials involving 2170 patients treated with the fixed combination timolol + travoprost, the most common adverse event was conjunctival injection (12.0%).
Adverse Event Data
The following adverse events were observed during clinical trials and post-registration use of the fixed combination timolol + travoprost and are classified according to the following gradation of the frequency of occurrence of adverse events: very often (≥1/10), often (from ≥1/100 to <1/10), infrequently (from ≥1/1,000 to <1/100), rarely (from ≥1/10,000 up to <1/1,000), very rare (<1/10,000), frequency unknown (estimate based on available data is not possible). Within each group, adverse events are listed in descending order of severity.
Immune system disorders: uncommon hypersensitivity
Mental disorders rarely nervousness: frequency unknown depression
Nervous system disorders: uncommon dizziness, headache, frequency unknown stroke, fainting, paresthesia
Violations of the organ of vision very often conjunctival hyperemia:
often punctate keratitis, eye pain, visual disturbances, blurred vision, dry eye syndrome, eye itching, eye discomfort, eye irritation
uncommon keratitis, iritis, conjunctivitis, inflammation of the anterior chamber of the eye, blepharitis, photophobia (photophobia), decreased visual acuity, asthenopia, eye swelling, lacrimation, eyelid erythema, increased eyelash growth, allergic eye phenomena, conjunctival edema, eyelid edema
rarely corneal erosion, meibomitis, subconjunctival hemorrhage, crusting on the eyelid margins, trichiasis, distichiasis
frequency unknown macular edema, ptosis, corneal pathology
Cardiac disorders: uncommon: bradycardia:
rarely arrhythmia, heart rhythm disturbances
frequency unknown heart failure, tachycardia, chest pain, palpitations
Vascular disorders: uncommon: arterial hypertension, arterial hypotension: frequency unknown; peripheral edema
Disorders of the respiratory system, chest and mediastinal organs:
uncommon: shortness of breath, postnasal drip
rarely dysphonia, bronchospasm, cough, throat irritation, pharyngolaryngeal pain, nasal discomfort
frequency unknown bronchial asthma
Gastrointestinal disorders: frequency unknown dysgeusia
Disorders of the hepatobiliary system: rarely, increased activity of alanine aminotransferase (ALT), aspartate aminotransferase (AST)
Disorders of the skin and subcutaneous tissues:
uncommon contact dermatitis, hypertrichosis
rarely urticaria, skin discoloration, alopecia, periocular skin hyperpigmentation
frequency unknown skin rash
Musculoskeletal and connective tissue disorders: rarely pain in the extremities
Renal and urinary tract disorders: rarely, chromaturia
General disorders and disorders at the injection site: rarely thirst, increased fatigue
Additional adverse events that were observed during therapy with monocomponents separately may be observed during therapy with the fixed combination of timolol + travoprost.
Travoprost
Visual disorders: uveitis, conjunctival disorders, conjunctival folliculosis, iris hyperpigmentation
Disorders of the skin and subcutaneous tissues peeling of the skin
Timolol
Like other drugs for topical use in ophthalmology, timolol is absorbed into the systemic circulation. This may cause the same range of adverse effects as with oral beta blockers.
Interaction
Interaction
No interaction studies have been conducted with other drugs.
During combined use of cytochrome CYP2D6 inhibitors (for example, quinidine, fluoxetine, paroxetine) and timolol, cases of increased systemic action of beta-blockers (for example, decreased heart rate, depression) were observed.
When eye drops containing timolol are used together with blockers of “slow” calcium channels, guanethidine, beta-blockers, antiarrhythmic drugs (including amiodarone), parasympathomimetics and cardiac glycosides, additive effects may develop, leading to the development of arterial hypotension and (or) severe bradycardia.
With the combined use of beta-blockers and clonidine, “rebound” arterial hypertension may develop after abrupt withdrawal of the latter.
Beta blockers may decrease the response to epinephrine (adrenaline), used to treat anaphylactic reactions. Particular caution should be observed in patients with a history of indications of atopy and anaphylaxis (see section “Special Instructions”).
The simultaneous use of two local beta-blockers or two local prostaglandin analogues is not recommended!
There have been reports of the development of mydriasis (dilation of the pupils) with the combined use of ophthalmic beta-blockers and epinephrine (adrenaline).
Beta-blockers may enhance the effect of hypoglycemic drugs.
Overdose
Overdose
In case of overdose with local ophthalmic use, no toxic effects on the organ of vision are expected. Immediate rinsing of eyes with water is recommended.
Symptoms
If accidentally ingested, symptoms of overdose resulting from systemic exposure to beta-blockers may include bradycardia, hypotension, heart failure and bronchospasm, and cardiac arrest.
Treatment
Treatment in case of accidental ingestion of timolol + travoprost eye drops should include symptomatic and supportive therapy. Hemodialysis is ineffective in removing timolol.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
After opening the bottle, the drops should be used within 4 weeks.
Do not use after expiration date.
Manufacturer
Manufacturer
K.O.Rompharm Company S.R.L., Romania
Additional information
| Shelf life | 3 years. After opening the bottle the drops should be used within 4 weeks. Do not use after the expiration date. |
|---|---|
| Conditions of storage | At a temperature not higher than 25 ° C. Keep out of reach of children. |
| Manufacturer | C.O.Rompharm Company S.R.L., Romania |
| Medication form | eye drops |
| Brand | C.O.Rompharm Company S.R.L. |
Other forms…
Related products
Buy Travapress Duo, eye drops (5 mg+0.04 mg)/ml 2.5ml with delivery to USA, UK, Europe and over 120 other countries.